How to Care for a Patient on Ventilator?
Ventilator

What is a Ventilator?
A ventilator is a machine that gives breath to a person who has lost ability to breathe by himself due to some diseases.
Ventilator also assists the breathing in people with “difficulty breathing” by removing excess carbon dioxide from the lungs and supplementing oxygen to the lungs.
Where is Ventilator Used?
Usually in hospitals, ventilators are used in the
- emergency departments
- acute care settings or intensive care units and
- operation theatres.
As soon as the patient is put on ventilator, the health care team start thinking of ways to take the patient off ventilator by correcting basic illnesses and the symptoms developed during the course. In other words, ventilator therapy is meant only for a short period.
Ventilator in Operation Theatres
If the ventilator was used to support breathing during a surgery and general anaesthesia, it is usually removed once the patient stabilises and comes out of anaesthesia. This means that ventilator helps in keeping the patient safe and his breathing is not impaired or arrested by the effect of drugs used in anaesthesia. However, depending on the type of surgery and the disease condition, the patient may be kept on the ventilator for a few days to few hours more.
Ventilator in Intensive Care Units
In the intensive care units patients suffering from serious lung diseases like pneumonia, acute respiratory distress syndrome and other serious illnesses like poisoning, head injury etc. are kept on ventilator. The process of assisting breaths with the help of ventilator is known as ventilation.
When is a Ventilator Used?
Normally, our lungs take in oxygen from the air and give out carbon dioxide in a process called ventilation. The process is so automatic that we need not put any special effort and it happens all the time without awareness.
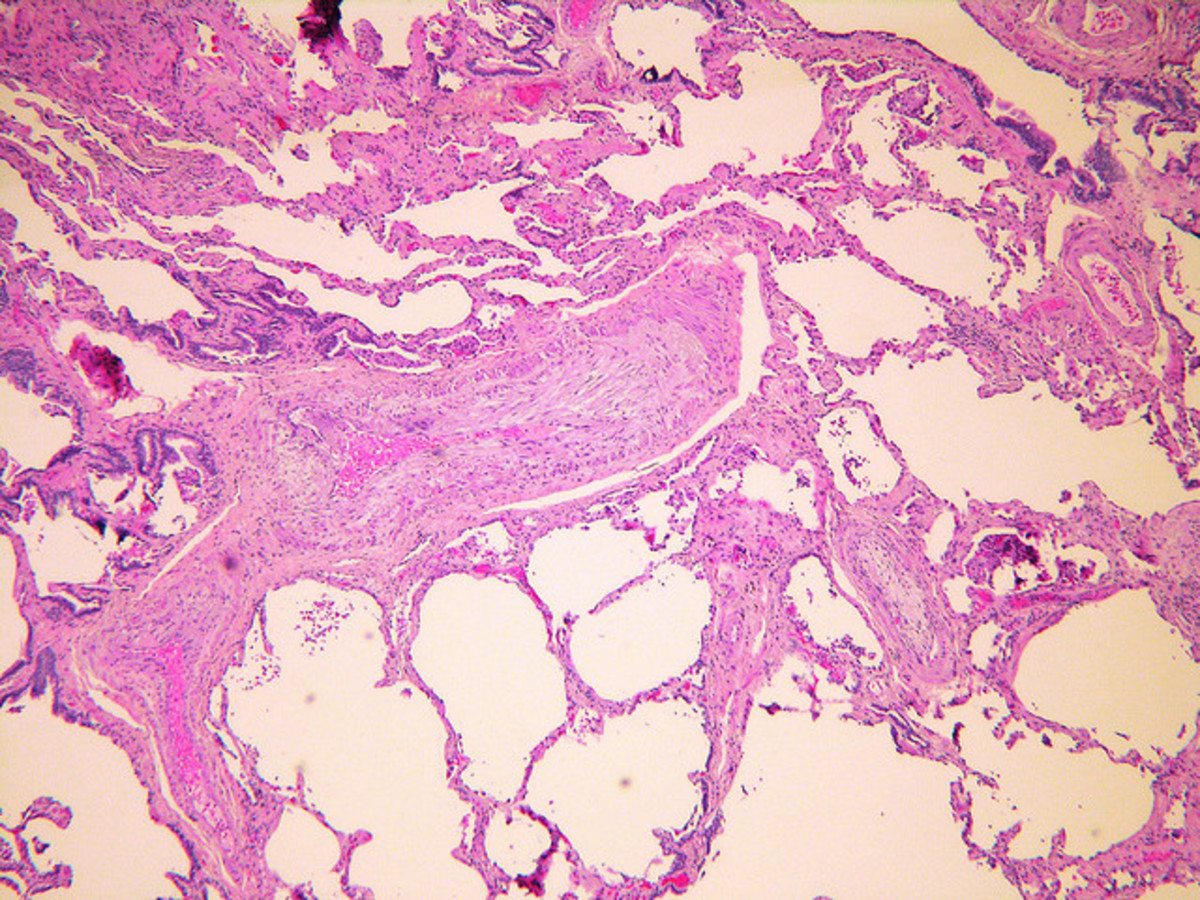
But for people suffering from diseases like asthma, obstruction to the airways, pneumonia and other serious inflammations of the lung, the breathing becomes laboured. There is increased work of breathing which can lead to respiratory muscle fatigue.
