Women and Heart Attacks - Misdiagnosed Due to Gender Differences, Bias
The reason I came so close to death was because I am a woman.
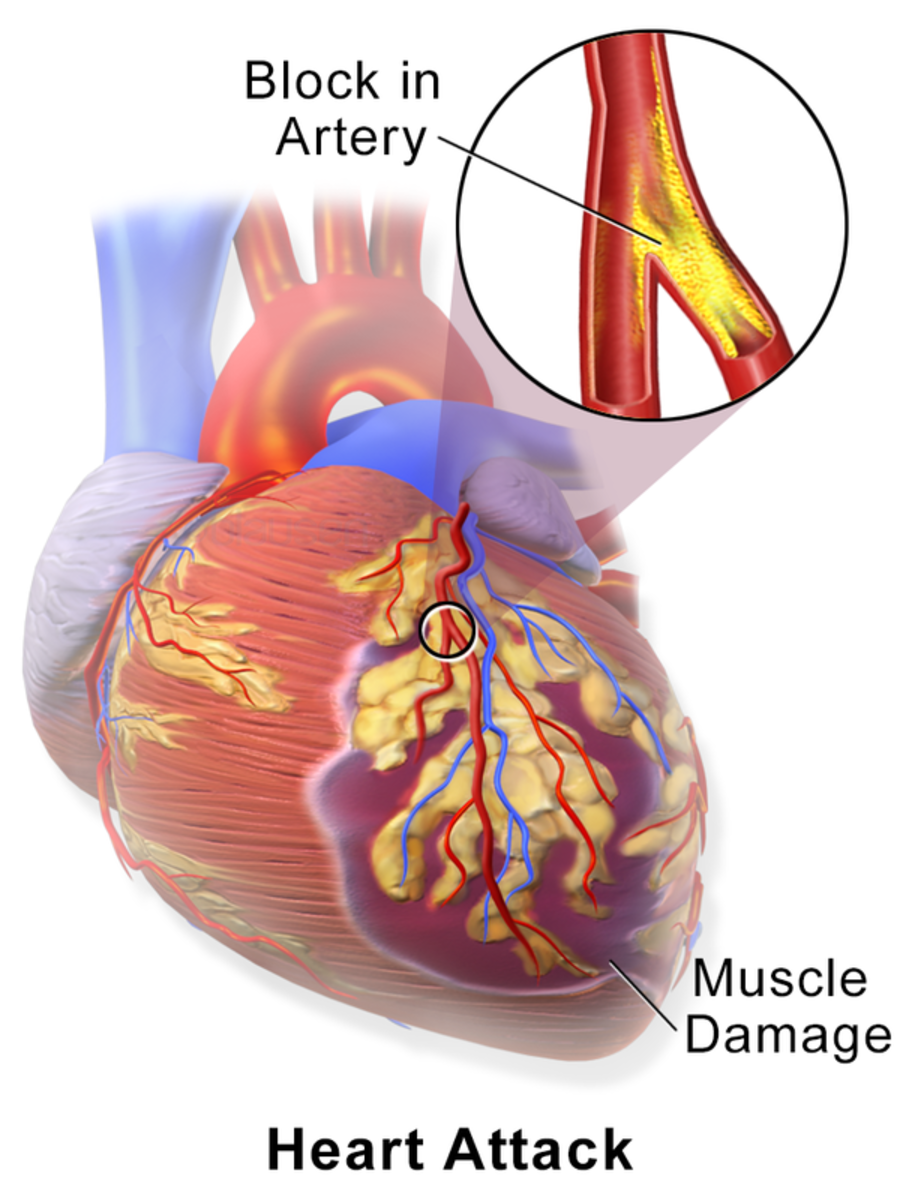
The Three Coronary Arteries
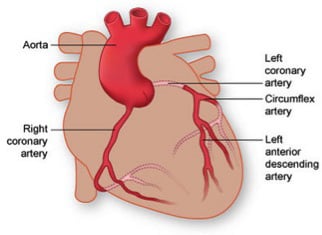
The Widow Maker Heart Attack Explained
Commonly referred to as the Widow Maker, this type of heart attack occurs when the Left Anterior Descending (LAD) artery has an occlusion at the beginning of the vessel. The LAD supplies blood to the front and main wall of the heart. If blood flow is not restored in time, the heart muscle (myocardium) stops working because blood flow is stopped or severely decreased, and the myocardium begins to die.
