General Considerations And The Physiological Actions Of The Parathyroid Glands
The Parathyroid Glands
A General Overview
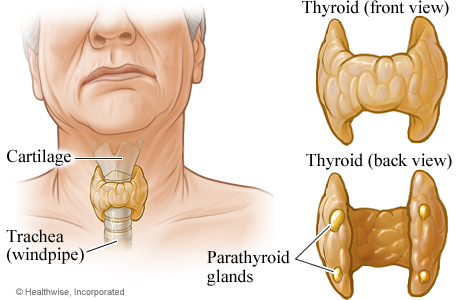
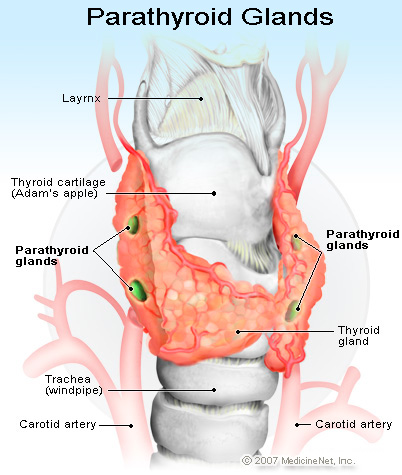
Collip identified the active principle of the parathyroid glands in 1924. There are two superior and two inferior parathyroids together weighing 120mg. The superior parathyroids develop along with the thyroid and the inferior parathyroids develop along with the thymus. Twigs from the superior and inferior thyroid arteries supply the parathyroids. Aberrant parathyroids may be seen at the trachea-esophageal groove, substance of the thyroid gland or thymus, retro-esophageal space, anterior mediastinum, surface of the pericardium, carotid bifurcation, jugular foramen or pharyngeal mucosa. The parenchyma consists of chief cells arranged in the trabecular, alveolar or acinar patterns with mature fat cells interspersed. Parathyroid hormone (PTH) is secreted by chief cells. The gland, in addition, contains large polyhedral oxyphil cells with bright eosinophilic cytoplasm which appear after puberty. Pre and pro-parathyroid hormones are precursors formed during the synthesis of PTH.
Parathyroid Hormone
This is a single chain polypeptide having 84 aminoacids. In circulation PTH is metabolized to biologically inactive fragments. The circulating PTH is a mixture of polypeptide chains of different biological activity. Therefore the biological activity does not correlate strictly with the total levels of PTH. The secretion of PTH is controlled by several factors. Circulating calcium exerts the major control on PTH secretion and release. Fall in serum calcium stimulates, and rise inhibits PTH secretion. This reciprocal relationship is maintained as long as the serum calcium level ranges between 7 and 15mg/dl. Rise in serum phosphate stimulates PTH secretion indirectly by decreasing calcium levels.
Calcium homeostasis
Normal calcium concentration is essential for bone formation, blood coagulation, cardiac contractility, neural function and secretory activities. Calcium stabilizes biological membranes and serves as a cofactor in cellular reactions. The plasma calcium level is maintained within a narrow range of 9-11mg/dl (4.5- 5.5meq/liter).
The Glands Secreting PTH
Actions of PTH
The ultimate effect of this hormone is to conserve body calcium and increase its level in extracellular fluid. It exerts its influence in several ways.
- Parathyroid hormone increases calcium resorption from bone,
- It increases tubular reabsorption of calcium.
- It increases absorption of calcium from the intestine
- It increase the renal loss of phosphate and hydroxyproline
- It enhances the formation of 1,25(OH)2D3 in the kidneys.
- It increases the secretion of acid-pepsin in the stomach, and
- It activates the cyclic AMP-adenyl cyclase system in its target cells.
Parathyroid hormone acts on the kidneys to conserve calcium and eliminate phosphate, bicarbonate and sodium. It stimulates osteoclastic activity in bone, inhibits collagen formation by osteoblasts and accelerates osteolysis. The net result is the resorption of bone with release of calcium, products of collagen breakdown and alkaline phsophatase into blood system. Vitamin D which enhances intestinal absorption of calcium and facilitates deposition of calcium in bone, influences the effects of PTH. The net effect on bone depends on the complex interplay of PTH, vitamin D and renal functions.
© 2014 Funom Theophilus Makama