There can also be stoppage of breathing or respiratory failure due to serious lung diseases or brain damage and high spinal cord injuries.
On all these occasions, a ventilator acts as a support for breathing, by giving oxygen to the lungs and removing carbon dioxide till the patient recovers.
How is the Need for Ventilator Identified?
- For surgeries, the need of a ventilator is anticipated because of the time required to complete the surgery, the need for general anaesthesia and because of the effect of drugs used in general anaesthesia on respiration.
- In an acute care setting, as soon as the patient is admitted, he will be connected to a monitor which can read the pulse rate, respiratory rate, blood pressure, the level of oxygen in the blood etc.
- If the clinical data suggests problems with ventilation and respiration (i.e., restlessness, difficulty breathing, confusion, anxiety, increased respiratory rate, increased heart rate, and excessive sweating), blood sample from patient’s artery is taken for blood gas analysis.
- If the oxygen saturation in the arterial blood is very less or if the carbon dioxide level is more than expected, the patient is put on ventilator with supplemental oxygen.
How is a Patient Put On Ventilator?
The ventilator receives the gas supply; both oxygen and atmospheric air from a wall supply in the intensive care unit or operation theatre. With the help of knobs on the ventilator, the respiratory rate, amount of oxygen, the time for inspiration and expiration, and some other parameters in providing ventilation to the patient can be adjusted.
The patient usually will have a tube (endotracheal tube) placed in to the mouth or nose and down into the trachea or windpipe. The process of inserting this pipe is called endotracheal intubation. If the patient requires ventilator support for a long period, a surgical hole is placed in the neck and a tube (tracheostomy tube) is inserted through that hole.
Ventilator tubing is connected to an endotracheal tube or tracheostomy tube. Ventilator delivers oxygen into the patient’s respiratory tract. Varying levels of oxygen can be delivered based on patient’s requirements. Ventilator can deliver higher levels of oxygen to the patient's system than delivered by mask or nasal cannula. Using ventilator, varying pressures can be applied to the patient’s system to enhance gas exchange between blood and alveoli. Excess amount of secretions can be suctioned out using a suction catheter from the endotracheal or tracheostomy tube.
Anesthesiologist using Glidescope video laryngoscope to intubate the trachea of a morbidly obese patient with challenging airway anatomy.

How are the Patients On Ventilator Cared For?
Continuous monitoring of patient’s vital parameters like heart rate, respiratory rate, blood pressure, oxygen saturation etc. will be done with the help of a monitor.
Arterial blood gases are assessed and necessary modification to the ventilator settings done from time to time. Chest X-rays are taken to check the position of the endotracheal tube as well as air entry into the lungs. Chest x –rays will also speak about the progress of lung disease.
Nurses will also give position change, bed bath, back care and passive exercises to the extremities to prevent complications like bedsore, blood clotting in the legs and constipation.
As mentioned earlier, patient on ventilator is continuously assessed for readiness to extubate as well
Drugs and procedures to correct the disease process will go on as per schedule.
How can a Patient On Ventilator Communicate?
Patients may be slightly sedated depending on the need. When we prepare the patient for extubation, the amount of sedation is reduced and stopped.
Patients on ventilator cannot talk as the endotracheal tube passes between the vocal cords into the windpipe. Patients who are awake will be able to communicate using sign language or with the help of a writing board or paper and pencil.
Patients with tracheostomy can often communicate with the help of a speaking valve.
How do People on Ventilators Eat?
Do you think patients on ventilators feel hungry and ask for food?
How does a Patient On Ventilator Eat?
