The main clinical syndromes in Renal pathologies
Introduction
This hub may seem more for the medical practitioners, but why? It is also for the patients because these syndromes are manifested ON THE PATIENT!. So, there are a lot to gain and in as much as there are medical terms here, it has also been made simpler. Hence, enjoy!
oedema

Renal Edema
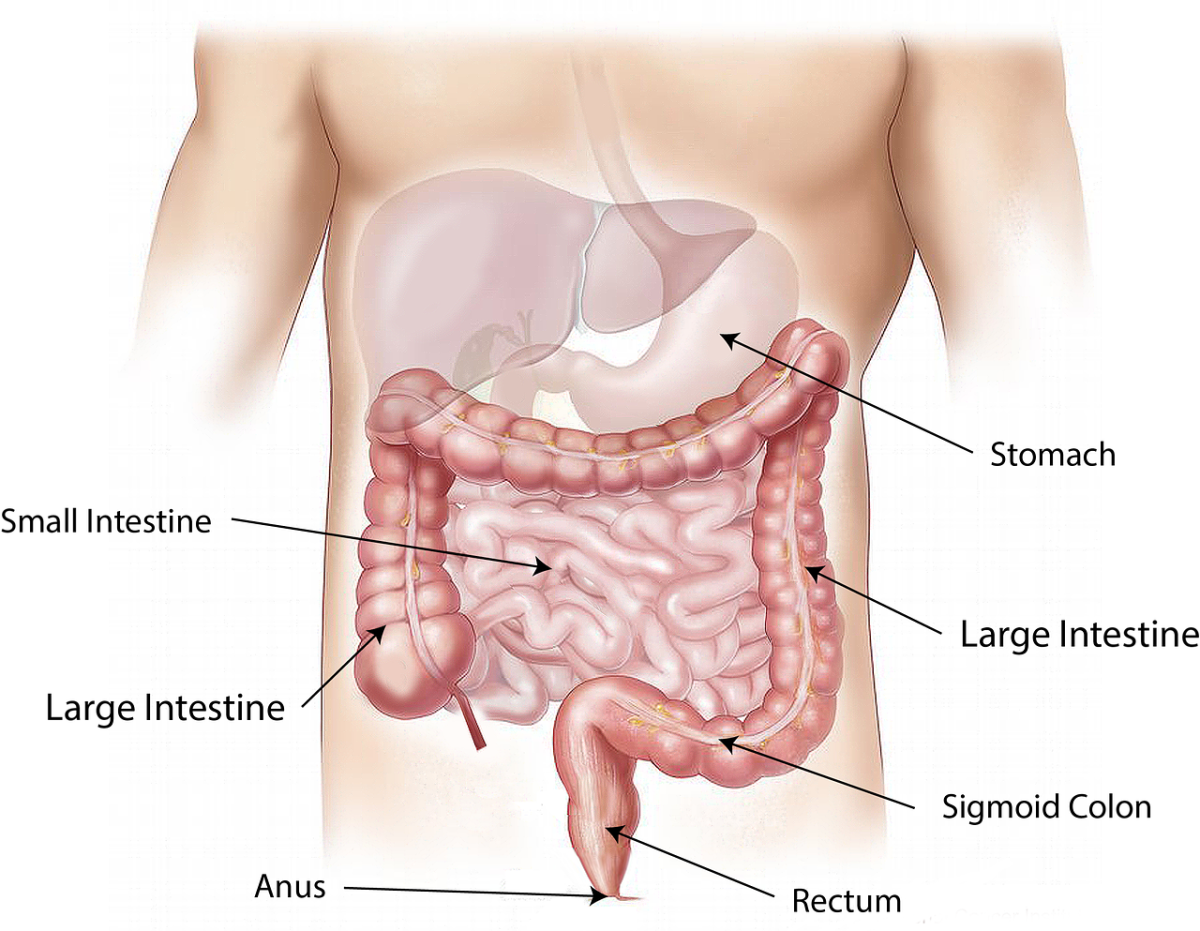
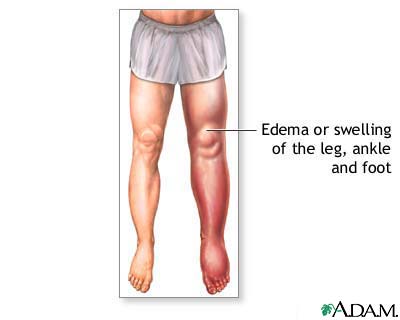
Oedema of renal aetiology is quite specific in most cases and can easily be differentiated from oedema of other origin, e.g. cardiac oedema, by the affection of loose connective tissue (the eyelids, the face) rather than of the lower extremities. Renal oedema can develop and resolve quickly. In pro nounced cases, oedema is usually uniform over the entire trunk and the ex tremities (anasarca). Not only the skin but also subcutaneous fat and the internal organs become oedematous. The liver usually becomes oedematous and enlarged, but in renal diseases the enlargement of the liver is usually proportional to enlargement of the other ograns, and is never so pronounced as in cardiac oedema. Greater or lesser amount of fluid is ac cumulated in the serous cavities, e.g. in the pleural, abdominal, and pericardial cavities. Oedema can be revealed by palpation. It can also be confirmed by the McClure-Aldrich test: 0.2 ml of isotonic sodium chloride solution is injected into the skin on the median surface of a forearm and the time of disappearance of the resulting weal is noted. In a healthy sub ject, the weal is resolved within one hour. In the presence of a marked oedematous syndrome, the dynamics of oedema during treatment can be better assessed by repeating the test in several days with measurement of girths of the extremities and the abdomen at the same level, by determining the fluid level in the pleural and abdominal cavities, by weighing the pa tient, and also by determining daily diuresis and water balance of the body (the ratio of the taken and eliminated liquid during 24-hour period).
