Arthritis and A Total Knee Replacement 101 (I just found out that a Garrett pin pointer can detect metals in the body)
TKR Update After 6 years Going Strong Out Of Nowhere I Get a Severe Knee Infection
November 18, 2013 I had to have my knee replaced again because of an infection. The doctor has no clue how I got it, I haven't been sick, no cuts that were infected, no bad teeth, he told me less than 2% of people get and infection like I had for no reason. This makes the 4 th replacement, first 2 done wrong the 3rd was going well, 6 years go by and I get an infection.
I had no warning, my husband and I were out metal detecting and it was windy, so I thought my knee was getting sore because of over doing it. We stopped at a restaurant afterwards and ate. I got out of the car and my knee was hurting worse. While eating I started to get chilled and thought oh great getting the flu. I then get up to use the restroom and almost couldn't walk. Within three hours I was unable to walk on that knee. The next day I went to the emergency room and they did a blood test and it came back that sed rates elevated. I was told to go to my doctor and then he set up surgery.
I was on vancomycin from November 19 till December 26th and had home health coming to my house. My knee is doing better and I know from experience that it will take time for my knee to get back to where it was.
I have a very good orthopedic surgeon, the first surgeon is no longer in Illinois, but from what we hear he is still practicing. The last we heard he is in Mississippi.
There are many good orthopedic surgeons in Peoria Illinois things would have been so much easier if I had known this in the beginning.
Garrett pin pointer can detect metal in your body
We do a lot of metal detecting and I have a Garrett pin pointer that I use. There have been many times I have set it off, I forget that I have it on and it starts sounding off, I had it next to my knee replacement.
One day I got curious and took it up and down my leg to find out how far the stem went, it goes further than I thought.
I then decided to see if it would pick up the metal in my neck from a previous surgery and it did.
What a handy little device it great for metal detecting and has other purposes.
Three time TKR Total Knee Replacement Survivor
You may have come to a point in life that your doctor has told you that your only option left is to get a total knee replacement. This is a decision not to make lightly.
I'm not a doctor or an expert, but I do know from experience about a TKR, since I've had it done three times on the same knee.
Your doctor will do ever thing possible to relieve your pain, before doing surgery.
Surgery will be your you last resort.
Doctors may prescribe anti-inflammatory drugs, to relieve inflammation, such as Celebrex, Ibuprofen, Naproxen, etc. They may also prescribe medication to go along with the anti-inflammatory drug. I was prescribed each one of the drugs above, trying to find one that would work for me. I was not able to get much relief out of any of these drugs.
My left knee was worse than my right knee. Going up or down any kind of stairs was getting quite difficult. I could hear my knees make popping noises with ever step. I could feel the grinding, from just rocking in a rocking chair.
Cortisone Shot
My doctor said another option was to take cortisone shots. You can only get these shots ever three months. So I took him up on the ideal and got the cortisone shot. When I first started the shots, they seemed to give some relief. But as the arthritis progressed, the pain was worse and the shots would only last a couple of days.
Since the cortisone shots were no longer giving any kind of relief, my doctor said arthroscopic surgery could be done. He said this is a way of cleaning up the arthritis, making a smoother surface for the knee to glide better. I was told I had a 50/50 chance this working. Since nothing previous was working for me any more I went ahead with the surgery on Nov 18, 2004. This procedure was done as an outpatient.
Right Knee Left Knee Arthroscopy
Operative Report
11/18/2004
Preoperative Diagnosis:
Internal derangement right knee.
Internal derangement left knee.
Postoperative Diagnosis:
Right Knee chondromalacia patella, right knee tear lateral menisus.
Left knee chondromalacia patella with condylar defect medial condyle and tear lateral menicus.
Procedure Performed:
Right knee arthroscopy, arthroscopic partial lateral meniscectomy and chondroplastic shaving patella.
Left Knee arthroscopy, arthroscopic chondropic shaving patella, partial lateral meniscectomy and chondroplastic shaving medial femoral condyle.
Indication: Patient has significant pain in both knees for prolonged period of time. She failed outpatient care including Cortisone injections. She is admitted for diagnostic bilateral arthroscopy. Her x-rays show some mild subluxation patella but otherwise normal.
