DiGeorge Syndrome – Pictures, Life Expectancy, Symptoms, Causes, Treatment
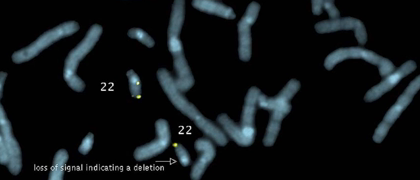
Also referred to as 22q11.2 deletion syndrome, DiGeorge syndrome is an abnormal condition caused due to errors in chromosome 22 and is characterized by developmental deficits in different body systems.
DiGeorge syndrome causes a varied of medical problems such as poor functioning of the immune system, cardiac anomalies, complications arising out of low blood calcium levels, a cleft palate, and behavioral abnormalities, etc.
The degree of severity and the number of problems related to DiGeorge syndrome differs widely. A majority of patients with DiGeorge syndrome require treatment by specialists from many different fields.
Before scientists found out the defect in chromosome 22, the condition was known by many names such as velocardiofacial syndrome and DiGeorge syndrome, etc. Currently, medical professionals generally refer to the condition as 22q11.2 deletion syndrome as it is a more precise description of the disorder. However, older names are still in use.
Symptoms of DiGeorge syndrome
The signs and symptoms associated with DiGeorge syndrome can differ considerably in severity and type. Such variations are dependent on the degree of defects and the body systems that are affected. A few symptoms may be visible from birth, while others may not be noticed till late infancy or early childhood.
Some of the common signs and symptoms of DiGeorge syndrome are listed below:
- Cyanosis or poor flow of oxygen-abundant blood can result in bluish skin
- Inability to grow and flourish
- Easy exhaustion or weakness
- Absence of any weight gain
- Breathlessness or other breathing difficulties
- Poor muscle tone
- Peculiar facial characteristics like wide-set eyes, low-set and small ears, hooded eyes, a comparatively long face, and/or a thin groove in the upper lip
- Spasms or twitching of the arms, hands, around the mouth, and/or throat
- Feeding problems
- Persistent infections
- Delays in reaching developmental milestones such as rolling over, sitting up, crawling, etc.
- Difficulties or delays in learning
- Delays in speech formation
- Cleft palate, or an opening in the roof of the mouth, or other anomalies of the palate
Medical Complications associated with DiGeorge syndrome:
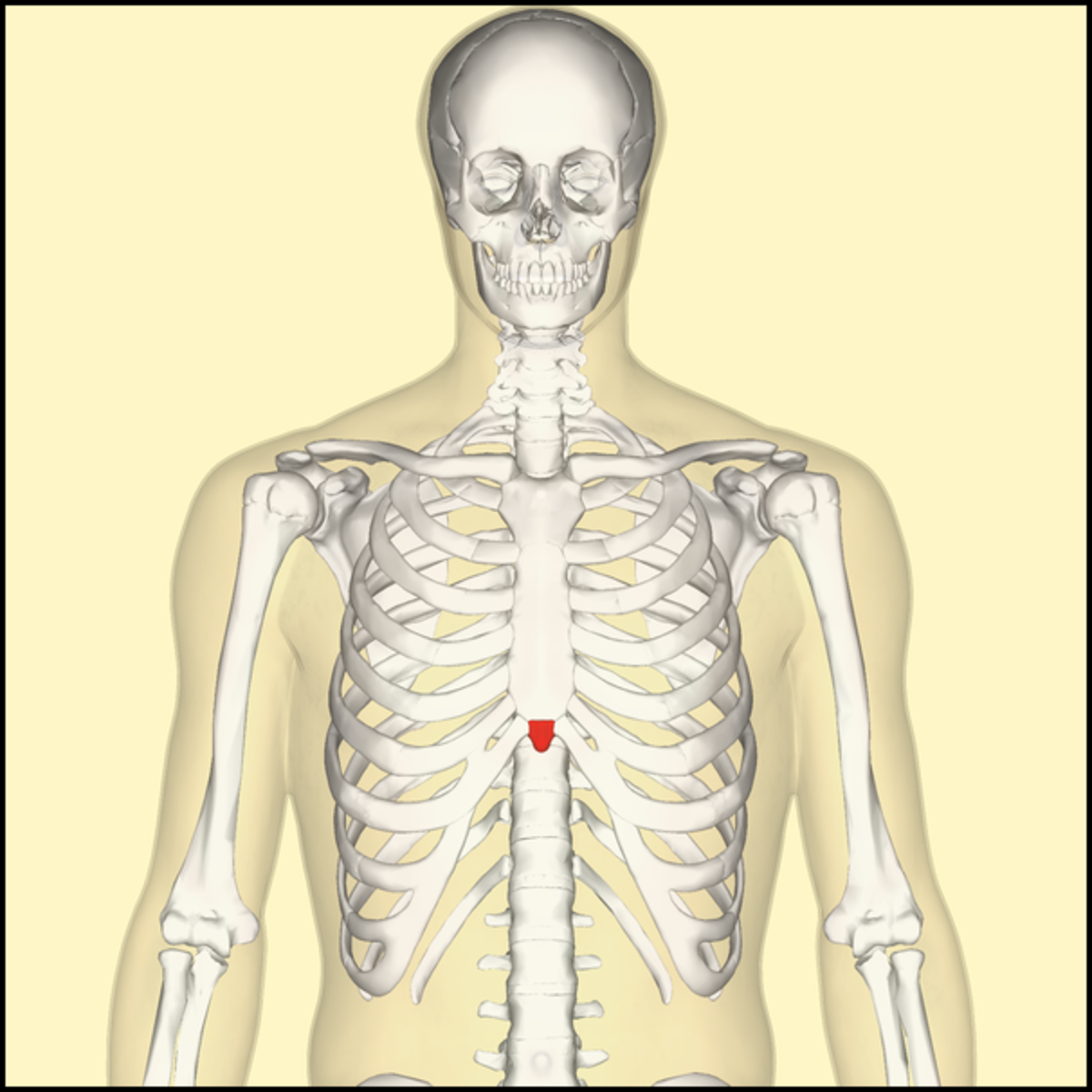
- The parathyroid glands maintain the ideal levels of phosphorus and calcium in the body by regulating the production of PTH or parathyroid hormone. Patients of DiGeorge syndrome may have smaller than normal parathyroid glands, causing reduced secretion of PTH, leading to hypoparathyroidism. This in turn causes low calcium and high phosphorus levels in blood.
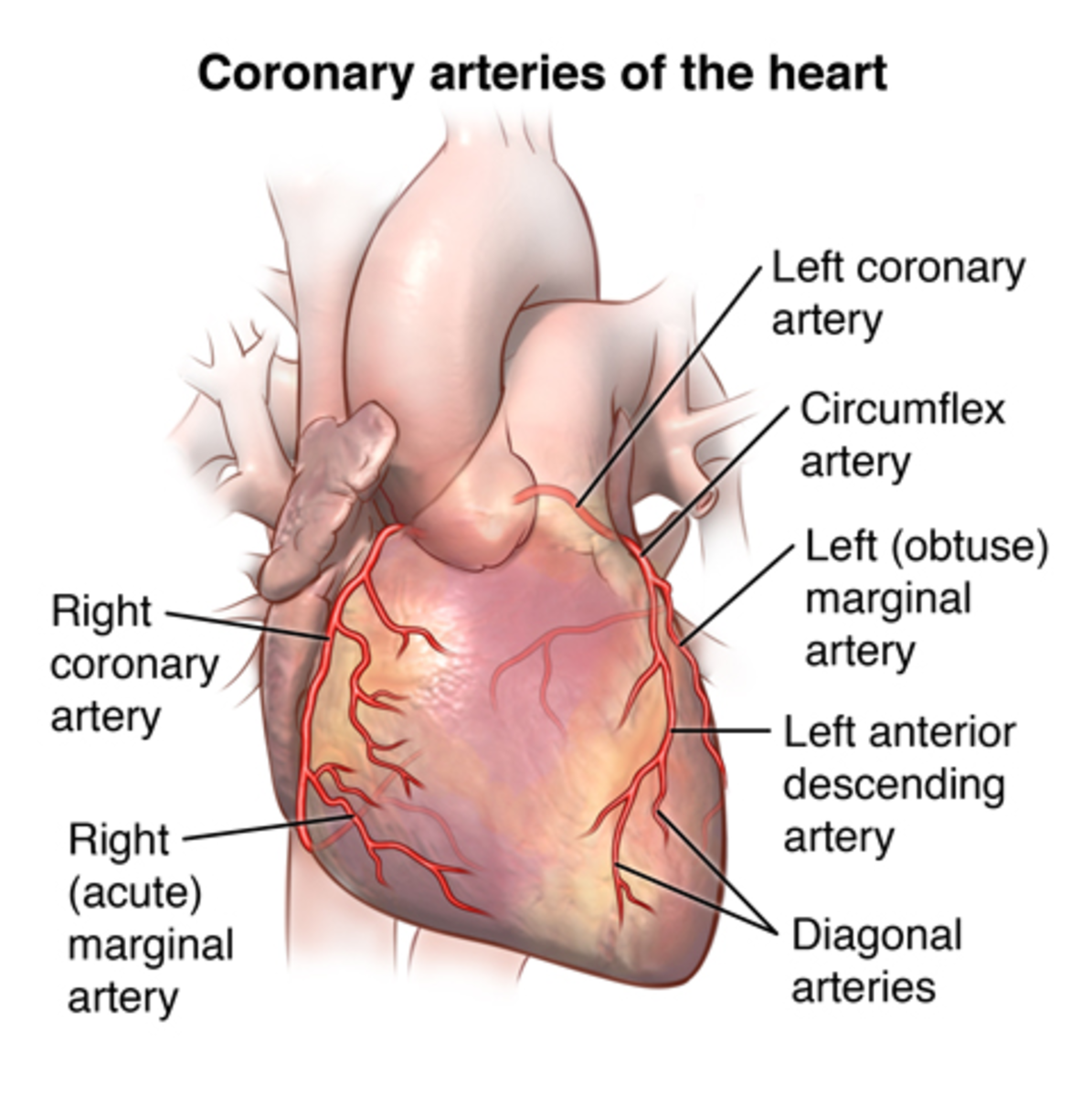
- Cardiac defects such as truncus arteriosus, ventricular septal defect, and tetralogy of Fallot may occur in DiGeorge syndrome patients resulting in deficient flow of oxygen-rich blood across the body.
