IMMEDIATE TYPE ALLERGIC ASTHMA: ROLE OF MACROPHAGES, MAST CELLS & FREE RADICALS AND THEIR TREATMENT WITH MEDICINAL PLANT
IMMEDIATE TYPE ALLERGIC ASTHMA: ROLE OF MACROPHAGES, MAST CELLS & FREE RADICALS AND THEIR TREATMENT WITH MEDICINAL PLANTS AS IMMUNOMODULATORS AND ANTIOXIDANTS
IMMEDIATE TYPE ALLERGIC ASTHMA: ROLE OF MACROPHAGES, MAST CELLS & FREE RADICALS AND THEIR TREATMENT WITH MEDICINAL PLANTS AS IMMUNOMODULATORS AND ANTIOXIDANTS
Immunology plays an important role in understanding and diagnosis of diseases, and further it is the most rapidly developing area of biomedical research for the prevention and treatment of a wide range of disorders. During the last 35 years immunology has witnessed an explosion of knowledge and experimental skills that has expanded our view of the immune system and means of searching for its structure and functions in an impressive way (Haddad et al., 2005).
Our immune system possesses two principal components: innate and adaptive immunity, which work together to defend the body against infection. The innate system or natural immunological mechanism, which essentially serves as a short-term first line of defense is inherited. This non-specific defense includes certain mechanical and chemical factors in the skin and mucous membranes of the body (such as lungs), which are involved in combating the initial attempt of a microbe to invade. In contrast, the adaptive system, also termed specific immunity, is acquired through interactions with the environment. It has two major characteristics - It can discriminate self from nonself, leaving host tissues undamaged and selectively destroying the pathogenic material; and it remembers the encounters with specific pathogenic agents such that subsequent encounters by the host with the same agents activates the immune response more quickly and vigorously, preventing recurrence of the disease caused by the specific pathogen. Although, the immune system, for the most part, has beneficial effects, there can be detrimental effects as well. An underactivated immune system increases risks of opportunistic, while an overactivated immune system leads to many complications, including inflammation, allergy and autoimmunity. The immune response mobilizes a battery of effector molecules that act to remove antigen or pathogens by various mechanisms. Generally these effector molecules induce a localized inflammatory response that eliminates foreign particles called as antigen, without extensively damaging the host’s tissue. Under certain circumstances, however, this inflammatory response can have deleterious effects, resulting in significant tissue damage or even death. This inappropriate immune response is termed as hypersensitivity or allergy and the study of these is termed immunopathology. Hence, an unchecked and unbalanced immune system affects good health and quality of life (Corren & Casale, 2002; Borchers et al., 2002; Jindal, 2007).
The traditional classification for hypersensitivity reactions divides the reactions into 4 types. Type I reactions (immediate hypersensitivity reactions) involve immunoglobulin E (IgE)–mediated release of histamine and other mediators from mast cells and basophils. Type II reactions (cytotoxic hypersensitivity reactions) involve immunoglobulin G or immunoglobulin M antibodies bound to cell surface antigens, with subsequent complement fixation. Type III reactions (immune-complex reactions) involve circulating antigen-antibody immune complexes that deposit in postcapillary venules, with subsequent complement fixation. Type IV reactions (delayed hypersensitivity reactions, cell-mediated immunity) are mediated by T cells rather than by antibodies (Goldsey, 2003; D’urzo, 2007; Jindal, 2007).
The Immediate Hypersensitivity occur quickly or immediately after exposure to the allergen which induces a humoral antibody response. Some examples of immediate hypersensitivity are asthma, allergic conjunctivitis, allergic rhinitis ("hay fever"), anaphylaxis, angioedema and urticaria (hives). Among these, the most common one is asthma which is often subdivided into either allergic asthma or non allergic asthma. Asthma is broadly defined as a chronic disease of the airways that is characterized by variable airflow obstruction, bronchial hyperresponsiveness, and underlying inflammation. It may also be classified based on the intrinsic or extrinsic etiology, severity, or level of control. Allergic (extrinsic) asthma is characterized by symptoms that are triggered by an allergic reaction. Allergic asthma is airway obstruction and inflammation that is partially reversible with medication. However, allergic asthma is triggered by inhaled allergens such as dust mite allergen, pet dander, pollen, mold, etc. resulting in asthma symptoms. Hence, allergic asthma is considered as a chronic inflammatory condition rather than a respiratory disease (Corren and Casale, 2002; Haddad et al., 2005; Bernstein, 2008).