Arthroscopy
- Arthroscopy
Arthroscopy is a surgical procedure that allows your doctor to look at the inside of a joint in your body through a thin viewing instrument called an arthroscope.
Right Knee Arthroscopy
Patient was taken to the Operating Room and adequate anesthesia obtained. Attention was focused on the right knee. The right knee was then prepped and draped in the usual manner. At this time a lateral parapatellar tendon stab was made and the arthroscope was inserted. A medial parapetellar tendon stab was made and the nerve hook was inserted. The knee was inspected. The medial joint showed some softening at the epicondyle but no frank abrasion. The medial meniscus was intact. Attention was focused laterally. The lateral meniscus showed some tearing of the anterior horn at the anterior third. The torn portion was explored. It appeared to be a degenerative type tear. At this time using combination of hand and power instruments, the torn portion was removed. There was some softening of the epicondyle cartilage of the lateral compartment with no frank abrasion. The anterior horn was inspected and found to be stable. I should mention that the reaming portion of the lateral meniscus and the entire medial meniscus was probed and found to be stable and the patellofemoral joint. There was chondromalacia patella. This was mostly at the lateral facet involved the bulk lateral facet. This was mostly Grade III. At this time using the axillary portal, this was shaved until smooth. After this was accomplished, both gutters were inspected along with the superior patellar pouch and this was within normal limits. The knee was then thoroughly irrigated. The portal was closed with staples. A sterile dressing was applied after the knee was injected with Depo-Medrol.
Left Knee Arthroscopy
Attention was focused on the left knee. The left knee was then prepped and draped in the usual manner. Same portals were utilized. Inspection was done and found some softening of the articular cartilage medially diffusely. There was a condylar fracture of the articular cartilage on the posterior medials aspect. This was approximately 5 mm x 7 mm. The loose piece of articular cartilage was then removed. The medial meniscus itself was intact. Attention was focused on the intercondylar notch. The anterior cruciate ligament was intact. There was noted to be an indentical tear of the anterior lateral meniscus as the right knee. This is shaved until smooth. The remaing portion of the lateral meniscus is within normal limits. Again there was softening or the articular cartilage laterally, but no frank abrasion. Attention was focused to the femoral joint. There was significant chondromalacia patella. There were two areas exposed subchondral bone approximately 1 cm x 1 cm in size. At this time the loose pieces of the articular cartilage was then shaved until smooth. The medial facet showed softening but no frank abrasion. Both gutters were inspected along with superior patellar pouch and this was within normal limits. The knee was then thoroughly irrigated. The portals were closed with staples. Sterile dressing was applied. Patient went to the Recovery Room in good condition.
Right Knee Arthroscopic Success
The surgery was a success on the right knee.
Left Knee Arthroscopic Failure
The left knee was said to be bone on bone. A few months after the arthroscopic surgery, my left knee was getting much worse, than before.
Synovics
So my doctor wanted me to try synovics to see if I could get some kind of relief. Synovics is supposed to be like grease. The relief did not lasted for about 2 months and you can only get this shot every 6 months.
TKR replacement needed
My doctor told me since nothing tried, was working, that I would need a TKR. I've talked to People who have had a TKR and most of them are very happy with their results. Some were saying they were walking great in just a couple of days. I even had one person say they went dancing the next week.
So on July 29, 2005 I was scheduled for a total knee replacement.
This was my first TKR picture
TKR Operative Report:
7/29/2005
Preoperative Diagnosis: Degenerative Joint Disease, Left knee.
Postoperative Diagnosis: Degenerative Joint Disease, Left Knee.
Operation: Left Total Knee Replacement, Zimmer Type.
Anesthesia: Attempted Epidural, General..
Indication: The patient had pain in her left knee. Previous arthroscopy showed degenerative joint disease. The patient has failed conservative management including the arthroscopy, therapy, cortisone, and Synvisc injections. She is admitted for total knee replacement. The risks, benefits, and alternatives have been discussed including the fact that given her age prosthesis would probably not last lifetime.