Oedema, like the general disorder in the water-salt metabolism, arises due to various causes in renal diseases.
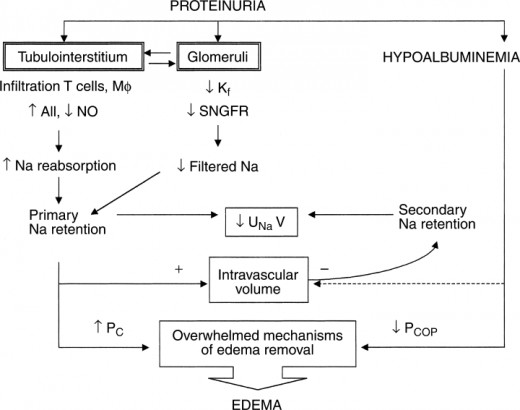
1. Diffuse increased permeability of the capillary wall is important in development of oedema in many diseases of the kidneys attended by the oedematous syndrome. Great importance in this process is attributed to auto-immune processes and increased hyaluronidase activity of the blood serum, which as a rule, attends many diseases of the kidneys
Hyaluronidase intensifies depolymerization of hyaluronic complexes of mucopolysaccharides that form the intercellular substance (interen-dothelial "cement") and the basal membrane of the capillary wall. Porosity of the wall thus increases. The decreased blood serum content of calcium is also important because calcium compounds with protein (calcium pro-teinate) is a component part of the intercellular "cement"; change in the blood pH (acidosis) is important as well. Because of the generalized increase in capillary permeability, not only water and the dissolved substances, but also much protein pass from the blood to the tissues. Depolymerization of mucopolysaccharides of the intercellular substance of tissues increases the quantity of molecules in the intercellular fluid and raises its colloidal-osmotic pressure.
It follows that the nephrotic syndrome is characterized not only by in creased permeability of the capillary wall that facilitates fluid transport to the tissues, but also conditions are provided for fluid retention in the tissues, because the increased colloidal-osmotic pressure of the intercellular fluid accounts for its hydrophilic property: the intercellular fluid easier ab sorbs water and gives it back with difficulty. The comparatively high protein content in the oedema fluid (transudate) explains the higher density and lower mobility of oedema in the presence of deranged capillary permeability compared with oedema associated with hypoproteinaemia.