This is a problem with deadly consequences for women.
Two weeks before my 41st birthday, I found myself in the emergency room surrounded by a large medical team. I was told to call my family members. I was having a massive heart attack and was informed they were preparing for the worst.
When all was said and done, it was a miracle I survived. I had what is referred to as the Widowmaker heart attack. This type of heart attack is King of all heart attacks. It was given the name "Widowmaker" because of the low survival rate in men. Women under the age of 50 are twice as likely than men to die during a heart attack.
Although modern medicine now realizes that women suffer from heart disease just as frequently as men and heart disease is the number one killer of both sexes, the reason I came so close to death was because I am a woman.
Common Signs of a Heart Attack in Women
- Discomfort, tightness,uncomfortable pressure, fullness, squeezing, burning in the center of the chest or slightly to the left of center lasting more than a few minutes, or comes and goes; however, women are more likely than men to have NO COMPLAINTS of chest pain during a heart attack
- Crushing chest pain
- Pressure or pain that spreads to the shoulders, neck, upper and mid back, jaw, or pain in one or both arms
- Dizziness, nausea, vomiting
- Clammy sweats, heart flutters, palpitations, or paleness
- Unexplained feelings of anxiety, fatigue or weakness - with or without exertion
- Stomach or abdominal pain, indigestion, loss of appetite
- Shortness of breath and difficulty breathing
Nearly 20 Years of Research...Ignored
It is common knowledge within the medical community that men and women frequently present with different symptoms when having a heart attack. Over 40% of women having heart attacks do not present with chest pain (link below--JAMA), rather, they present with jaw, shoulder, and/or back pain, and even nausea. Many women have pain that radiates down the right arm, rather than the classic, left-sided arm pain. These are just a few of the physical differences. In addition, diagnostic tests (EKG's, stress tests, etc.) are not as reliable for diagnosing a heart attack and/or coronary artery blockages for women as they are for men.
Despite research for the last 20 years concluding there are significant differences between men and women in regards to heart disease and heart attacks, physicians and emergency rooms continue to use the same protocol to diagnose both sexes when being evaluated for chest pain and/or a possible heart attack. This is a problem with deadly consequences for women.
Women are less likely to experience chest pain during a heart attack.
Observation and study included over 1.1 million patients admitted for myocardial infarction/heart attack (men outnumbered women by 200,000) between the years 1994-2006. Women were less likely to experience chest pain during a heart attack compared to their male counterparts (42% versus 30%).
- JAMA Network | JAMA | Association of Age and Sex With Myocardial Infarction Symptom Presentation and
Research from JAMA — Association of Age and Sex With Myocardial Infarction Symptom Presentation and In-Hospital Mortality
Coronary Artery Spasms and Microvascular Disease, More Common With Women, Cause Heart Attacks
- Misdiagnosed: women’s coronary microvascular and spasm pain | Heart Sisters
Circulation. 2006 Oct 10;114(15):1565-71. Epub 2006 Oct 2. Evaluation Studies; Multicenter Study; Research Support, Non-U.S. Gov't
A study concluded that patients who presented to the emergency department with acute cardiac ischemia were more likely not to be hospitalized if they were women
- Missed Diagnoses of Acute Cardiac Ischemia in the Emergency Department — NEJM
Original Article from The New England Journal of Medicine — Missed Diagnoses of Acute Cardiac Ischemia in the Emergency Department
Common Misdiagnoses for Women Suffering Heart Attacks
The prevalence of women being misdiagnosed for heart disease and during an acute heart attack is disturbing. Study after study indicates that women are frequently being sent home from emergency rooms and physician's offices despite complaining of chest pain. Women are commonly diagnosed with panic/anxiety attacks (studies conclude a gender bias in addition to gender differences--women are more likely to be diagnosed with panic attacks), heartburn and/or GERD, and musculoskeletal inflammation even when presenting with "classic" heart attack symptoms.