Procedure: The patient was taken to the operating room and placed in the supine position. After an adequate level of general anesthesia was obtained, the left leg was then prepped and draped in the usual manner. There was noted to be about 10- to 15- degree flexion contracture. At this time, a medial arthrotomy was carried out. The patella subluxed laterally, it was osteotomized. Attention was focused to the distal femur. The femur was entered; it was then osteotomized in 6 degrees of valgus. Attention focused to the tibia. The tibia was not osteotomized. Attention focused back to the femur. The femur was measured for size and a size D femoral component gave the best fit. In the appropriate rotation, the anterior and posterior condyles were chamfered and then removed. The notch for the patella and the focused back to the tibia.. Utilizing the instruments for the MIS tibial guide, the tibia was measured and a #3 tibial baseplate gave the best fit. In the appropriate rotation, the central peg holes were created and a canal for the 45 - mm stem
Knee Replacement
At this time, the trials were inserted including the 45 - mm stem. With the 10 - mm polyethylene, the knee had a range of motion from 0 to 155 degrees. With gravity alone, the knee flexed to 130 degrees. The knee was stable in all planes. At this time, the patella was re-osteotomized. It was measured for size and a 35 -mm patellar button gave the best fit. The patellar button was inserted. The patella tracked well using the no-hands technique. At this time, the trials were removed. Mutiple drill holes were placed in the femur and tibia. The entire wound was copiously irrigated with a Water Pik and dried. All remaining osteophytes were removed. At this time, the above-mentioned components were cemented into place. The wound was then irrigated and dried. Utilizing a #3 tibial baseplate, a size D femoral component and a 35 - mm patellar button. Again a 45 - mm stem was utilized on the MIS tibial baseplate. After the cement was appropriately cured, excess cement was removed. Hemostatsis was achieved using the platelet gel. The tourniquet was released. At this time, trials were again done. With the 10 - mm polyethylene insert, the knee had a range of motion from 0 to 150 degrees. The knee was stable in all planes. The patella tracked well using no-hands technique. The knee was stable in all planes. At this time, the trials were removed. The wound was again irrigated. All remaining cement and osteophytes were removed. A 10 - mm polyethylene was then inserted in the tibial baseplate and secured using the Zimmer locking mechanism. Range of motion and stability were again tested and were identical with the trials. The patella tracked well using the no-hands technique. Final hemostasis was achieved. The wound was again irrigated. The remaing portion of the platelet gel was utilized. The wound was then closed utilizing interrupted #1 Vicryl for the fascia, interrupted 3-0 Vicryl for the subcutaneous tissue, 4-0 Monocryl for the skin along with Steri-Strips and Dermabond. The patient tolerated it well and went to recovery room in good condition. Estimated blood loss was 400 ml.
Epidural Failed
The type of anesthesia that my doctor wanted me to have was an epidural with a nerve block. This did not work for me; I could still feel everything they were doing to my leg. So they up the meds in the epidural, they would stick me in the leg to see if the epidural was working. The epidural failed, so they put me to sleep. They put the Foley in while they were prepping me.
Morphine
The first day after surgery I was not allowed out of bed. For the first two days I was on Morphine for pain control.
Vicodin
Third day I was then given Vicodin to control the pain. Do not let your pain get out of control, before asking for pain medicines. Take your pain meds on schedule, you will avoid much unneeded pain.
Therapy Starts the Morning after Surgery
The morning after surgery a physical therapist came in to my room. I was then gotten out of bed, with the aid of the therapist and a walker. I then walked from the bed to a chair that was next to the bed. I was told I needed to sit in the chair for as long as I could handle it. This was a glider type chair. The therapist said the rocking motion would be a good therapy for my knee. I was told it would also help strengthen my knee, later that day I walked from the bed to the door. When I got back in bed, I was showed other exercises that I was supposed to do. The third day I was walked down the hall with a walker. My therapist then took me to where they had stairs to show me how to use the walker on stairs. I had therapy 3x a day.
Occupational Therapy
I then had an occupational therapist come into my room. She was there to educate and to show ways of bathing and dressing. I only saw the occupational therapist twice.
Release from Hospital after TKR
I could not be released from the hospital until my knee was bending to a certain point, and I was walking to my doctor's satisfaction. On August 2, 2005 I was released from the hospital. A walker was brought up to my room for me to take home. I was given instructions on how to care for my knee, I was told to keep my leg elevated and to keep ice on my knee. I was told not to put a pillow behind the knee because this could cause blood clots. I was given a prescription to for pain medication. Therapy was set up for 3x a week.