In the presence of increased capillary permeability, transudate is ac cumulated in the subcutaneous fat and other highly vascularized tissues. Serous cavities usually contain low amounts of fluid. Disordered capillary permeability in the glomeruli causes proteinuria and promotes develop-i ment of hypoproteinaemia. Oedema of this type occurs not only in diseases of the kidneys but in some other diseases as well, e.g. it can also be allergic or angioneurotic (Quincke's oedema), in cases with bee stinging, etc.
2. Colloidal-osmotic (hypoproteinaemic) mechanism of oedema development is also important in the nephrotic syndrome. It is manifested in a decreased plasma oncotic pressure due to high proteinuria which usually occurs in such patients, and also in protein passage through the porous capillary walls into the tissues. Oedema of predominantly colloidal-osmotic origin obeys the laws of hydrostatics and tends to develop in the first instance in the lower extremities in walking patients and in the loin of bed-ridden patients. Hypoproteinaemic oedema usually occurs in cases where the blood protein content is less than 35-40 g/1 (3.5-4 g/100 ml) and albumins are contained in the quantity below 10-15 g^/1 (1-1.5 g/100 ml). Qualitative changes in the composition of the blood proteins are very important. Highly dispersed proteins (albumins) are mainly lost in the urine in nephritis patients; the amount of globulins decreases to a lesser extent. Osmotic pressure is determined by the quantity of molecules contained in a unit volume of blood plasma rather t their molecular weight. The loss of highly dispersed albumins, specific colloidal-osmotic pressure is about three times that of dispersion globulins, therefore substantially decreases oncotic pres the blood.
Hypoproteinaemic oedema arises not only in the nephrotic syndr can also develop in long starvation (hunger oedema), deranged abs( in the small intestine (disordered absorption syndrome), cancer cai and in some other diseases attended by a decreased protein contenl blood plasma.
3. Hypernatriaemic oedema (to be more exact, hypernatr: oedema) is explained by the retention of the highly hydrophilic sodiu in 4he blood and especially in the tissues. Administration of I chloride in large doses can thus cause this oedema. Hypernatriahi tending diseases of the kidneys is an additional factor intensifying feet of increased capillary permeability and hypoproteinaemia. He factors, and in the first instance hypersecretion of aldosterone (the s cortex hormone) and antidiuretic hormone (the posterior pituitai mone), are very important in the accumulation of the sodium ion i diseases.
Any oedema, irrespective of its intensity, indicates upset osmo tion in which the hormone link (aldosterone-antidiuretic hormone s is the decisive one. This hormone system is mainly responsible for taining constant volume and ionic composition of the blood, volume of circulating blood decreases even insignificantly (which cai in renal diseases when part of the liquid passes from the blood to due to increased porosity of the capillary wall or decreased oncotic p of the blood), the volume receptors, located mainly in the walls of tr atrium and the common carotids, are stimulated. Protective mech respond to this stimulation to maintain the intravascular v Aldosterone secretion by the adrenal cortex is intensified to ii sodium reabsorption in the walls of the renal tubules and its concen in the blood, and to promote its accumulation in tissues. Accorc some authors, the quantity of aldosterone excreted in the urine dui hours increases in the nephrotic oedema from 2-10 to 25-200/ more. Sodium excretion in the urine thereby decreases considi Secondary hypersecretion of aldosterone that develops as a comper reaction, e.g. in oedema or a sudden loss of water from the body, is secondary hyperaldosteronism as distinct from the phyperaldosteronism that occurs in tumours or hypertrophy of the a cortex. Increased sodium reabsorption in the renal tubules is follo\ increased reabsorption .of water. High concentration of the sodium lood (due to its intensified reabsorption in the renal tubules) lates osmoreceptors and intensifies secretion of the antidiuretic hor by the pituitary gland, which in turn intensifies the facultative reab-ion of water in distal tubules still more. If the primary cause of na (increased capillary permeability, decreased oncotic pressure of ixa) is still active, fluid is not retained in the blood vessels and con-s its passage from the blood to the tissues to intensify oedema. . Oedema can occur in acute anuria of the kidneys in acute poisoning with corrosive sublimate), hypovolaemic reduction of blood circula-in the kidneys (profuse blood loss, shock), and also in the terminal e of certain chronic renal diseases (retention oedema). But decreased aerular filtration becomes only important in the presence of other runners of oedema rather than an independent factor. For example, in ire renal insufficiency attended by pronounced filtration disturbances, ema is often absent or even resolved, if any.
