- HubPages»
- Health»
- Health Care, Drugs & Insurance»
- Prescription & Over-the-Counter Drugs
Effects of raising high-density lipoproteins cholesterol
Effects of raising high-density lipoproteins cholesterol HDL-C by fibrate, niacin or combined statin therapy on cardiovascular events
Abstract
Clinicians have recognized the importance of reduction of the levels of the low-density lipoproteins (LDL-C) in an effort of reducing the risks associated with cardiovascular disease. However, studies have shown the contribution of other lipid fractions such as high-density lipoproteins cholesterol (HDL-C) as well as triglycerides (TG) to impact on the cardiovascular health increasing future preferences. However, care initiatives towards the reduction of associated cardiovascular disease typically focus on the highly effective statin therapy, which acts as LDL-C lowering agent, and have lesser triglycerides lowering as well as HDL-C raising effects. It is important to incorporate other therapies i.e. nicotinic acid and fibrate therapies in reduction of the associated cardiovascular risks. The study analyses the effects of raising high-density lipoprotein cholesterol levels (HDL-C) by utilization of fibrate, niacin or a combined therapy on cardiovascular events.
Effects of raising high-density lipoproteins cholesterol HDL-C by fibrate, niacin or combined statin therapy on cardiovascular events
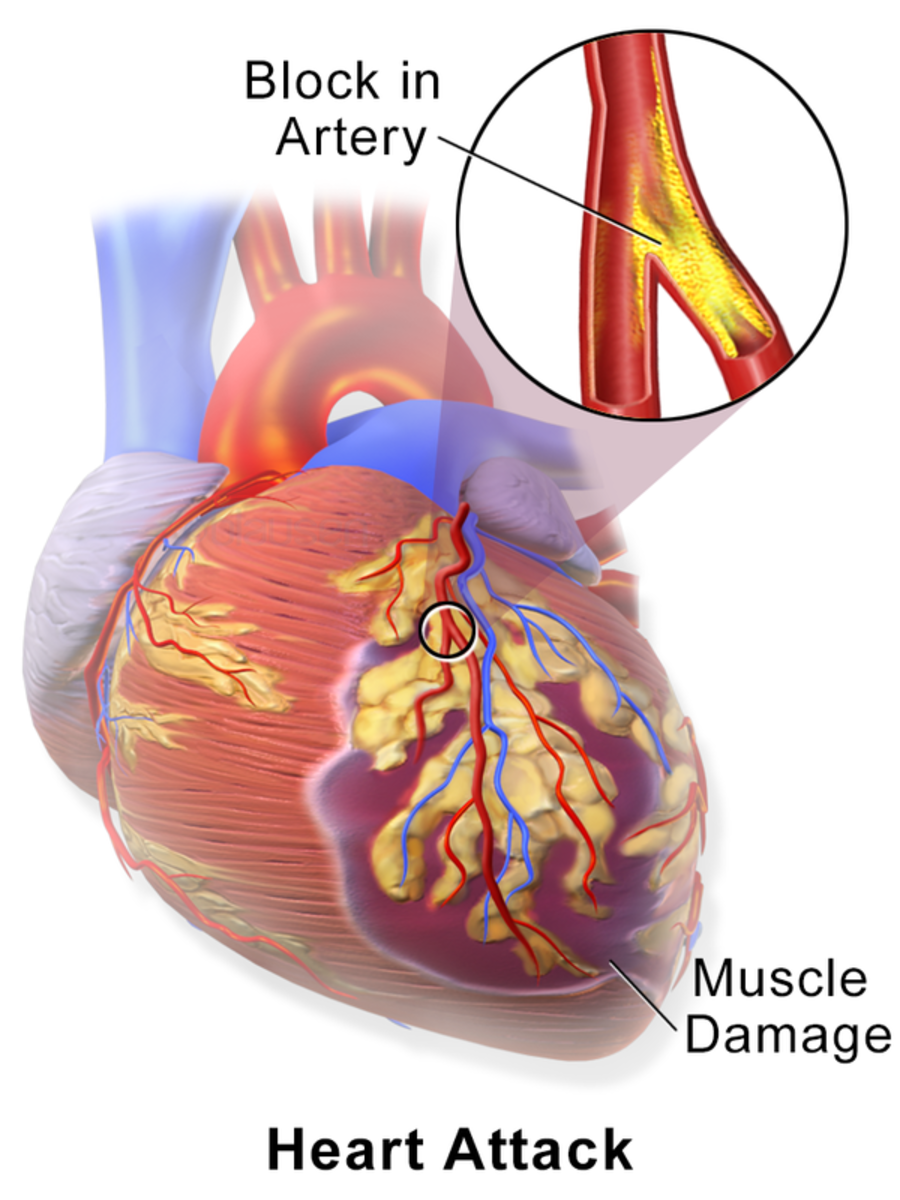
Epidemiological studies have shown that low-high-density lipoproteins cholesterol (HDL-C) increase the risk of morbid coronary events. Thus, the interventions to correct the low levels of HDL-C are essential, as they are cardio protective. A number of randomized interventions have been used to address the situation using fibrates, nicotinic acid or in combination of statin therapy to prove their effectiveness (Rader, 2002). These trials demonstrate