Allergic Reaction to Derma Bond
Everything was going great; except one minor thing, my knee developed a rash and started itching real bad. It turns out that I was allergic to the derma bond glue they used to close my knee during surgery.
Knee Replacement coming loose
Therapy was going great, two weeks after surgery I was walking without the aid of a walker. I was now using crutches.
Then the end of August 2005 my problems began. I had all kinds of problems, increased pain, and instability; swelling, redness; heat and I couldn't straighten my leg. I could not trust my knee at all, I would be walking and all of a sudden it would give out o
Dynasplint
Then in September my doctor then had me fitted with a device called a dynasplint. Which is to be worn at night while sleeping. This is supposed to straighten my leg. I wore this device every night till January with no luck.
Estim
In January my doctor had me wear a device called an Estim, which produced electrical current into the knee. This was supposed to help relieve the pain. This did not work.
Not pleased with Doctor
February I was still on crutches and my knee was getting worse; my knee had so much swelling and heat that my doctor thought that I had an infection. My doctor ordered test to see if my knee was infected, it was not.
He x-rayed my knee constantly to make sure everything was in place. Each time I would be told things are fine; nothing is out of place, your knee is stable and in a well fixed position.
I was told that when my year is up that he would like to do a bone scan. He said that if he did a bone scan now that it would give a false reading.
Finally in May he set up a bone scan. The bone scan showed that my knee replacement had come lose.
I was told that my knee had come loose, and that I would need to have a revision done.
So August 25, 2006 a TKR revision is done. The revision seemed to be going great for the first few weeks.
This replacement only lasted 3 weeks.
This doctor would not listen to me. I told him that something was wrong with this replacement. My therapist was even concerned. She had called him on more than one occasion with concerns.
My knee had so much swelling that my therapist thought I had a bad infection. The doctor drew fluid to check it for infection. As before there was no infection.
I asked my doctor could you do a bone scan to see if it is lose again. His reply was as before. It is to soon for a bone scan, if we did one now it would give a false reading.
I was getting really irritated with this doctor.
Second Opinion
So I started looking for a different doctor, to get a second opinion. I was told I had to stay with this doctor for at least 6 months past surgery. I could not get anybody to take my case, each place I was told the same thing.
In March after enough complaining my doctor decided to do a bone scan. As soon as I could I got a copy of the bone scan and read it. I compared it to the first scan that I had done. It said the same thing. When I went back for the results of the bone scan, my doctor told me everything is fine. He had lied to me; my knee had come lose again.
After many calls I finally found a doctor who will see me. On May 25, 2007 I see the doctor. This doctor was not at all happy with the doctor who had done my first two surgeries. I was told that my knee was lose, malrotated, misaligned, there was missing bone he had used extra cement to fill in the gap, he cracked my tibia, stretched my ligaments, the list goes on. This doctor that I'm seeing now said the first doctor knew he had made a mistake and tried to cover it up. I was told I needed to have my knee revised again.
Third Opinion
I got a third opinion to make sure I was being told the truth. The third doctor said the same thing the second doctor said.
I already had an appointment with the first doctor for June. I hadn't cancelled it yet. So I had a thought, I'll see if this doctor will tell me some more lies. Sure enough he did, he said my knee was doing just fine, that there is nothing wrong with it.
Third TKR
On July 17, 2007 I had my knee done for the third time. Believe me I was leery about the outcome. I was prepared for it to go bad again. I did have some problems, but nothing compared to the first two times. My doctor kept reassuring me things are going just fine. I was told the ligaments might never be the same. I was told that since there was so much damage done to my knee that it will take along time for it to heal. This doctor had one heck of a mess to clean up after the first doctor and did a remarkable job.
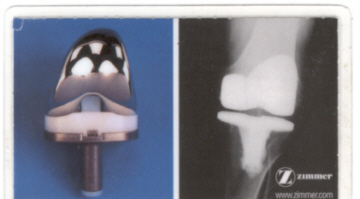
This an actual picture of my 3rd TKR
Operative Report
7/17/2007
Pre-Procedure Diagnosis: Painful, Malaligned, Unstable Left Total Knee Arthroplasty.