Careful examination of most people who get frequent asthma fails to bring out any visible deficits in the immune system. They have all the immune cells and antibodies they need in roughly the right amounts and all the various parts appear to work just fine. But still such people get sick so often. It was hypothesized that in some people the immune system fails to function properly for a relatively subtle, invisible reason, much as a well-equipped army might lose its fighting form due to apathy or disunity. However, even people who develop frequent colds manage to fight off thousands of other infections every day.
For this reason, an alternate hypothesis comes to mind that over-susceptibility to a particular type of infection may be caused by something more specific than general immune weakness. Scientists can measure the effects of drug on individual white blood cell types and note changes in activity, but they don’t know how to interpret the results of those measurements as a whole. After all, the immune system is a system, and systems are notoriously complicated to analyze. To acknowledge this limitation, the term immunomodulatory is used rather than immune stimulating or immune suppressing when they refer to a substance that causes measurable alterations in immune function. This terminology notes a change (modulation), but does not jump to conclusions regarding whether that change is good, bad, or indifferent (Gasbarro, 2001; Jindal, 2004; D’urzo, 2007).
`Immunomodulation` is any procedure which can alter non specific immunity by interfering with its functioning. Immunostimulation and immunosuppression both need to be addressed in order to regulate normal immunological functioning. Immunostimulation and immunoinhibition or immunosupression are all routes that permit immunomodulation. If it results in enhancement of immune reactions, it results in immunostimulation and primarily implies stimulation of the non-specific immunity that is stimulation of the function and efficiency of granulocytes, macrophages, natural killer cells, complement, and the various effector substances. It consists of techniques that stimulate the body's own immune system to overcome diseases Immunosuppression mainly implies reduced resistance against infections and stress and may be due to environmental or chemotherapeutic factors. It represents a state of the body's immune system to respond adequately to a disease. Hence, immunostimulating and immunosuppressing agents both have their own standing (Atal et al., 1986; Dasgupta et al., 1998; Borchers et al., 2000; Bradding et al., 2006; Sagrawat and Khan, 2007).
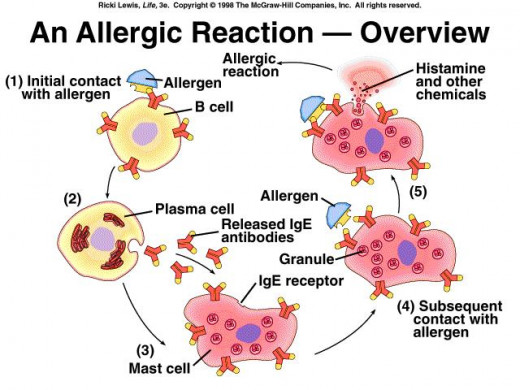
The course of allergic or the immediate hypersensitivity reaction can typically be divided into 2 phases: the early- or acute phase reaction or period of sensitization and the late-phase reaction or the allergic reaction itself. The early- or acute phase reaction occurs within 1 hour after allergen exposure (in a sensitized individual) and is thought to be driven by cross-linking of allergen-specific IgE bound to the surface of resident mast cells via the high-affinity IgE receptor. When a foreign substance (antigen) enters our body, it meets up with a B cell, a type of white blood cell (lymphocyte). Lymphocytes are key players in our immune system. They circulate throughout the body looking for invaders and are programmed to recognize invading antigens based on a previous encounter. When encountering an antigen, B cells, in cooperation with other cells, produce a large number of substances called antibodies, which identify the antigen (Corren & Casale, 2002; Reed, 2006).
The antibodies are made of a special kind of protein called immunoglobulin (Ig). Immunoglobulins are of five kinds— IgA, IgD, IgE, IgG and IgM. Among them, IgE is most often involved in allergic responses. Antigens that bind to IgE are called allergens, because they can cause an allergy. The IgE antibodies produced by B cells attach themselves to certain cells, including basophils — another type of white blood cell — as well as mast cells found in our respiratory and gastrointestinal tracts and in our skin. As more of the allergen enters our body, the antibodies "grab" the allergen. This triggers the basophils and mast cells to release powerful chemicals, including histamine (Figure A). Thus, the mast cell is the key effector cell in immediate hypersensitivity reactions (Bellanti, 2006).