It should also be noted that none of the above mechanisms of renal ema develops independently but becomes only a dominating factor in i or that case.
clinical signs and pathogenesis of Nephrotic syndrome


Series of lectures on the Glomerulus 1-10
Nephrotic syndrome
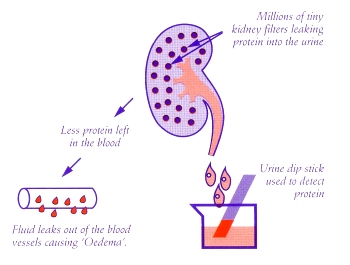
The nephrotic syndrome (symptom complex) is characterized by pronunced proteinuria, hypoproteinaemia (mainly due to hypoalbuminemia), hyperlipidaemia (hypercholesterolaemia), and oedema.
The nephrotic syndrome occurs in chronic glomerulonephritis, amiyloidosis, malaria, sepsis, tuberculosis, collagenosis, diabetes mellitus and certain other diseases. Less frequently the cause of the nephrotic syndrome cannot be established immediately, but in most cases a detailed analysis of anamnestic data and a thorough examination of the patient and also in chronic glomerulonephritis. These forms of the nephrotic syndrome occur mostly in children. Cases where the cause of renal dystrophy is unclear are identified as lipid nephrosis.
It is believed that the nephrotic syndrome is caused by metabolic disorders, mostly upset fat and protein metabolism, with subsequent derangement of capillary permeability in the glomeruli. Protein and lipids contained in large quantity in primary urine of these patients nfiltrate the tubular wall to cause drastic dystrophy in the epithelial cells. the auto-immune mechanism is of great significance for the development of the chronic nephrotic syndrome. It has been proved by animal experiments: small doses of nephrotoxic serum provoke nephritis in rabbits; a picture characteristic of the nephrotic syndrome develops on administration of large doses.
Pathological anatomy. The following morphological signs of the nephrotic syndrome develop, in addition to the changes characteristic for the main disease. The kidneys are enlarged ("large white kidneys") and their capsule is easily removed. Histological studies reveal dystrophic changes in the epithelium of the tubules, especially of the convoluted tubules. Lipid deposits can be found in the basal parts of the epithelial cells. The glomeruli are affected by dystrophy; especially specific are changes in podocytes and endothelial cells with which the disordered permeability of the glomerular membrane is associated.
Clinical picture. The main, and often the only complaint of patients is persistent oedema. It is especially pronounced on the face which becomes swollen and pallid, the eyelids are only a narrow slit, and the patient opens his eyes in the morning with difficulty. The legs, the loin, the skin of the abdomen and the hands are also affected by oedema. The oedema is mobile: when the skin is pressed by the finger, a depression remains in it which soon disappears. Fluid is accumulated also in the internal organs and the serous cavities. In typical cases the arterial pressure remains unchanged or even decreased.
As the oedema progresses, diuresis usually decreases and the patient often eliminates only 250-400 ml of urine a day. The specific gravity of the urine is high (1.030-1.040) and it contains much protein, to 10-20 g/1 and more. Cases were reported where the urine contained 24 g/1 of protein. Fine dispersed molecules of albumins prevail among protein. It is believed that the increased filtration of the plasma protein through the glomerular capillary wall and also disordered reabsorption of protein molecules by the affected tubular epithelium are important in the aetiology of proteinuria in the nephrotic syndrome. Great quantity of hyaline, granular and\ waxy casts, and cells of renal epithelium are found in the urinary sediment. The presence of leucocytes and erythrocytes in the urinary sedimentyis not characteristic for the nephrotic syndrome. Doubly refracting cholesterol crystals are usually found, which are, as a rule, absent in renal diseases proceeding without the nephrotic syndrome.