If I had known any of this information, I would have been much more assertive. I would have taken more control over my healthcare (or lack of healthcare), but I didn't have this information and nearly died because of it. This does NOT, in any way, take blame away from the medical staff and placing it, even partially, onto myself. Every minute counts when someone is having a heart attack, because every minute results with more damage to the heart.
Your "Normal" EKG May Not Be Normal - When Abnormalities Are Missed
A retrospective study of patients with confirmed heart attacks concluded that ER physicians missed significant abnormalities in 12% of the patients. This resulted with delayed treatment as well as doubled the mortality rate compared to patients without missed EKG abnormalities.
Cold Air Can Cause Chest Pain in People With Coronary Artery Disease
- Cold Weather and Cardiovascular Disease
The American Heart Association explains the potentially dangerous link between cold weather and heart conditions.
Day One: My First Visit Seeking Treatment for Chest Pain
On a Wednesday, I woke up at four in the morning with crushing chest pain in the center of my chest. With a history of heartburn and my doctor doubling my dose of antacids a few months prior, I thought that I was suffering from the most severe episode of heartburn, especially given the fact the night prior I had banana bread topped with butter. I knew that butter was a big no-no for me, but I just couldn't resist.
Six hours later, I drove myself to urgent care. I reported the above as well as the pain now being to the left side of my chest, the pain coming and going in both frequency and intensity along with pain ranging anywhere from a 3 to a 10 or off the charts, and left-sided arm pain that radiated from my shoulder down the entire left arm.
An EKG was performed--several, actually--as I was informed that I needed to keep still because the EKG was "all over the place". It was pointed out by the technician that the cold air from the air vent might be causing the EKG to go haywire, and she stated she informed the doctor I was underneath the air vent.
Five strips finally resulted with a more acceptable and more readable result which showed slight changes from six months prior. "It looks a little funny, but it isn't concerning."
GI Cocktail
A GI cocktail is a mixture of antacids and a pain killer (usually lidocaine) that is often given to patients with suspected heartburn or GERD in order to stop the pain.
Purpose of the Chest X-Ray When Evaluating Chest Pain
A chest x-ray does not show whether or not a patient is having a heart attack. A chest x-ray will show if the heart is smaller or larger than it should be. A chest x-ray will also examine the lungs and show if the patient has pneumonia or a collapsed lung. A chest x-ray during an evaluation for chest pain is used to rule out other causes of chest pain.
Here's a GI cocktail and a pain reliever for your chest pain.
I was then given a GI cocktail despite being adamant that the chest pain was in a different location than my heartburn. Twenty minutes later, after the antacid concoction had not helped and I was now in tears from the chest pain, I was given an injection containing an anti-inflammatory and sent for a chest x-ray which was normal.
About 45 minutes later, I was put in a different room with the examination table away from the air-conditioning vent. Slowly, the chest pain became less debilitating, although I indicated it did not completely go away. I did not realize until the next day that cold air would cause my chest pain to become excruciating. I was sent home indicating that the problem was musculoskeletal because the injection had obviously worked. I continued to have pain that would wax and wane all through the night and awoke several times crying due to the pain.
Day Two: My Second Visit Seeking Treatment for Chest Pain
Thursday morning brought chilly temperatures and, bright and early, I left for a follow-up appointment with my primary physician. On the way to the office, the pain was so severe I was unsure if I could continue to drive. By the time I made it into the exam room, yet again, the pain decreased in severity. I complained of continued chest pain, continued pain radiating down my left arm and feeling like my entire body was wiped of energy. I was short of breath during the office visit. My doctor did not look at the EKG but did mention the chart note indicating "slight EKG changes".
My diagnosis, again, was musculoskeletal. I did not ask what, precisely, that meant. I was given a prescription for an anti-inflammatory. My doctor did indicate that due to a very strong family history of heart disease, including an uncle who died at 42 from a massive heart attack, that she would like me to have a stress test that day. I said that there was no way I could tolerate a treadmill test that day.