that treatments to increase HDL-C ought to deliver clinically significant improvements in the prognosis of the conditions and ensure safe strategies in minimizing cardiovascular risks in the patients with dyslipidemia. Diabetes carries a high risk of getting cardiovascular disease especially stroke or coronary heart disease (CHD) and is the leading cause of death among patients especially type two diabetes. Statin therapies alone reduces risks of major cardiovascular risks by about 1/5th per millimole litre with reduction of LDL-C with major residual risks remaining high. Combined multifactorial interventions have proven to reduce the associated risks significantly, but significant danger signs remain. Current guidelines, therefore, call for aggressive treatment modalities to reduce LDL-C and blood pressure and glucose levels in the patients (Brown et al., 2001).
Statin therapy
Cardiovascular associated diseases (CVD) are among the leading causes of morbidity and mortality worldwide. According to the estimations, dyslipidemia accounts for 1/3 of the world burden of heart related diseases estimating at least four million deaths associated by inadequate control of the condition. The management of dyslipidemia with statin therapy to affected individuals with cardiovascular diseases has shown to reduce these events. Several trials and meta- analyses have been conducted to investigate the effects of statin therapy. These studies have demonstrated that statin therapies ought to significantly reduce the levels of low-density lipoproteins thus reduces the incidences of the associated cardiovascular events. However, in spite their efficiency, statin therapy does not reduce the associated cardiovascular risks (P.P. Toth, 2012).
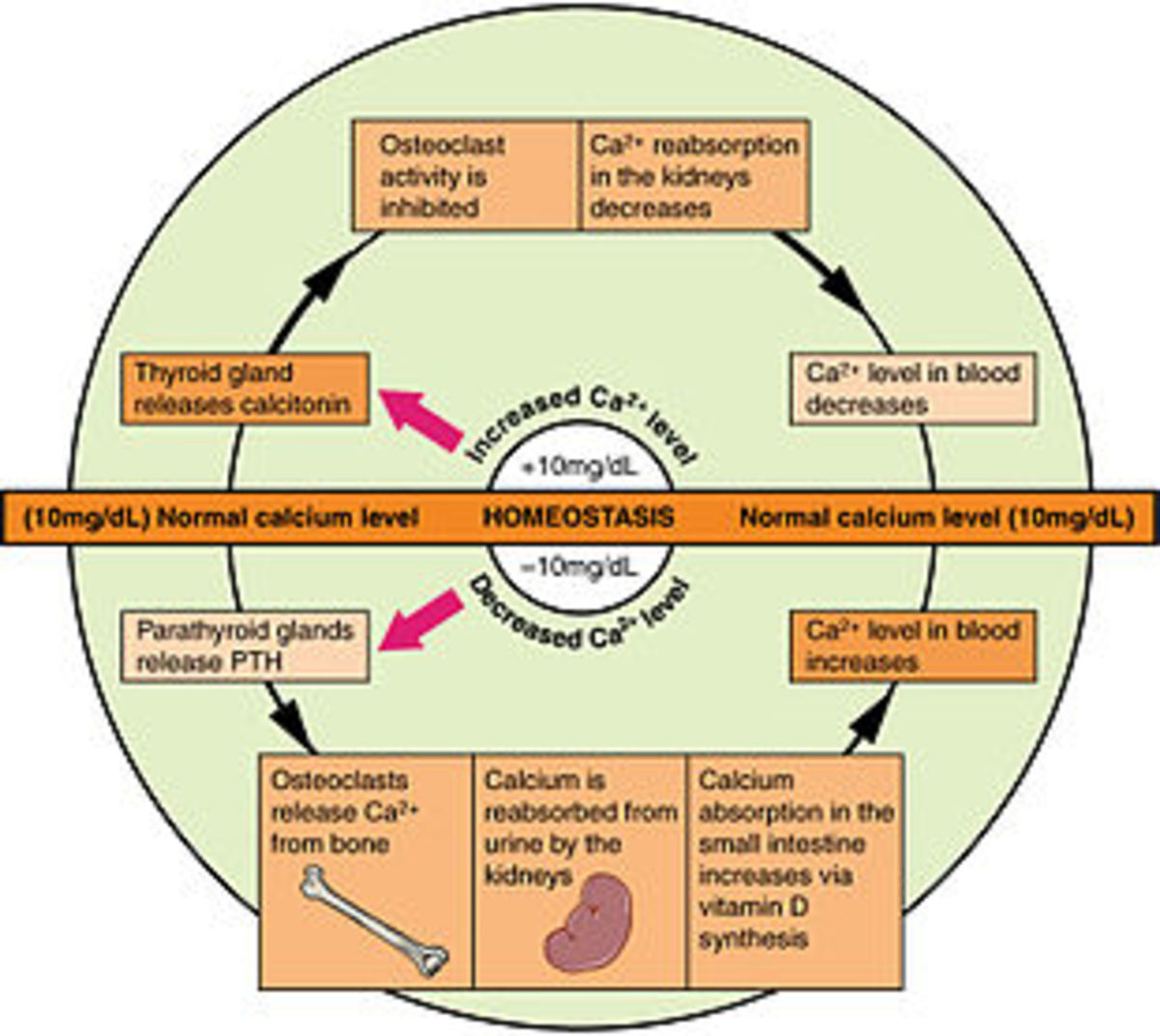