A long-standing and persistent proteinuria causes protein depletion of the body and a stable reduction of its content in the blood plasma (1.5 and even 2 times). The albumins become especially deficient, and the albumin to globulin ratio, which is normally 1.2—2.0, decreases significantly. The content of a2-globulins, and also 7-globulins, slightly increases. Proteinuria and hypoproteinaemia (especially hypoalbuminaemia) largely account for oedema that develops in the nephrotic syndrome (see "Renal Oedema"). It has been established that the loss of protein in the urine is aggravated by the renal catabolism of plasma proteins (proteolysis of part of serum protein during its reabsorption in the tubules) and also, probably, by the increased protein loss through the alimentary tract.
Among the constant symptoms are pronounced hyperlipidaemia, increased blood serum concentration of cholesterol (to 13-15 mmol/1, i.e. 2 or 3 times as great), phospholipids, and neutral fat. These changes are probably secondary to upset protein metabolism and hypoproteinaemia. Laboratory studies reveal three characteristic signs of the nephrotic syn drome: proteinuria, hypoproteinaemia, and upset lipid metabolism (hypercholesterolaemia).
The blood clearing function of the kidneys is not substantially affected in the nephrotic syndrome, and azotaemia does not develop for a long time. The main functional renal tests remain normal for a long time, but the tubular secretion can decrease. Biopsy of the kidneys supplies valuable information concerning the nature of the nephrotic syndrome in chronic renal diseases.
Course. If the main disease does not progress, the nephrotic syndrome lasts for years. Oedema and the urinary syndrome intensify at times usually when provoked by an attending infection. Patients with the nephrotic syndrome are sensitive to coccal infection. They often develop recurrent pneumonia and erysipeloid inflammation of the skin. These patients usually died before antibiotics were discovered. Vascular thrombosis is likely to occur in patients with the nephrotic syndrome. The prognosis depends mostly on the main disease and the attending infections.
Treatment. The main disease should be treated. In the presence of pronounced hypoproteinaemia, the patient is prescribed a diet rich in proteins (2—2.5 g/kg body weight without reference to oedema) and poor in sodium chloride. Plasma or concentrated human albumin is given intravenously. Corticosteroids (prednisolone) and immunodepressants (imurane, etc.) are prescribed. If oedema is pronounced, the patient is given diuretics: furantril (furocemid), 0.04 g per os every other or third day, in combination with verosperon (0.075-0.15 g/day per os) to remove oedema. Sanatorium andhealth-resort therapy in dry climate (Central Asia) is recommended during relative remissions.
Note that Nephrotic and Nephritic syndromes are very similar, but most journals and thoughts differentiate them as Nephrotic syndrome consisting of Oedema which is absent in Nephritic syndrome and the presence of hypertension in Nephritic syndrome which is as well absent in Nephrotic syndrome.
Contributors







For the medical students/student doctors
Renal hypertension
Renal arterial hypertension is a symptomatic hypertension caused by the affection of the kidneys or renal vessels and upset renal mechanism of arterial pressure regulation. Among all cases of arterial hypertension, renal hypertension makes about 10—15 per cent.
Many diseases of the kidneys, in the first instance acute and chronic glomerulonephritis, pyelonephritis, nephrosclerosis and various affections of the renal blood vessels are attended by elevated arterial pressure. This is underlined by the important role that the kidneys play in the regulation of arterial pressure. The juxtaglomerular apparatus of the kidneys, which is an accumulation of special cells at the vascular pole of the glomerulus, the point where the artery nears the proximal end of the distal convoluted tubule, produces renin in the presence of ischaemia of the renal parenchyma. Renin acts on the liver-produced hypertensinogen, which is the conversion of a2-globulin of plasma, to convert it into angiotensinogen. This converted enzymatically into angiotensin (hypertensin).
