Polymyalgia Rheumatica - A pain in the neck
My story
I was on vacation summer 2006, traveled to Berkeley to visit a friend for eight days, practiced yoga in 100 plus degrees, walked each and every day for hours. It was grand. Went on my next vacation in August to North Carolina and again had a great time. Came home on August 13th. On Monday morning, August 14th I could not move my left shoulder. I thought I had played too hard and just needed to recover from my holiday. I went to a yoga teacher training on the last weekend and found most of the arm/shoulder poses unavailable to me. In September I decided to detox, sure that I had contracted something on my last adventure. By October, my shoulders, neck and hips were bound up. I finally went to my PCP who referred me to Rheumatology and Immunology. Three months of pain pills, anti-depressants, hypnotics, sleep labs, x-rays, and increasing pain.
I was beyond miserable and saw no relief in sight. In February, I was referred to another rheumatologist. She was leaving the country but agreed to see me on her return. On March 14, 2007 she drew new labs and called in a script for prednisone. I started on 20 mg that night and 20 again in the morning.
I FELT GREAT!!! Seven months of misery and there was immediate relief. That was my four day dose. When it was reduced the pain returned and she thought I might have RA. ( I have a seronegative RA factor.) The challenging point is that I am 47 years old - Too young for this diagnosis. I am thankful she choose to treat the symptoms rather than follow an arbitrary standard, which have delayed the process even longer.
At this writing, I am a year post diagnosis and treatment. Prednisone is the miracle drug anyone who has ever been in pain or discomfort can attest, but comes with a long list of side effects. From that original life altering dose of 20 mg daily, I have been reducing the dosage so that today I am at 4.5mg and in moderate discomfort.
Along with Prednisone, I took Prilosec to protect my belly, calcium and vitamin D to protect my bones. I saw my rheumatologist monthly to check my labs and eyes. Then had bone density test as well. Because of the age of onset, there is some suspicion that this may be a precursor of RA.
So, here are that facts I found after I had the story. You too...
Here are the facts:
Polymyalgia rheumatica is a rheumatic condition that is frequently linked to giant cell (temporal) arteritis. It is a relatively common disorder, with a prevalence of about 700 per 100,000 persons over 50 years of age.
Polymyalgia rheumatica occurs in about 50 percent of patients with GCA, while approximately 15 percent of patients with PMR as the primary diagnosis go on to develop GCA. Some patients have manifestations of both disorders occurring at different times.