Post-Procedure Diagnosis: Painful, Malaligned, Unstable Left Total Knee Arthroplasty.
Procedure: Revision, Left Total Knee Arthroplast.
Anesthesia: General endotracheal.
Blood Loss: Less than 10 cc.
Drains: Orthopat and Foley catheter
Fluid Replacement: 2100 cc crystalloid.
Tourniquet Time: 114 minutes at 300 mmHg
Implants: CCK left size D femur with a straight 12 by 145 femoral stem. The size 3 tibial base plate with a straight 10 mm, 145 tibial stem. A size 17 LCCK polyethylene liner.
Specimens: Cultures and fluid for culture.
Description of Procedure: The patient was taken to the operation room, given a general anesthetic, intravenous antibiotic, a Foley catheter, and tourniquet on the left proximal thigh. All bony prominences and superficial nerves were well-padded and protected. The left lower extremity was thoroughly prepped and draped in the usual sterile fashion. Her previous midline inferior knee incision was again utilized for expose. Scar tissue was encountered consistent with previous revision surgery. I continued my dissection until the extensor mechanism and a medial parapatellar arthrotomy was performed. Some clear fluid was seen and this was aspirated and cultured. Intraoperative results would show not white blood cells or bacteria on the gram stain. Clinically, it appeared to be an aseptic
source of failure. Dissection then allowed us to further expose the knee joint. We removed an abundant amount of scar cartilage intra-articularly. Examination of the tibia grossly revealed that there was an anterior medial tibial defect with a significant amount of bone loss. The bone loss was near the tubercle region and so care was taken throughout the procedure to protect avulsion of the extensor mechanism. We initially removed the existing polyethylene liner is it entirety. We then went ahead and flexed the knee. We then in an atraumatic fashion removed the distal femoral component, preserving maximal bone stock. Any remaining cement was also removed. We then went ahead and exposed the tibia. The cemented tibial stem extension was removed in an atraumatic fashion. We removed the tibial component in its entirety along with a significant amount of cement that remained in the proximal femur. There was cement that was noted throughout the knee and it was removed carefully with mostly a bur technique to prevent injury to the bone. There was significant bony deficiency posteriorly as well. After the cement and all components were removed, we copiously irrigated all bony surfaces, removing any excess debris and derided any membranous tissue. I then went ahead and assessed my flexion and extension gaps. We initially cut the proximal tibia with a 2 mm reference with an extramedullary guide, simply to establish a proximal working surface. The bone was removed and it sized at a 3. Reaming of the tibial canal for the press-fit stem extender was then carried out. We reamed to about 11 to 12 mm range, which would allow for a press-fit 10 mm stem. We then went ahead and did a trial reduction with the tibia. When proper rotation and position was established, a nice fit was noted. I did then go ahead and work on the femoral component. Intramedullary reaming to 12 mm was carried out. Intramedullary reaming to 12 mm was then allowed to place the stem and then a fresh up cut at 5 degrees valgus made with the intramedullary alignment guide. The component was sized for a D. Rotation cut made for the CCK femur. Trial was assembled and then placed. We then did a series of trial reductions with a variety of inserts, and it was noted that the 17 gave full extension, flexion, and a nice stability throughout the range of motion. A significant amount of scar tissue was noted around the patella, and this was debrided. The patella was not damaged. It was well fixed and then left in place. Final preparations were made for the tibial and femoral components and then trials removed. Copious irrigation, cleaning, and drying of all bony surfaces was followed by mixing of three bags of cement with antibiotic and a vacuum. Components were selected, assembled, and then inserted with the cement and given adequate time for hardening and pressurization while removing any excess cement. We then irrigated one final time when the cement was hard. We selected the final polyethylene line, locked it securely into the
tibial base plate and set the screw and torqued it. I then went ahead and assessed motion and tracking which was excellent. We placed a deep drain. We closed the wound with #1 Vicryl, Inverted 2-0 Vicryl, staples for skin and a bulky bandage. All counts were correct by the nursing staff at the end of the case. She appeared to have tolerated her procedure well and was transferred to the recovery room in stable condition. Tourniquet was deflated 114 minutes and good blood flow was established distally.