Leaving the office and entering the chilled air, the chest pain, again, became nearly intolerable. I went home, bundled up, and fell asleep for hours. When I awoke in the hot afternoon, the pain had lessened, but I was extremely fatigued. I spoke with my mother about how the colder air seemed to worsen the chest pain and we both wondered if arthritis could be present in the sternum, as I had arthritis in my knees and back. We thought that could be a possibility, especially given the fact I had taken notice that cold air seemed to make the pain worse. When evening settled in and the temperature dropped, I again struggled with crushing chest pain that woke me several times in the middle of the night.
Day Three: It Must Be Musculoskeletal
The next morning it was warm and temperatures reached the 100 degree mark. I had a job interview. The chest pain was completely absent, although I continued to suffer from shortness of breath and extreme fatigue. I figured the anti-inflammatory prescription was obviously working.
That evening, the temperature dropped to cool, and the nagging pain in my chest began again.
Blood Tests - Cardiac Enzymes
There are enzymes within the heart muscle that will leak into the blood, over a period of hours, when the heart muscle has been damaged:
Troponin I and Troponin T: Unfortunately it can take up to 12 hours AFTER a heart attack for these tests to show any elevation of enzymes; therefore, it is important that these blood tests be performed several times, with the last test being performed 12 hours AFTER the onset of symptoms. If, AFTER 12 hours, these enzymes do not show up in the blood, it is unlikely that someone suffered from a heart attack. This means that negative results LESS THAN 12 HOURS AFTER THE ONSET OF SYMPTOMS DOES NOT RULE OUT A HEART ATTACK.
Creatine kinase (CK): CK testing will not identify a heart attack that occurred over 72 hours previously. Elevation of CK should occur within 3-4 hours after a heart attack with peak levels around 10-24 hours after a heart attack.
CK-MB: This enzyme can be found within the heart, but it is also found in other organs of the body like the small intestines and the uterus. High levels of CK-MB can also be used to determine other conditions such as renal failure, musculoskeletal damage, and muscular dystrophy, so it is unreliable as a sole cardiac marker to diagnose a heart attack.
Myoglobin: This is another protein that is present in the heart that is also present in other locations: skeletal muscles; kidneys. Again, this test alone, is unable to identify a heart attack because it is not specific for heart damage; however, myoglobin levels will begin to rise sooner than troponin levels at 2-3 hours.
IT IS IMPORTANT THAT ALL OF THESE TESTS BE RUN WHEN PRESENTING WITH CHEST PAIN WHEN THE ONSET OF SYMPTOMS ARE LESS THAN 12 HOURS. NOT ONE SINGLE TEST USED ALONE IS AN INDICATOR OF A HEART ATTACK.
Day Four: Third Time Seeking Treatment for Chest Pain. PREPARE FOR THE WORST
When I woke Saturday morning, I was back in bed within a few hours due to sheer exhaustion. The weather was extremely warm. That afternoon my husband turned the fan on in the bedroom. I immediately woke up clutching at my chest. Although I was dripping with sweat, I was unable to tolerate any air being directed at me.
Several hours later, my brother came over to pick up my husband. They had tickets to a hockey game in Los Angeles--60 miles away. The only reason I woke up was because my dog was barking and running marathons around the house -- she was so excited to see my brother. If not for her waking me, I would have stayed in bed and died.
I forced myself to stay awake and watch some television, as I had slept the entire day away.
Then, I did the dishes.
This minimal task resulted with me breaking out in a sweat, chest pain with pain radiating down the left side of my arm, breathing as if I had run a marathon, and feeling as if I was going to collapse. It was obviously time for me to go back to bed.
When I walked into the bedroom, I envisioned myself on the bed and my husband entering the bedroom. The dog was jumping on me trying to get to my husband, and I didn't move at all. My husband pushed our dog off the bed and tried to shake me awake.
I turned around, called my mother, and told her I was going to the ER. We argued briefly about calling an ambulance, and I indicated that I felt stupid doing that since I was told, twice, that I had obvious inflammation in my chest.
Upon arrival I had an EKG within ten minutes. Twenty minutes later I had a chest x-ray. And nearly an hour after arriving, I finally had lab work performed. After each test I was sent to the waiting room. I was in obvious distress. I clutched at my chest, I was having difficulty breathing, and I was sweating.