The residual cardiovascular risk remains even after administration of the statins especially among the high-risk patients with diabetes. This associated cardiovascular risk stems from the low levels of high-density lipoprotein cholesterol levels and elevated levels of triglycerides. The low levels of HDL-C in patients are a significant, independent predictor of heart associated risks as well leads to an increase in the levels of HDL-C associated with reduced cardiovascular states. High levels of triglycerides possess as a significant risk for cardiovascular events. High-triglyceride levels are an indication of atherogenic lipoproteins remnants i.e. very low-density lipoproteins (VLDL-C) which further aggravate the situation. The elevated levels of triglycerides combined with low-density lipoprotein cholesterol (LDL-C) as well as a very low density lipoproteins (VLDL-C) is a good measure of non- high-density lipoprotein cholesterol that is a better predictor of cardiovascular events than the low-density lipoproteins alone. Thus, a combination therapy ought to be necessary for addressing the multiple lipid targets through combination of niacin or fibrate in the therapy (Bays, 2008).
Extended-release niacin or ezetimibe effects on the carotid intima-media thickness
The study involved additional of treatment to a statin monotherapy to either modify the lipid profile by raising the high-density lipoprotein cholesterol levels or further lower the low-density lipoproteins cholesterol levels. Patients with coronary heart conditions and with coronary heart disease risk equivalent receiving long-term statin therapy were incorporated in the study. Their levels of LDL-C levels ought to be less than 2.6 mmol in a litre and HDL-C levels between 1.3 to 1.4 mmol in a litre. Patients were randomly assigned to receive extended niacin therapy or ezetimibe only each day. The primary end for the study was the difference of change of the baseline of the carotid media thickness after therapy of 14 months.