Polymyalgia rheumatica is almost exclusively a disease affecting older adults, and is rarely diagnosed under the age of 50 years. In older persons its prevalence approaches that of rheumatoid arthritis.
Few nonwhite individuals have been included in most case series. However, PMR occurs in African-Americans and the disease presentation and response to treatment are similar to that in whites.
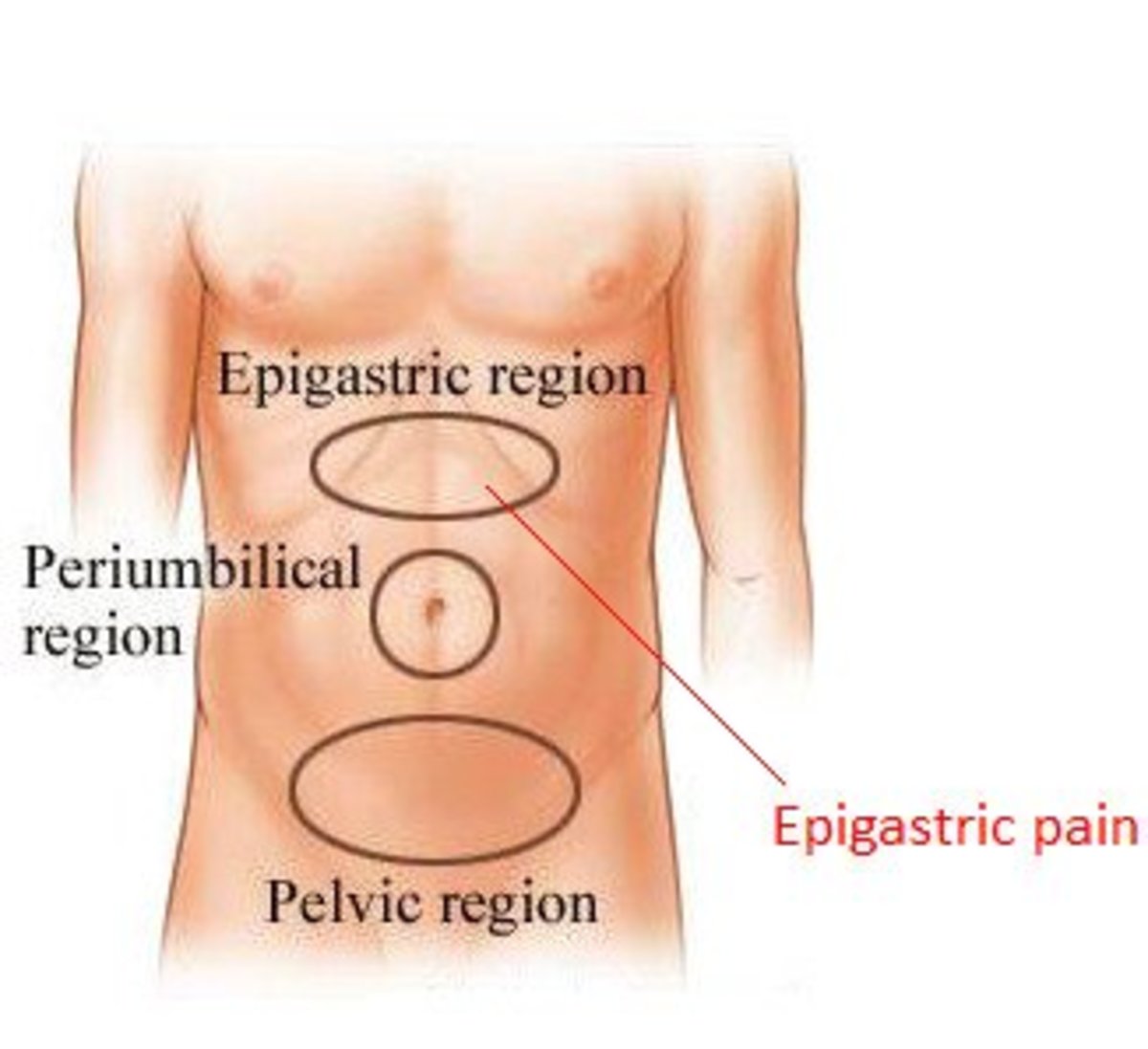
Polymyalgia rheumatica is classically characterized by a subacute or chronic onset of aching and morning stiffness in the shoulders, hip girdles, neck and torso in patients over the age of 50. The symptoms are usually symmetric, but asymmetric pain can occur. Difficulty with activities related to the shoulder and hip stiffness may be reported as trouble dressing (eg, fastening a bra normally, donning a shirt or jacket, or pulling on stockings). Some patients also complain of malaise, fatigue, anorexia, weight loss, and fever, but the high spiking fever that can occur in GCA is rare in patients who have only PMR.
Synovitis and bursitis are considered to be the causes of the discomfort and stiffness found among patients with PMR. However, because the shoulders and hips are surrounded by large muscles, small amounts of synovitis in these joints are not readily detected on physical examination. By comparison, palpable synovitis in more peripheral joints (knees, wrists, and metacarpophalangeal joints) is relatively common in PMR.
Some patients develop swelling and pitting edema of the hands, wrists, ankles, and top of the feet . The edema usually occurs with other signs of PMR but can be the presenting symptom. It appears to represent tenosynovitis and synovitis in regional structures. Tenosynovitis can also cause carpal tunnel syndrome, which occurs in approximately 10 to 14 percent of patients with PMR.
Physical examination in PMR may reveal decreased active range of motion of the shoulders, neck, and hips. Despite the implications of the name "polymyalgia", muscle tenderness is not a prominent feature of this disease, and what tenderness there may be about the shoulders is more likely due to synovial or bursal inflammation than muscular involvement.
Muscle strength is usually normal. However, weakness may become a problem because of disuse atrophy or lack of effort on examination because of pain.
The characteristic laboratory finding in PMR and GCA is an elevation in the erythrocyte sedimentation rate that can exceed 100 mm/h. However, values below 40 mm/h are seen in as many as 7 to 22 percent of patients. This is most likely to occur in patients with limited disease and fewer systemic symptoms and in those who have been treated with corticosteroids.