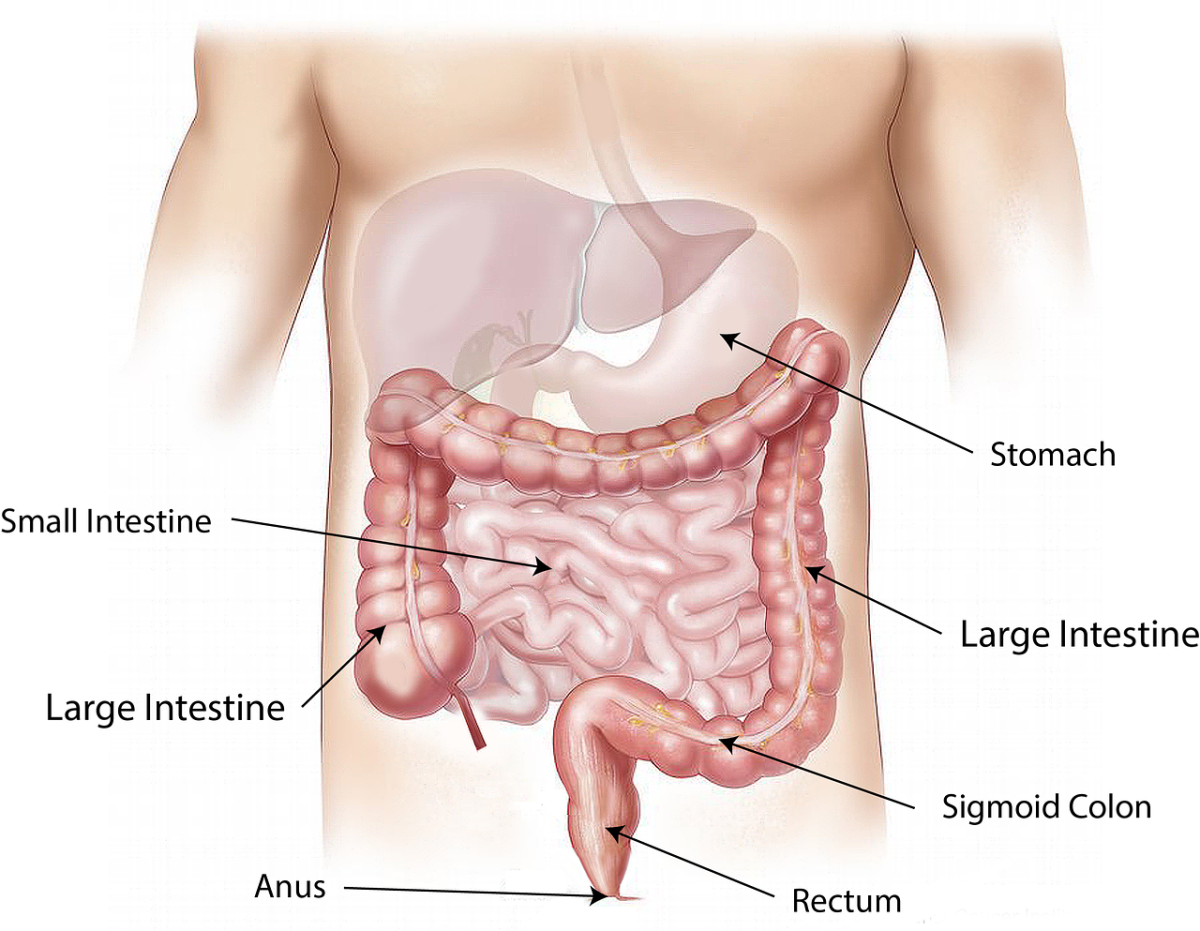
Patients on ventilator may not be able to eat by mouth as it is the most common route for endotracheal intubation.
They will be usually fed through a nasal tube that goes into the stomach. In very severe illnesses, feeding formulas are given through the veins.
What are the Usual Reactions of Patients on Ventilator?
It is very difficult for anyone to be in a critical care unit because the environment is so very restricting and unfamiliar for a person who is getting admitted for the first time into the unit.
Patients feel helpless and may think that their privacy is interfered too often.
If the person is conscious and awake, they usually do not like keeping a tube in their mouth or nose. In addition there will be many other types of tubing like intravenous lines, nasogastric tube, urinary catheter etc. Sometimes the patient may try to breathe out when the ventilator tries to push the air in. This may result in fighting against the ventilator and anxiety and panic in the patient.
Are there any Risks Involved while a Patient is On Ventilator?
Doctors and nurses weigh the risks and benefits for keeping a patient on ventilator. In an acute care setting, endotracheal intubation is often an emergency procedure to save the life of the patient. However, there are certain risks like the development of lung injury, lung infection, a reduction in blood pressure and other complications related to the patient’s disease. Some patients can be extubated within hours whereas for some it may take days. Very sick patients may not come out of ventilator and in them it may help only to postpone death.
How is a Patient Taken Off Ventilator?
The process of taking a patient off the ventilator is known as weaning. Doctors and nurses think of weaning the moment a patient is put on ventilator. As the patient improves spontaneous breathing trials are given still with the endotracheal tube in place. Once the weaning trial is successful, the ventilator is disconnected and the endotracheal tube is removed. Patient may continue to receive oxygen by mask. Continuous monitoring of the arterial blood gases is done to ensure safety. The patient has to be repeatedly called and asked to take breath because they may sleep off because of the effect of medications.