The mean HDL-C levels in the combined therapy group increased by 18.4 percent in the 14-month period. However, the mean LDL-C levels in the ezetimibe group decreased by 19.3 percent. Niacin therapy reduced LDL-C levels as well as triglyceride levels while ezetimibe reduced HDL-C and triglycerides levels. In comparison, niacin had a greater efficiency in change of the mean carotid thickness over the period causing a significant reduction of the mean and maximal carotid media thickness. The incidence of major cardiovascular events lowered in the combined treatment group comparing to the monotherapy ezetimibe group. The study illustrates the effectiveness of utilization of combined therapy of utilization of extended release of niacin therapy over the utilization of ezetimibe statin monotherapy in the reduction of related cardiovascular risks (Taylor et al., 2009).
Effects of adding a fibrate to a statin therapy in the reduction of cardiovascular associated risks.
Despite the widespread utilization of statin therapy in the treatment of cardiovascular events, a considerable residual risk of cardiovascular events remains. Although the associated reduction risk of cardiovascular events is by 20 to 50 percent, there remains a considerable risk for future events. A study was conducted evaluating the effects of adding a fibrate therapy to a statin therapy to reduce the cardiovascular risks that are associated with elevated levels of triglycerides as well as low levels of high-density lipoprotein cholesterol. Subjects with dyslipidemia with residual risk in addition to atorvastatin therapy a statin therapy was evaluated after fenofibrate acid was incorporated in the treatment.
A controlled study performed on patients with mixed dyslipidemia (fasting levels of triglycerides greater r equal to 150mg/dl and HDL-C less or equal to 105 mg/dl for men and 55mg/dl for women.) participants had a history of coronary heart disease or equivalent risk. Participants were divided into groups with each group receiving an additional fibrate therapy while the other received only the statin therapy. However, in the study, fenofibric acid combination with atorvastatin therapy was associated with greater incidences of renal related adverse effects compared to the atorvastatin monotherapy, i.e., 6.5 percent risk compared to 0.9 percent. Compared to the monotherapy of atorvastatin, fenofibrate acid combination with atorvastatin further reduced the associated risks of cardiovascular events on the participants who utilized the combination of a statin and fibrate therapy (Davidson et al., 2014).
Effects of combined therapy in type two (2) diabetes mellitus patients
A study to investigate whether combined therapy (of statin and a fibrate) comparing with a monotherapy of statin would reduce the risk of cardiovascular disease. The study participants were patients with type 2 diabetes who are at a risk of cardiovascular disease. Participants mean follow-up period was 4.7 years a total of 5518 patients receiving simvastatin treatment that was reinforced with fenofibrate therapy. The study primary outcome was the occurrence of the first non-fatal myocardial infarction, stroke or resulting death from cardiovascular ailment. The study was divided into two groups i.e. the fenofibrate group and the placebo group. The rate of cardiovascular associated deaths was 1.5 percent in the fenofibrate group and 1.6 in the placebo group with no great significant difference in the outcome. This was attributed to the heterogeneity in treatment effects in relation to sex, with men benefiting and possible harm resulting to the women. Only the patients with high-baseline triglyceride level and low levels of high-density lipoprotein cholesterol levels benefiting. The combination however did not reduce the rate of fatal cardiovascular incidences, non-fatal stroke and myocardial infarction incidences in comparison to the monotherapy treatment. These results of the study were however contradictable and never supported the routine utilization of combined therapy in a reduction of cardiovascular associated risks (Ginsberg et al., 2010).