The late-phase reaction is in many respects a sequel to these mast cell–driven events and occurs 12–24 hours after allergen challenge. The hallmark of the late-phase reaction is the recruitment of inflammatory cells, including eosinophils, basophils, T cells, neutrophils, and macrophages, to the site of allergic inflammation. In the reaction phase, re-exposure to the allergen results in the binding of the allergen to mast-cell-bound IgE antibody. The large, basophilic granules present in the mast cells are released into the tissues; this process of degranulation releases a variety of pharmacologically active compounds; some directly from the granules (e.g. histamine and heparin), others newly synthesized by the cell soon afterwards. The acute-phase reaction therefore is not only responsible for early clinical signs of allergic inflammation, but is essential for the generation of late-phase responses and chronic allergic disease. Mast cells can be stimulated nonimmunologically by direct triggers such as neuropeptides, basic compounds, complement components, and certain drugs (Corren and Casale, 2002; Bernstein, 2008).
Figure A. Role of mast cells in allergic reaction
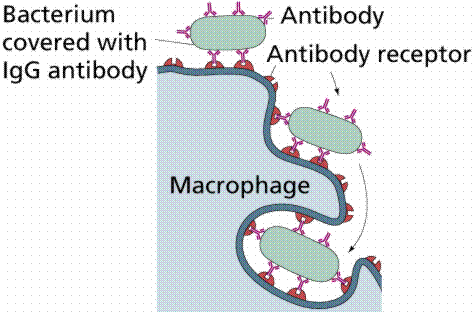
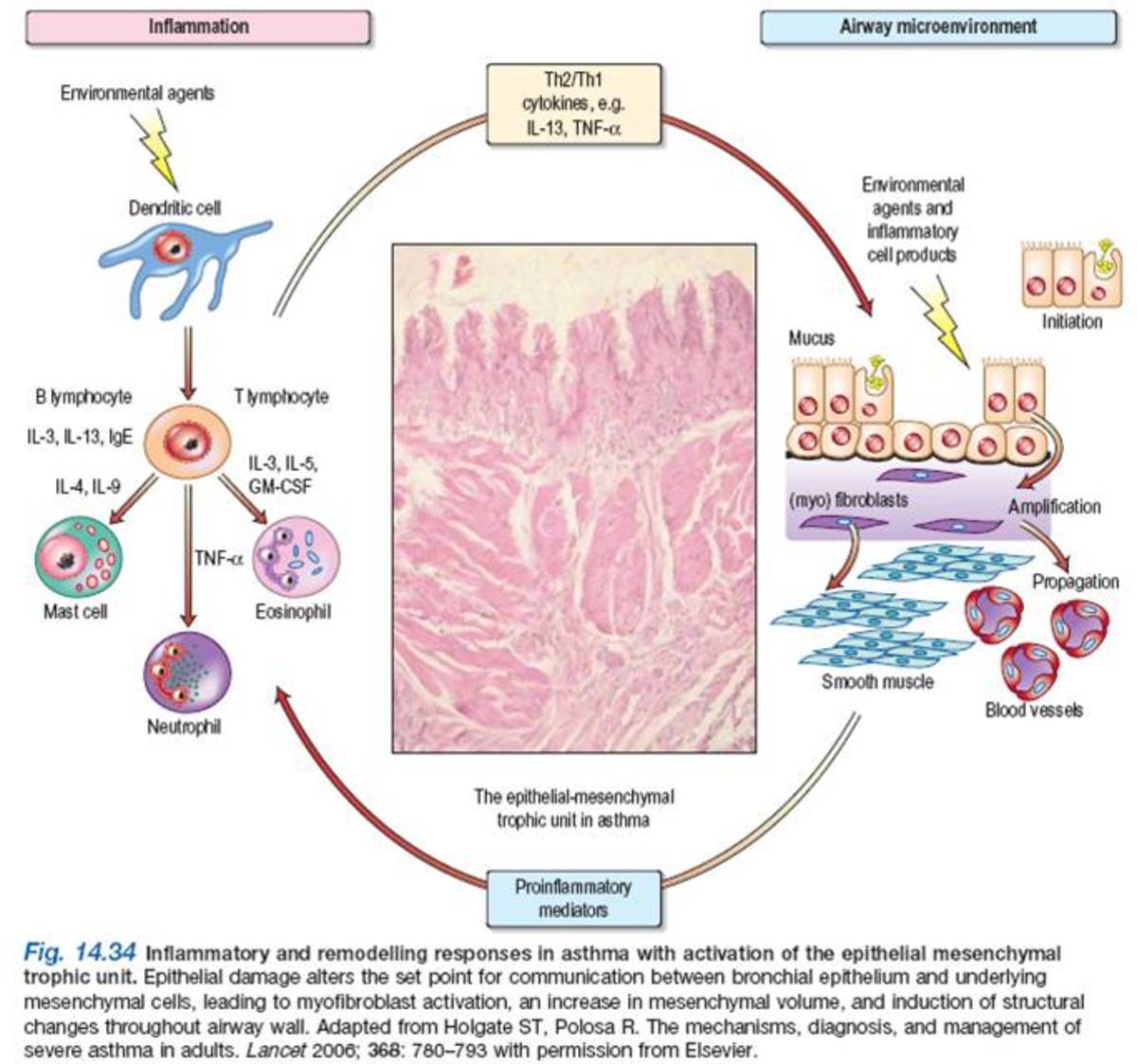
The special job of identifying foreign invaders and helping to determine whether they are good or bad guy, is done by macrophages. If the macrophages decide the foreign invader is a harmful microbe, then they may devour it (Fig. B). If the macrophages wrongly identify harmless antigens as bad guys, they set in motion inflammatory processes, including the activation of mast cells. They may also inhibit allergic inflammation through the secretion of various inhibitory mediators. The secretion of these inhibitory mediators may be impaired in patients with asthma (Gopumadhavan et al., 2005; Schepetkin et al., 2008).