It had been more than two hours since arriving at the emergency room. I requested to use the check-in desk's phone to call my mother (I don't have a cell).
"Mom, I must be fine. I'm not in the operating room--they did an EKG two hours ago, and I'm still sitting in the waiting room."
As I was toying with the idea of leaving in order to go home to my bed, I heard a physician yelling at staff that a patient had been sitting in the waiting room for two hours while having a massive heart attack.
It wasn't me. Or was it?
Ten minutes later, I had IVs in both arms, a nitro patch on my chest directly over my heart, I was hooked up to an EKG monitor, and I was on the phone with my mother relaying the severity of my heart attack. They were awaiting for the invasive cardiologist to arrive at the hospital, and I was to have an emergency surgery for stent placement. I was panicked.
I called my brother's cell phone and spoke to my husband in a very calm voice relaying I was having a heart attack and needed surgery, so it would be really great if he could be there before I was taken into the operating room. An "I love you" three times. They were stuck in traffic.
My husband arrived two minutes before I was wheeled into surgery. He looked like death. His tanned face was pale, his eyes were wide with worry and he had a pained look. I was going to survive...for him. If I didn't, I knew that pained look would remain on his face for years. The thought of me being the cause of all of his pain was incomprehensible, and I wasn't going to do that to him.
After surgery, the cardiologist told my family that, at best, I had twenty minutes remaining to live by the time the stent was placed into my fully occluded LAD. I had been having a heart attack for four days. My heart attack was in March of 2015. Currently, I am suffering the effects of having a four-day heart attack. When time and energy permits, I will explain these debilitating and life-altering effects that has decreased my quality of life forever.
Every minute counts when someone is having a heart attack. Every. Single. Minute.
What Could Have Been Done Differently? A LOT!
I did speak with an ER physician after I was discharged from the hospital, as I had written a request to have a physician call me and explain why, exactly, I had been sitting in the waiting room for over two hours while having a heart attack.
The response I received: We are just understanding the differences between men and women and how they present differently when having a heart attack. At the time your EKG was done, you were receiving sufficient blood flow to your heart. If, at any time, labs were drawn, including the Wednesday and Thursday, they would have been able to tell that you were in the midst of a heart attack. Even if you had been put on an EKG monitor instead of a standard EKG strip, it would have showed within a few minutes that your heart was not receiving sufficient blood flow. A 15 or 30 second strip wasn't long enough to detect your heart attack.
I have a lot of questions that still remain today. The biggest question I have, of course, is if the ER physician recognizes that men and women present differently when having a heart attack, why did the protocol remain the same? Why, as the physician indicated, was I not put on an EKG monitor? Why was lab work the last test performed rather than being done immediately?
Lastly, and most importantly, how many women have died despite medical professionals knowing that these differences exist? The physician I spoke with knew what should have been done differently simply because I am a woman, yet none of it was protocol.
Use My Story as Knowledge
- If you are having chest pain, do not allow your physicians to be so quick to dismiss you with: Panic/stress/anxiety; heartburn/GERD; musculoskeletal issues.
- Demand that medical staff pursue further evaluation if EKG results show any "slight abnormalities". This includes an EKG monitor as well as all relevant lab tests.
- If your EKG is "all over the place" or there is trouble obtaining a readable strip, and/or the technician tells you to stay still, and you are staying still, allow this to serve as a BIG, RED FLAG.
- If you are at a hospital being evaluated for chest pain, INSIST that you be put on an EKG monitor. If you are at a physician's office or an urgent care, make this same request.
- If you are at a hospital being evaluated for chest pain, demand the lab work be performed prior to the chest x-ray. If you are at an urgent care facility or at your physician's office, and even if the EKG is normal, demand that lab work be performed as a STAT (immediate testing and results within 1-2 hours).
- Listen to your body. If your body is telling you something is wrong and your physician says otherwise, stand your ground and demand that all of the above be performed. Doctors are not always right. Doctors do make mistakes, and this is especially true for women who are having heart attacks.
© 2015 Jenifer L