Niacin and fibrate monotherapy
Effects of raising high-density lipoprotein cholesterol (HDL-C) levels using fibrate
A low level of high-density lipoprotein cholesterol levels possesses a greater risk factor to coronary disease attainment. According to the veteran’s affair high-density lipoprotein trial (VA-HIT), secondary prevention study, it demonstrated that coronary heart diseases could be reduced during a median follow-up of 5 years through treatment of the patient with fibrate acid derivatives. Gemfibrozil, a fibrate derivative, was used to raise the low levels of high-density lipoprotein cholesterol levels. A randomized placebo-controlled trial conducted to determine the whether the reduction in cardiac heart diseases events with Gemfibrozil ought to be attributed to changes in the plasma lipid levels. A total of 2531 participants with a history of cardiac heart disease was selected for the study. The participants had low levels of HDL-C (Mean 32md/dl) with low-density lipoprotein cholesterol levels (mean 11mg/dl). The participants were randomly selected to receive treatment (Peter P Toth, Zarotsky, Sullivan, & Laitinen, 2009).
Results- the outcome for the study was to determine the lipid level baseline for 18 months of treatments with the combined incidence of non-fatal infarction and coronary heart disease death. The concentration of HDL-C was inversely related to the coronary heart disease events. The study illustrated that the CHD ought to be significantly reduced by 11 percent with treatment of fibrate therapy alone for every 5mg/dl increase in HDL-C. During Gemfibrozil therapy, only increase in high-density lipoproteins predicated a lower risk of coronary heart disease incidents. However, for the study, neither triglycerides nor low-density lipoprotein cholesterol levels predicated the associated coronary diseases. The concentration of high-level lipoproteins cholesterol levels achieved in the treatment illustrated a significant reduction of cardiovascular events in patients with low levels of high-density lipoproteins. The change in the HDL-C levels partially illustrated the beneficial effects of cardiovascular disease reduction with utilization of fibrate therapy (Robins et al., 2001).
As monotherapy agents to be used alone in treating cardiovascular events, niacin and fibrates have proved to alter the lipid parameters as well as reduce associated cardiovascular events. Among the two, niacin has proved to exert the greatest effects on the greatest range of lipoprotein abnormalities. It possesses an established profile of safety (Meyers, Kamanna, & Kashyap, 2004). However, a combination therapy of statin and niacin provide great benefits as a treatment modality. This is manifested through reduction of associated atherogenic abnormalities in lipids, slowed the rate of atherosclerosis progression in the coronary event in the patient as well as a reduction of the residual cardiovascular risk. This enhances the achievement of optimal lipid values that are associated with reduced cardiovascular events for which the magnitude of risk reduction accompanies the achievement of the greater number of lipid goals. Studies have estimated that a fixed dose of niacin ER therapy ought to reduce directly medical costs of associated cardiovascular events effectively than a high-dose monotherapy (Koskinen et al., 1992).
Conclusion
Reduction of the low-density lipoproteins cholesterol levels (LDL-C) with statin therapy is a cornerstone of management of dyslipidemia for the patients with cardiovascular conditions according to the treatment guidelines. However, among the statin therapy treated patients who achieve the low levels of lipoproteins, the residual risk of getting another cardiac disease remains undoubtedly high. Although researchers suggest that intensive levels of the low levels of lipoproteins on the patients ought to provide additional benefit to the patient, it however does not suppress the associated events of further cardiovascular risks sufficiently. Thus, it is significant that there is an unmet clinical need in the care of the cardiovascular affected patients. Thus, it is important to view any additional interventions for the management of the patients. Reduced levels of high-density lipoproteins cholesterol levels (HDL-C) < 1.03 mmol/L (40 mg/dL) for the males and (HDL-C < 1.29mmol/L (50 mg/dL) levels in females is an independent predictable factor of coronary heart conditions (Whitney et al., 2005).