Figure B. Role of macrophages in the formation of antibodies
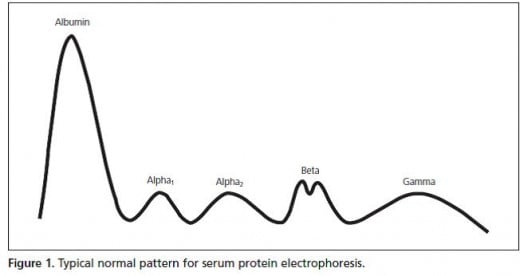
Total protein concentration is also an indication of immune system disorders. The levels of different blood proteins rise or fall in response to such disorders as cancer and associated protein-wasting syndromes, immune-system disorders, impaired nutrition etc. The pattern of serum protein electrophoresis results depends on the fractions of two major types of protein: albumin and globulins (Fig.C). The different types of blood proteins are separated into fractions of five distinct classes: albumin, alpha1-globulins, alpha2-globulins, beta-globulins, and gamma-globulins (immunoglobulins) (Deshmukh et al., 1999; Soresi & Togeas, 2006).
Fig. C: Typical normal pattern for serum protein electrophoresis
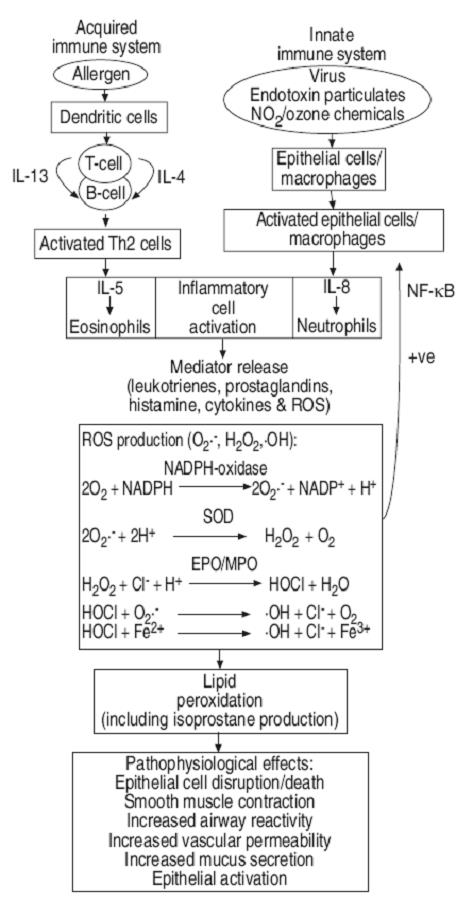
Immediate type allergic asthma, a chronic inflammatory condition, is also characterized by an excess of free radicals, which irritate and inflame tissues and cause excessive immune reactions. Immune responses unavoidably produce free radicals because, in limited amounts, they are a valuable part of the defense mechanism. Free radicals are other most potent mediators of inflammation. Free radicals are unstable molecules produced as a normal by-product of respiration. In excessive amounts these free radicals can fuel the flame of inflammation and damage healthy tissues (Devasagayam and Sains, 2002; Gayathri et al., 2005).