While there is generally no need in clinical practice to resort to MRI or ultrasonographic imaging in the majority of patients suspected of having PMR, such testing may be useful if the diagnosis is uncertain and/or there are relative contraindications to a therapeutic trial of corticosteroids.
The diagnosis is more difficult to establish in those with atypical presentations. These include age 40 to 50 years, asymmetric symptoms, and ESR less than 40 mm/h. Although there is less experience with use of serum CRP testing to establish the diagnosis of PMR, it may be reasonable to substitute an elevated serum CRP as a criterion for PMR if the ESR is less than 40 mm/h.
As noted above, there is considerable overlap between PMR and GCA. Nevertheless, patients with "pure" PMR lack the classic findings of GCA such as temporal artery tenderness, headache, jaw pain, visual loss, and evidence of noncranial ischemia (such as arm claudication or cerebral ischemia)
The differential diagnosis of PMR includes early seronegative rheumatoid arthritis and a variety of other disorders that can usually be easily distinguished from PMR. These include hypothyroidism, infective endocarditis, fibromyalgia, malignancy, polymyositis, bursitis/tendinitis, and amyloidosis.
Patients with rheumatoid arthritis usually have symmetric polyarthritis of the small joints of the hands and feet, which is persistent and only partially responsive to low doses of prednisone. These findings are different from that in PMR in which fewer joints are swollen, and the swelling subsides completely in response to low dose prednisone.
Polymyalgia rheumatica is characterized by a prompt response to corticosteroids, usually in low doses. The initial dose of prednisone needed to alleviate musculoskeletal symptoms in PMR is lower than that required to control the vascular inflammation associated with GCA.
A higher ESR, larger initial doses of prednisone, and rapid tapering may be associated with earlier relapse. The initial goal of therapy is to achieve symptomatic control using a minimum dose of glucocorticoids. After a period of quiescence, a slow taper of glucocorticoids is begun. The following represents our usual approach:
Depending upon the patient's weight and the severity of symptoms, the starting prednisone dose of between 7.5 and 20 mg/day. Patients usually respond quickly and often note improvement after the first dose. The dose should be increased if the symptoms are not well controlled within one week. Such patients may have underlying GCA or a paraneoplastic syndrome.
Occasional patients find that a single daily dose of prednisone does not provide relief from evening or night-time pain or stiffness. Use of a divided (BID) dose may suffice for some, while others may require an increased total daily dose.
Because many patients will require corticosteroid treatment for more than six months, an assessment of bone mineral density is suggested at or near the time prednisone is begun. Calcium and vitamin D supplementation are appropriate for most patients. Prophylactic use of other agents, such as bisphosphonates may be considered for some. Patients found to have osteoporosis will need therapeutic, rather than preventive, intervention. These issues are discussed in detail elsewhere.
Among patients with PMR who are at increased risk for corticosteroid-induced side effects, the addition of methotrexate may be steroid-sparing, as suggested by some, but not all, studies. However, methotrexate is seldom indicated for the vast majority of patients with PMR but without GCA, since adverse effects are relatively mild with the low doses of prednisone required to adequately control the disease.
In most patients, PMR runs a self-limited course over months to years and steroid therapy can eventually be discontinued. There is no evidence of increased mortality associated with this disorder. As a result, every effort must be made to control symptoms with a minimum of drug-induced side effects.
In addition, ongoing monitoring should be performed for signs suggestive of GCA. In a large series described above, 4.4 percent of patients with pure PMR had a positive temporal artery biopsy. These patients are usually not detected unless they develop manifestations of vasculitis, which presumably can also occur over time in some patients with initially normal temporal arteries.
A current note
That's my story. It took a great deal of research to find information on this disorder as it is often overlooked in the arthritis pages. I am thankful to both my rheumatologist and friends in the medical field who continually supported me when it looked like there were no correct answers. Women in pain are often medicated with anti-depressants, hypnotics, and minimal pain relief medications. I was in pain, and had a many sleepless nights, which clearly could lead to depression. Once the pain was treated I became the vibrant excited person I know myself to be. Even though I still have pain and stiffness, I am able to move in my life. And I am glad.