Third TKR a Success
My knee is getting better with each day. I still have problems with it going out on me, because of the ligament damage. The pain is also getting better. I was told it could take up to a year, for my knee to be up to par. But since I had so many problems and surgeries that it will take longer.
The first thing I would do in preparing for a total knee replacement is:
I would make sure that it is absolutely necessary to have it done. If you don't feel comfortable with what a doctor has told you. Get a second opinion, or do research to make sure you are doing the right thing.
Research your Doctor
Do a thorough research on the doctor you are seeing or are about to see. Make sure all information you have on your doctor is accurate I thought I had a qualified surgeon and as it turns out he has had a very poor outcome of many surgeries preformed by him. If I had known everything I needed to know about this doctor. I never would have let him do surgery on me. Being in the dark as I was, I allowed this doctor to perform a total knee replacement twice on the same knee. The first came lose, because he used the wrong replacement. The second, was malrotated, misaligned, missing bone, cracked tibia, stretched ligaments, the list goes on. The third surgery was finally done correct by a different doctor. The first doctor kept telling me nothing was wrong, even though he knew different.
Malpractice
We later found out he has multiple lawsuits pending, not allowed to do surgery in 3 hospitals. I was told if I wanted to sue him to wait in line. I wished I had known then what I know now. This would have saved me thousands of dollars, and much heartache.
Information
This is a site that I found some very good information. Some of which I have related below along with my own experiences, and knowledge.
http://www.kneereplacement.com/DePuy/docs/Knee/Replacement/DuringSurgery/knee_surgery.html
Home Preparation
You will want to prepare you home before having your surgery so it will be comfortable and safe when you come home from the hospital. After all you wouldn't want to catch your walker, or crutch on a rug or cord and fall.
Choose a spot in your home that you feel comfortable, because you are going to be spending most of your time there. A great place would be the couch or a recliner. A TV tray, or table would be great to have near your couch or chair. There are many things you are going to want to have near you.
It's possible you may need to set a bed or cot in another area of your house. You may not be able to sleep in your bed. I have a waterbed, and there was no way that I was going to be able to sleep in it. I spent many weeks on the couch.
I myself used a nightstand that had a drawer, which I kept my brush and comb. I also kept the instructions from my doctor along with important phone numbers in this drawer. Under the stand I kept a garbage can.
Your doctor is not going to let you take a bath or a shower for a while. So you are going to want to have something set up to take care of your grooming needs.
I also had a pan that came from the hospital under this table, in this pan I kept the no rinse foam that I got from the hospital, along with my toothpaste and toothbrush. The no rinse foam that I had could also be used to clean my hair. There was no way I was going to be able to wash my hair in the shower or bath, for a while. I also kept a container of baby wipes for freshening up.
On top of this stand I kept a bottle of water, and my prescriptions, in doing this I was able to take my pain medication as needed. I also kept the TV remote and the phone on this stand. As you know the phone always likes to ring, when you are alone, and it's in another room. You might also want to have some reading material near you. After all it gets quite boring watching the same thing on TV, time after time.
Your flexibility and mobility are going to be limited after surgery. It took a while before I could bend my leg far enough to get it over the tub to take a shower. Grab bars are really handy to have next to the toilet or in the shower. Your knee is going to be unstable for a time, and it is nice to have something to hold onto, so you don't fall. I also had a shower brush and a long handled sponge. I couldn't bend my leg up far enough to wash my feet.
You might want to go shopping before your replacement. I bought a lot of simple foods to fix. My husband does not know how to cook. So I had to purchase foods that he could fix. There are so many things you may find that you are going to need after your surgery.
Something else I found to be quite handy, I had a basket attached to the front of my walker, for carrying things. This enabled me to do things for myself. I didn't have to ask my husband to carry from room to room for me. With my crutches I had a bag strapped to it to put things in. You learn real fast, what it is like to be handicap.
Preoperative Testing
Before you have your surgery, your doctor may order tests and may have you get a physical by your family physician to make sure you are healthy enough for the operation.