There are some compounds that can neutralize these free radicals and prevent them from doing further harm. These compounds are called as antioxidants. They help reduce most inflammatory reactions including asthma, allergies and post-operative inflammation by quenching free radicals. An oxidant-antioxidant imbalance occurs in patients with bronchial asthma, supporting the concept of systemic oxidative stress in these conditions. The best way to deal with a chronic inflammatory disease is to completely stop the allergic reaction using natural Immunomodulating and Antioxidising agents (Fig. D).
Fig. D. Correlation between immune system and oxidation systemHence, immunomodulation can go hand in hand with antioxidant activity for treating a chronic inflammatory condition like immediate-type allergic-asthma (Desmarchelier et al., 2005; Aherne et al., 2007).
In order to treat allergic asthma, symptomatic treatments for inhibiting the reaction steps of the altered immune system and oxidation mechanism of immediate type allergic asthma should be used. That is, the treatments are carried out by inhibiting the release of chemical mediators accompanying the degranulation and/or by inhibiting allergic reactions induced by the released chemical mediators including free radicals (Jayaprakasha et al., 2006; Ashvin and Mishra, 2007).
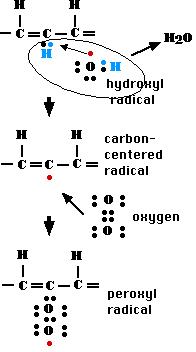
Fig. E. formation of free radical
Figure E shows that a hydroxyl radical removes a hydrogen atom from one of the carbon atoms in the fatty acid chain (only a portion of which is shown) forming a molecule of water and leaving the carbon atom with an unpaired electron; thus now a radical.
Since the pathogenic mechanism(s) of allergic-asthma are unknown, animal models have been developed to investigate the various disease processes, as well as to enable study of environmental and genetic factors which may contribute to disease development. A murine model for asthma presents numerous advantages when compared with use of other animal species. Adult mice weigh approximately 20–25 g. Being small, they are easy to handle and relatively inexpensive. A mouse model offers the opportunity to explore mechanisms of allergic reactions because of the existence of numerous immunological reagents specific for murine cytokines, growth factors and cell surface receptors. Murine models have provided fundamental information regarding certain features of asthma (James, 2002; Kim et al., 2007).
Intensive research during the last several decades had highlighted the role of lymphocytes, immunoglobulins, macrophages, mast cells and various autocoids in the etiopathogenesis of allergic conditions. Inspite of the voluminous literature on the subject, the treatment of allergic diseases continues to be far from satisfactory. The available treatment options for allergic diseases have major limitations owing to low efficacy, associated adverse events, and compliance issues. Considering the entire array of components involve in the immune system, it present as a complex, but precisely interwoven network of biochemical mechanisms. It is vulnerable to oxidative stress from reactive oxygen and nitrogen species, which have potential to damage various biological molecules produced during the functioning of the immune system. During certain diseased states there is a need for boosting the antioxidant availability and thereby potentiating the immune mechanism. In this context immunomodulators having antioxidant abilities especially derived from Indian medicinal plants, have considerable potential. Despite the advanced and increasing understanding of the pathophysiology of asthma and other allergic diseases, current treatment remains unspecific and targets late events within the allergic cascade (Almeida et al., 2006; Aherne et al., 2007).