- Cleft palate is one of the most common complications associated with DiGeorge syndrome. This along with other less noticeable palate anomalies can cause swallowing difficulties or speech defects.
- In infants, the thymus gland produces T-cells which help fight off infections. As children grow older, the immune system takes over the function of fighting-off invading pathogens. Infants with DiGeorge syndrome may have absent or smaller than normal thymus gland, thereby increasing the risk to frequent and serious infections.
- Reduced immune function can also increase the susceptibility to autoimmune disorders such as Graves' disease and rheumatoid arthritis.
- The chromosomal deletion associated with DiGeorge syndrome can lead to abnormal brain development and function. This can cause social, learning, behavioral, or developmental problems. Affected children may suffer from ADHD, autism or autism-related conditions, while as adults they may be prone to mental health issues like anxiety disorders, depression, schizophrenia, and/or other psychiatric conditions.
- Patients of DiGeorge syndrome are also at risk to developing other health complications such as poor vision, impairment of hearing, a shorter stature, and poor functioning of the kidneys.
Causes of DiGeorge syndrome
DiGeorge syndrome is caused due to the deletion of a section of chromosome 22. Every individual has 2 copies of the chromosome 22, and each copy is passed on by the father and the mother. This chromosome consists of approximately 500 to 800 genes.
In individuals affected by DiGeorge syndrome, a specific segment in one copy of chromosome 22 is absent or missing. This portion contains around 30 to 40 genes. Researchers have not yet identified all the genes and even aren’t aware of their full functionalities. The area of chromosome 22 that is missing in people with DiGeorge syndrome is called 22q11.2. A minor percentage of patients may experience a smaller deletion in the same section of chromosome 22.
The removal of genes in the specific region of chromosome 22 typically happens at random in the maternal egg or the paternal sperm. The deletion can also occur during very early stages of fetal development. Hence, the deletion tends to get repeated in ‘almost all’ or all of the cells in the body as the unborn baby grows.
Treatment of DiGeorge syndrome
DiGeorge syndrome has no known cure. Treatment is aimed at correcting the vital defects like cardiac problems and low levels of calcium. Medical care for mental health, developmental, or behavioral anomalies is more complex and the prognosis is usually less predictable.
Some of the treatment options for DiGeorge syndrome associated defects are listed below:
- Limited thymus function usually causes frequent but less serious infections like ear infections or colds. They are corrected as per standard treatment procedures.
- Severe dysfunction of the thymus gland or its absence can result in serious infections. Doctors may recommend transplantation of specialized bone marrow cells, or of thymus tissue, or of specific germ-fighting blood cells.
- A diet with decreased phosphorus and intake of vitamin D and calcium supplements can help manage hypoparathyroidism. In case sufficient parathyroid tissue is present, then the glands are more likely to eventually control the phosphorus and calcium levels in the body without a specific diet.
- Most types of cardiac defects related to DiGeorge syndrome need surgical intervention to repair and correct the blood circulation and heart abnormalities.
- Surgery is also required to correct a cleft palate and other problems of the palate
- The overall development of the child with DiGeorge syndrome can be enhanced with different therapies like occupational therapy for imparting daily skills, speech therapy for articulation and verbal skills, developmental therapy for behavior modification, and interpersonal and social skills learning. ADHD, depression, and other mental health disorders can be treated with medications and psychotherapy.
Life Expectancy
The prognosis turns better for individuals who are able to survive DiGeorge Syndrome during their childhood and early teens. With constant support, love and medical intervention, the person can live up to a normal life span.
DiGeorge Syndrome Pictures