My surgeon wanted me to have a physical, blood test, EKG, and chest X-ray. Your doctor may want you to donate blood before your surgery in case you need a transfusion for surgery. As soon as you have the clearance of good health, you can then move forward with surgery.
Anesthesia
Prior to your knee replacement, your anesthesiologist will review you medical chart and discuss the appropriate type of anesthesia for you. There are two common types of anesthesia used during knee replacement surgery: General anesthesia, where you are asleep, and regional anesthesia, where you are numbed below the waist, typically with an epidural. The type of anesthesia will depend on your surgeon, your situation, and your anesthesiologists' recommendations.
Find out which type of anesthesia is going to be used. If you are feeling uncomfortable about the type of anesthesia that is going to be used, discuss it with your doctor. I had a bad experience when the doctor tried to use the epidural the first replacement. I told my doctor I was not comfortable using that type of anesthesia, my doctor then decided to use another method of anesthesia, such as general.
Knee Replacement Surgery
This is what happens during knee replacement surgery. A special instrument is used, to remove the worn surfaces at the end of the thighbone. The bone is the shaped for preparation of the new covering that is most commonly made out of metal.
The top of the shinbone is done in a similar way. The worn surface is removed, and a new metal tray is then placed on top of the remaining bone. This tray contains a hard plastic spacer that will become the new shock absorber between the smooth metal coverings. Some surgeons may replace the back of the kneecap with a new plastic surface.
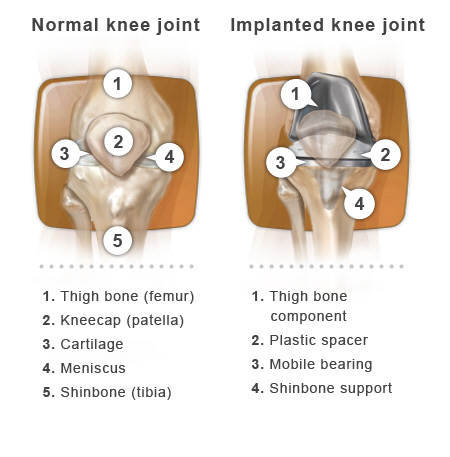
Near the end of your surgery, your surgeon will attach the new metal and plastic coverings to the ends of the bones and the back of the kneecap. This can be done with bone cement where the new knee is essentially glued to the bones. This can be done without cement with certain knee replacement implants that can be press-fitted tightly into the bones and affix to them naturally. Either way, your doctor wants to secure the new knee so you can get back on your feet as soon as possible. When the implant is in position and all the supporting muscles and ligaments are working well, your surgeon closes the incision with stitches, staples or dermabond glue.
When your surgery is over, you will be taken to the recovery room. A nurse will care for you and monitor your condition as your anesthesia wears off. You may experience some symptoms during this time such as blurry vision, dry mouth, nausea, chills, and perhaps some pain. If you do, let the nurse know so that they can provide you with medication to help ease your symptoms if appropriate. After recovering from the anesthesia, you will be asked to do some simple breathing and moving activities. These activities help to prevent possible post-surgical complications, such as developing blood clots in your legs.
Generally, you can expect to be moving your regular room within one to three hours after surgery.
There are different designs for knee replacements. My first knee replacement was a nex-gen flex design. The reason for failure was the stem was to short. Below is a picture of the replacement.
The picture below is from my last replacement. The replacement is called a Zimmer. There is a website that you can go to get information on this type of replacement
Third Knee Revision
My third knee revision was a different design.
This replacement was done because of
complications of the second replacement.
You should receive a card to carry with you, a short time after surgery. This is what it says on the back of my card: Antibiotics required before dental or medical procedures. Implant may activate metal detectors, x-rays replica shown.
Before I have any procedure now, I'm required to have a coarse of antibiotics, to prevent any kind of infection. You can find more information on this on different websites, or ask your doctor.
Hospitals
Hospitals are no different than doctor. Find a quality hospital, research their reputation, and ask around, so you have a much quicker and smoother recovery. I had my knee replacements done in two different hospitals. The first hospital was great and second not so great. Even though I had a very good surgeon the third time, I was not overly fond of the hospital. The staff was not friendly at all and the care was not up to par. I had some nurses that were very rude. One of my nurses waited two hours before me a pain pill. Since you are going to be in the hospital for a few days, you'll want it to be as pleasant as possible. After all you are at the mercy of your caregiver for those first few days.