Medicines frequently prescribed or sold over the counter for allergy relief include antihistamines, decongestants, and corticosteroids. Many chemotherapeutic agents available today are basically immunosuppresants, most of them are cytotoxic and exert a variety of side effects. Further, the metabolism and clinical safety of these agents has also not been clearly established. Further the drugs used at present are costly and have low benefit-risk ratio. But since these drugs are not without side effects, the advent of a safe and more sure-acting drug for the prevention and treatment of allergic disorders has been anticipated (Gasbarro et al., 2001; Acun et al., 2005).
On the other hand there are reasons to believe that plant extracts having pharmacological and biological activity can serve as a good source for newer immunostimulants. Fortunately, it is possible, by use of nutritional therapy, to reduce asthmatic symptoms through more natural methods. Many medicinal plants contain photochemicals that modulates the immune system without the dangerous side effects of pharmaceutical prescriptions. Some of the basic reasons for the dependence of people towards traditional herbal medicines are, popularity worldwide - for primary healthcare, several side effects of the synthetic drugs, better cultural acceptability, better compatibility with the human body and increased efficiency of new plant derived drugs, prohibitive cost of allopathic drugs, great interest in alternative medicines and unavailability of allopathic drugs in remote areas, rising trend in last decade in many developed and developing countries, a growing interest in maintaining good health, and a growing interest in preventing future health problems and a view to address specific health concerns, particularly during ageing are the main reasons for the deviation of people towards plant-based drugs (Dahanukar and Thatte 2000; Patwardhan et al., 2004; Patwardhan and Gautam, 2005; Singh et al., 2007).
It is advisable to avoid the use of plant based medicines on which no scientific studies are available since they may contain toxic substances which are harmful or even dangerous to health and the main objective of taking herbal medicines is to improve one's health and not to be harmed. Hence, herbal medicines should also be subjected to extensive scientific and pharmacological screening before being recommended as drug. One of the therapeutic strategies in Ayurvedic medicine is to increase body’s natural resistance to the disease-causing agent rather then directly neutralizing the agent itself in practice. This is achieved by using extracts of various plant materials called Rasayanas. Immunomodulation, especially using rasayanas drugs could provide an alternative to conventional chemotherapy under the condition of impaired immune responsiveness (Devasagayam & Sainis, 2002; Patwardhan et al., 2004; Haddad et al., 2005; Blanc et al., 2006; Sundararajan et al., 2006; Reed, 2006; Singh, 2007).
REFERENCES:
Acun, C., Tomac, N., Ermis, B., and Onk, G., (2005). Effects of inhaled corticosteroids on growth in asthmatic children: A comparison of Fluticasone propionate with budesonide. Allergy Asthma Proc. 26(3) : 204 - 206.
Aherne, S.A., Kerry, J.P., and O’Brien, N.M., (2007). Effects of plant extracts on antioxidant status and oxidant-induced stress in Caco-2 cells. British Journal of Nutrition. 97 : 321 - 328.
Almeida, P., Macari, T., Portela, C.N., and Pohlit, A.M., (2006). Antioxidant, cytotoxic and UVB-absorbing activity of Maytenus guyanensis Klotzch. (Celastraceae) bark extracts. Acta Amazonica.36(4) : 134 -140.
Ashvin, V.D., and Mishra, S.H., (2007). In-vitro antioxidant activity of an adaptogenic homeopathic formulation. Phcog Mag. 3 (10) : 124 - 128.
Bellanti, J.A., (2006). The best new articles in the specialty of allergy, asthma, and immunology. Allergy Asthma Proc. 27(3): 186 - 96.
Bernstein, D.L., (2008). ABCs of Asthma. Clinical Cornerstone. 8(4): 9 - 25.
Blanc, P.D., Chen, H., Katz, P.P., et al. (2006). Complementary and alternative medicine practices among adults with asthma and rhinitis: relation to physical health status in prospective follow-up. Chest Meeting Abstracts. 130: 164 - 165.
Borchers, A.T., Sakai, S., Henderson, G.L., et al. (2000). Shosaiko-to and other Kampo (Japanese herbal) medicines: A review of their immunomodulatory activities. Journal of Ethnopharmacology. 73 : 1 - 13.