High-density lipoprotein cholesterol level is a logical therapeutic target towards the reduction of cardiovascular associated risks among the statin-treated patients even among those who have achieved low levels of lipoprotein level. Thus, low levels of HDL-C is common in patients suffering from dyslipidemia with cardiovascular conditions. A therapeutic strategy ought to be aimed at raising the HDL-C levels and at the same time lower the levels of LDL-C to offer clinical benefits beyond that achieved by LDC-C reduction alone. To achieve this nicotinic acid and fibrate can be incorporated. However, nicotinic acid has great potency with studies demonstrating that a combined therapy of nicotinic acid and statins possesses acceptable normality’s, tolerable levels, good lipoprotein profiles with the ability of reducing regression of coronary risks for patients with established heart disease. A combination of statin and an HDL-C raising agent is important to consider despite achievement of the low levels of lipoproteins in statin monotherapy (Investigators, 2012).
References
Bays, H. (2008). Safety of Niacin and Simvastatin Combination Therapy. American Journal of Cardiology, 101.
Brown, B. G., Zhao, X. Q., Chait, A., Fisher, L. D., Cheung, M. C., Morse, J. S., … Albers, J. J. (2001). Simvastatin and niacin, antioxidant vitamins, or the combination for the prevention of coronary disease. The New England journal of medicine (Vol. 345, pp. 1583–1592).
Davidson, M. H., Rosenson, R. S., Maki, K. C., Nicholls, S. J., Ballantyne, C. M., Mazzone, T., … Stolzenbach, J. C. (2014). Effects of Fenofibric Acid on Carotid Intima-Media Thickness in Patients With Mixed Dyslipidemia on Atorvastatin Therapy: Randomized, Placebo-Controlled Study (FIRST). Arterioscler.Thromb.Vasc.Biol.
Ginsberg, H. N., Elam, M. B., Lovato, L. C., Crouse, J. R., Leiter, L. A., Linz, P., … Byington, R. P. (2010). Effects of combination lipid therapy in type 2 diabetes mellitus. The New England Journal of Medicine, 362, 1563–1574. doi:10.1056/NEJMoa1001282
Investigators, T. A. H. (2012). Niacin in Patients with Low HDL Cholesterol Levels Receiving Intensive Station Therapy. The New England Journal of Medicine, 365, 2255–2267.
Koskinen, P., Mänttäri, M., Manninen, V., Huttunen, J. K., Heinonen, O. P., & Frick, M. H. (1992). Coronary heart disease incidence in NIDDM patients in the Helsinki Heart Study. Diabetes care (Vol. 15, pp. 820–825). doi:10.2337/diacare.15.7.820
Meyers, C. D., Kamanna, V. S., & Kashyap, M. L. (2004). Niacin therapy in atherosclerosis. Current Opinion in Lipidology, 15, 659–665.
Rader, D. J. (2002). High-density lipoproteins and atherosclerosis. The American Journal of Cardiology, 90, 62i–70i. doi:10.1097/00041433-199310000-00008
Robins, S. J., Collins, D., Wittes, J. T., Papademetriou, V., Deedwania, P. C., Schaefer, E. J., … Rubins, H. B. (2001). Relation of gemfibrozil treatment and lipid levels with major coronary events: VA-HIT: a randomized controlled trial. JAMA : the journal of the American Medical Association (Vol. 285, pp. 1585–1591).
Taylor, A. J., Villines, T. C., Stanek, E. J., Devine, P. J., Griffen, L., Miller, M., … Turco, M. (2009). Extended-release niacin or ezetimibe and carotid intima-media thickness. The New England Journal of Medicine, 361, 2113–2122.
Toth, P. P. (2012). Niacin in Patients with Low HDL Cholesterol Levels Receiving Intensive Statin Therapy. Yearbook of Endocrinology. doi:10.1016/j.yend.2012.05.027
Toth, P. P., Zarotsky, V., Sullivan, J. M., & Laitinen, D. (2009). Niacin and fibrate use among patients with high triglycerides and low high-density lipoprotein cholesterol. Current Medical Research and Opinion, 25, 1355–1363.
Whitney, E. J., Whitney, E. J., Krasuski, R. A., Krasuski, R. A., Personius, B. E., Personius, B. E., … Gotto, A. M. (2005). A randomized trial of a strategy for increasing high-density lipoprotein cholesterol levels: effects on progression of coronary heart disease and clinical events. Annals of Internal Medicine, 142, 95–104.