At later stages, dystrophic changes occur in the myocardium because vascularization lags behind the growth of the muscle weight to account for the deficient blood supply; next, cardiosclerosis develops. At the time, atherosclerosis of the coronary vessels may develop due to upsemetabolism, which is characteristic for arterial hypertension and other renal diseases attended by the nephrotic syndrome. The coi disease impairs blood supply to the myocardium to an even greater pain, like that of angina pectoris often occurs. Further progress of diseases can provoke circulatory insufficiency, urtain acute diseases of the kidneys attended by a rapid and pronounc-:vation of the arterial pressure, mainly acute glomerulonephritis, are Jed by the condition at which the left ventricle is not hypertrophied >h to compensate for the markedly increased load. Acute ventricular e can therefore develop. It is manifested by attacks of cardiac asthma ven by a lung oedema.
It follows therefore that in certain kidney diseases, the renal hypertension syndrome can be of primary significance in the clinical picture of the disease and can be decisive for its course and outcome.
Renal eclampsia
Eclampsia (Gk ek, lampein to flash) usually develops in acute diffuse glomerulonephritis, but can also arise in aggravated chronicglomerulonephritis and nephropathy of pregnancy. The pathogenesis of eclampsia is largely underlain by increased intracranial pressure, Oedema of the cerebral tissue and cerebral angiospasm. Eclampsia in all these con ditions usually arises in pronounced oedema and increased arterial pressure. Attacks of the disease are provoked by salted food and excess liquid.
The first signs of approaching eclampsia are often unusual somnolence and flaccidity. These are followed by severe headache, vomiting, temporary blindness (amaurosis), aphasia, transient paralysis, mental confu sion, and a rapid rise in the arterial pressure. Convulsions develop unexpectedly, sometimes after uttering a cry, or after a noisy deep inhalation. The convulsions are first strong tonic spasms, which are followed (in 0.5-1.5 minutes) by strong clonic contractions. Less frequently only twitching of some muscles is observed. The face becomes cyanotic, the neck veins swell, the eyes turn aside or roll up, the tongue is bitten, and foam emerges from the mouth. The pupils are dilated and do not respond to light; the eyeballs are firm. The pulseis tense, slow, the arterial pressure increases. The body temperature rises in frequent attacks. Involuntary defaecation and urination often occur.
Attacks of renal eclampsia usually last for a few minutes, rarely for longer time. Eclampsia occurs in some cases as a series of two oi; three attacks which follow one another. The patient then calms down to stupor, deep sopor or coma; consciousness is then regained. After recovery from the state of stupor the patient sometimes remains in amaurosis (blindness of the central origin) and aphasia (mutism).
This is the classical picture of an eclampsia attack. But it should be-remembered that attacks of eclampsia may also be atypical; they may occur without loss of consciousness or occur in an obliterated form, as a transient aphasia, amaurosis, and mild muscular twitching.
Renal eclampsia should be differentiated from convulsions of other origin. Convulsions in eclampsia are the same as in epilepsy (a congenital or post-traumatic nervous disease). But oedema or other signs of renal insufficiency are absent in epilepsy; attacks of convulsions usually occur in the course of many years. Convulsions develop also in uraemic coma, but the patient has a typical anamnesis in this case (chronic renal insufficiency), signs of uraemic toxicosis, slow (in the course of several days) development of the convulsive state; the character of convulsions is different as well: convulsions develop as slight fibrillary twitchings.
Treatment. An attack of renal eclampsia can be removed immediately by a suboccipital or cerebrospinal puncture with extraction of a small portion of the cerebrospinal fluid: the intracranial pressure decreases and the patient regains consciousness. The extraordinary efficacy of cerebrospinal puncture proves the importance of increased intracranial pressure for the pathogenesis of attacks of renal eclampsia. Phlebotomy and intravenous injection of magnesium sulphate (10 ml of a 25 per cent solution) remove attacks of eclampsia, effectively decrease the arterial pressure and lessen cerebral oedema.