Corren, J., and Casale, T., (2002). Immunomodulation of Asthma: Where Do We Stand?. Current Allergy and Asthma Reports. 2 : 433 - 435.
Dahanukar, S.A., Kulkarni, R.A., and Rege, N.N., (2000). Pharmacology of medicinal plants and natural products. Indian Journal of Pharmacology. 32 : S81-S118.
Desmarchelier, C., Pacciaroni, A.V., Abate-Daga, D., Coussio, J., Gil, R.R., and Silva, G.L., (2005). Antioxidant and free radical scavenging activities of Misodendrum punctulatum, Myzodendrone and Structurally Related Phenols. Phytother. Res. 19 : 1043 - 1047.
Devasagayam, T.P.A., and Sainis, K.B., (2002). Immune system and antioxidants, especially those derived from Indian medicinal plants. Indian Journal of Experimental Biology. 40 : 639 - 655.
Gasbarro, R., (2001). Identifying and managing patients with asthma and allergy. Drug Topics. 32 : 68 - 77.
Gayathri, V., Asha, V.V., and Subramoniam, A., (2005). Preliminary studies on the immunomodulatory and antioxidant properties of Selaginella species. Indian Journal of Pharmacology. 37 (6) : 381 - 385.
Goldsy, R.A., (2003). Immunology. 5th Edn. 363.
Gopumadhavan, S., Rafiq, M., Venkataranganna, M.V., and Mitra, S.K., (2005). Antihistaminic and antianaphylactoc activity of HK-07, a herbal formulation. Indian journal of Pharmacology. 37(5) : 300 - 303.
Haddad, P.S., Azar, G.A., Groom, S., and Boivin, M., (2005). Natural Health Products, Modulation of immune function and prevention of chronic diseases. Advances Access Publication. 2 (4) : 513 - 520.
James, T.L., (2002). Allergy Testing. Am Fam Physician. 66 : 621 - 626.
Jayaprakasha, G.K., Jaganmohan Rao, L., and Sakariah ,K.K., (2006). Antioxidant activities of curcumin, demethoxycurcumin and bisdemethoxycurcumin. Food Chemistry, 98 : 720–724.
Jindal, S.K., (2007). Bronchial asthma: the Indian scene. Current Opinion Pulm Med.13(1) : 8 - 12.
Kim, S.J., Kim, C.H., Moon, H.S., Song, J.S., and Park, H.S., (2007). Time sequence of airway remodeling in a mouse model of chronic asthma: the relation with airway hyperresponsiveness. J Korean Med Sci. 22 : 183 – 191.
Patwardhan, B., and Gautam, M., (2005).Botanical immunodrugs: scope and opportunities. Drug Discov Today. 10(7) : 495 - 502.
Patwardhan, B., Vaidya, A.D.B., and Chorghade, M., (2004). Ayurveda and natural products drug discovery. Current Science. 86(6) : 789 - 799.
Patwardhan, B., Warude, D., Pushpangadan, P., and Bhatt, N., (2005). Ayurveda and traditional chinese medicine: a comparative overview. eCAM. 2(4): 465–473.
Reed, C.E., (2006). The natural history of asthma. J Allergy Clin Immunol. 118 : 543 - 548.
Schepetkin, I.A., Xie, G., Kirpotina, L.N., Klein, R.A., Jutila, M.A., and Mark, T., (2008).Quinn Macrophage immunomodulatory activity of polysaccharides isolated from Opuntia polyacantha. International Immunopharmacology. 8 : 1455 − 1466.
Singh,S., Khajuriaa,A., Tanejab,S.C., Khajuriab, R.K.,Singha, J.,Johria,R.K., and Qzia,G.N., (2008). The gastric ulcer protective effect of boswellic acids, a leukotriene inhibitor from Boswellia serrata, in rats. Phytomedicine. 15 : 408–415.
Soresi, S., and Togias, A., (2006). Mechanisms of action of anti-immunoglobulin E therapy. Allergy Asthma Proc. 27(2 Suppl 1): 15 - 23.
Sundararajan, R., Haja, N.A., and Mukherjee, P.K., (2006). Cytisus scoparius link - A natural antioxidant. BMC Complementary and Alternative Medicine.13 : 6 – 8.