Therapist
You will also want to find a good therapist, because you are going to need one. Therapists are not all the same either, they have there own methods of doing therapy.
Aftercare Knee Replacement
Make sure you have somebody lined up to help you at home. If not, you will need to find a good skill care unit to go to.
Good Surgeon and Research
Not all people go through what I went through. If I would have had a good surgeon in the first place, I do not think I would have had all the problems that I had encountered. Learn from my mistakes, do your homework before having any kind of surgery.
Update 1/27/2013
1/27/2013
It has been a little over five years since
I had my knee replaced 3 times. July 2007
was my last knee replacement. It has been a long road to recovery since the first Doctor did the surgery wrong twice. The Doctor who cleaned up the first Doctors mess did a great job.
I still have some small problems with this knee. But only because the first surgeon did so much damage. He stretched the ligaments in my knee, which will never heal completely. I have adapted and learned to control it so well I don't even notice it anymore. Amazing how our bodies adapt to overcome a handicap.
Some ask would you recommend having a knee replacement? My answer is if I would have had to live with the first two surgeries, the answer would be no. But with the surgery that was done right, yes.
My husband needs his knee replaced, but refuses to have it done. He is afraid it will go wrong like mine did.
I'm still researching options and trying to keep myself updated on new procedures.For when the day comes and he decides to finally have his surgery.
I tell people don't let my experience scare you and keep you from having this done. I just had a bad surgeon. There are many great doctors out there that know what they are doing.
Recovering and Know Your Body and Get a second opinion
My knee is still recovering, and doing so much better. Be persistent, if you think something is wrong. Don't take their word for it, you know your body, and if you think something is wrong, have it checked out. If you don't get the answers you need, get a second opinion.
Here are websites and searches I found helpful:
http://www.americanarthritis.org/portal/loader.php?seite=practical_tips_for_artificial_knee_joints
Practical Tips for Artificial Knee Joints. Today many orthopedic surgeons perform even more knee replacements than hip replacements. Although some surgeons still advise a certain amount of caution, most experts are convinced that artificial knees are at least as successful as artificial hips, or possibly even more so. The following tips offer some important recommendations. For more information, we would also like to refer you to the tips in the two previous issues of ARTHRITIS INFO.
http://www.medscape.com/viewarticle/421337_2
You will need to join their site in order to view most information. But this is a great site.
Primary Knee Replacement: Management and Alternatives
From Medscape Orthopaedics & Sports Medicine have some really good information
Great information on pain and surgery
http://www.zimmer.com/en-US/pcg.jspx;jsessionid=E5133E04339600D177DB0EEE057AD6E9.zim-prodws2-01
Experiencing PainConsidering SurgeryScheduling SurgeryBeginning Recovery
The only knee replacement inspired
By a woman's shape and size
No one has to tell you that women and men are different. But did you know that even our knees are different? It's true, and you might also not be aware that most knee replacements don't account for the differences between a woman's and a man's knee. Only the Zimmer® Gender SolutionsTM Knee matches your shape and size and has 3 distinct differences from other knee replacements-for a better fit, higher flexion, and more natural movement
Custom Total Knee Replacement
Here is some information I came across recently. It sounds great but scary at the same time. The part that scares me is what if your surgeon messes up like my first surgeon and take out to much bone. What would their solution be for this kind of a problem.
- Custom Knee Replacement
The essentials of a knee replacement surgery are universal, but there are some new techniques and implants that have raised interest in knee replacement. Once such change is the development of a custom fit knee replacement designed to fit more precis
Updated 2/7/2013
2/7/2013
The left knee which was replaced is still going strong. It still gives me fits but educating myself, and knowing what is going on with that knee has help me a lot. Knowing those ligaments are not going to heal completely, let's me know, I will need to adapt, to that sloppy knee. It has a mind of it's own, but so do I. You learn real quick to pay more attention to your surroundings such as gravel. Also be more cautious when walking. A pebble on the sidewalk can send you to the ground so pay attention, so that pebble be on the ground, and not you.








