America's Gluttony and Nutrition Fact Labels
IMPORTANT NOTICE: Before you read this article, keep in mind I am not a medical professional, I am self read. I do not give medical advice. I am not promoting any products. Some suggested litterature may somewhat promote either pharmacological products or nutritional products. I am not promoting them and chose the texts in questions because they explained, often, in the simplest manner, the mechanisms involved in the concerned metabolisms and pathologies. Some will be easier to grasp for the novice reader, others may prove challenging, but I support only one approach here, and that is in the quest to adressing the Metabolic syndrome and Diabetes Pandemic, and their associated multiple pathologies, the first course of intevention should be a change in diet. This change in diet is, I believe, an elimination of starchy foods from the diet of those who have pathologies of this nature, and a very tight control of starchy foods in the diet for those who do not show these signs yet. Promoting the elimination of starchy foods from diets is not a medical advice, and food is not a drug, I can therefore give advice on the diet without having to answer to the FDA or other authorities. Promotting some foods in a matter that associate them with medical benefits is a concern of the FDA. The human body does not need starchy foods to survive, It does not need grains or legumes or root vegetables.These foods offer the lowest nutrient density per calorie.
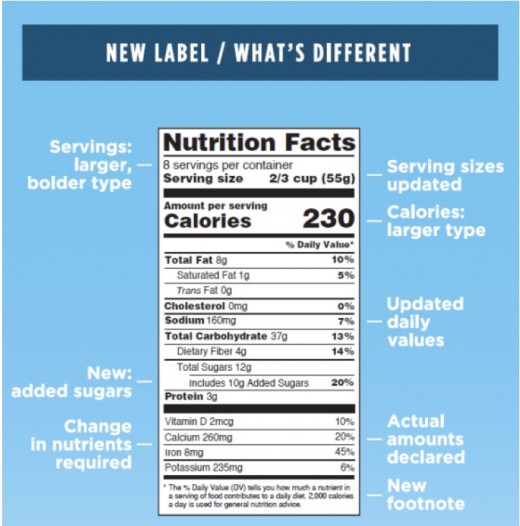
Nutrition Fact Labels still come short on Most Important Content
Last Spring, the FDA made public its proposition and format for the new Nutrition Fact Labels present on manufactured and transformed foods. Much accent has been put on the added sugars, since, as to the FDA, they represent the biggest danger to health. To the right is the proposition from the FDA material disseminated on May 20 2016.
It astonishes me that in the current catastrophic Obesity and Diabetes Type 2 demographics in the USA, the principal Substrate responsible for this heath catastrophe still can't find a place on our nutrition fact labels. On the other hand, my identification of the key substrate is in disagreement with that identified by the FDA.
Much litterature disagrees on the root cause of Obesity, Diabetes and the Metabolic Syndrome which have reached Pandemic proportions in the USA and Western World. Principal substrate proposed are Fats (some have theories as to specific fats), Fructose, Added Sugars (that also contain Fructose, but also Glucose). Very few, and more recent, litterature has pointed to the possibility that Digestible Starches, a Carbohydrate found in very high densities in Cereal grains, in Legumes and some Root Vegetables may be responsible1,2,3.
I am not a medical professional, nor a professional researcher, I am self-read. I have read extensively on the subject from peer reviewed litterature, and my opinion on this subject is that I also conclude that the principal substrate responsible for the health drift of Americans is Digestible Starches, and Starchy foods of our diets.
Furthermore, it appears that Fats are not the culprit of neither of the afformentioned conditions. Instead, Fats in the diet become a problem when juxtaposed to a High Glucose diet, which is what is procured by the high digestible starches content of the North American diet.4
Notice the Branched texture of Amylopectin. This structure gets broken down quicker and liberates its glucose into single units quicker than Amylose, giving an accelerated spike to plasma glucose (source: 2008 - Journal of Cereal Science)It appears that the FDA is under the impression that starches, digestible starches (Amylose and Amylopectins, which are respectively unbranched and branched Glucose polymers, Figure 1 at bottom of page) are safe for the health, and are therefore still not described explicitly on food labels, and must be calculated by differentiation and approximation.
Most doctors and nutritionists I have spoken to, either ignore that digestible starches are pure glucose, or, when deciphering a Nutrition Facts Label, believe that the "Total sugars" incorporate the count of glucose from starches. Now, this is inexact and as an FDA published document explains in:
"Food Labeling: Revision of the Nutrition and Supplement Facts Labels (dated march 3 2014)"
"...“Other carbohydrate” represents different types of carbohydrate, and, unlike sugars and dietary fiber, carbohydrates covered under this heterogeneous category have no shared physiological effects. Moreover, there is no well-established evidence to support the role of particular types of carbohydrate that fall within the “other carbohydrate” category, such as starch and oligosaccharides, in human health that is based on reliable and valid physiological or clinical endpoints. In addition, a quantitative intake recommendation for “Other carbohydrate” is not available from relevant consensus reports. Given the lack of public health significance or a quantitative intake recommendation for “other carbohydrate” as a category, consistent with the factors discussed in section I.C., we tentatively conclude that “Other carbohydrate” should no longer be permitted to be declared on the Nutrition Facts label."
It is astonishing that something as self evident as dietary glucose excess as cause, in the first hand of hyperglycemic bouts, that then gradually creates a progressive multi-organ health degeneration, metabolic disorganisation, can still be ignored by a whole discipline in their decision process. Yet, some litterature, which appears to have been ignored by the FDA is quite clear on this.
First: why self evident...when we test for Diabetes, we test with either Fasting Glucose (FG) or Oral Challenge Glucose Test (OCGT) postprandial glucose. The standard test used to be 50 or 75 gram equivalent of glucose from white bread, while the new standard is usually 75 grams glucose solution (which is much like a soft drink safe that any sucrose is changed for only glucose. Soft drinks were once made with sucrose (50% fructose - 50%glucose); from the 1990s and on, different mixtures of fructose-glucose ratios were used in a bracket of 40%-60% interchangeably. And the use of 55 High Fructose Corn Syrup, which is a mix of 55% Fructose and 45% Glucose, akin to honey, was agressively introduced.)
Now, the difference in response between white bread and glucose testing, in terms of metabolic response is important, yet once again ignored by scientific and political decision makers. Glucose solution drinks (single bound mono-saccharides form) creates a sudden but shorter lived metabolic plasma spike, while white bread, in fact the starchy component of white bread, because of the time needed to decompose the polymer structures slows the time to peak, and the time to trough. Important also, is that there is no food we eat that contains large amounts of unbounded glucose (free glucose), while we eat tremendous amounts of starchy foods (glucose polymers).5
In fact, it is estimated that close to 25% of the North American diet is composed of starchy foods against the 12% of dietary energy from added sugars.(see calculations below) Yet the whole health establishment focuses only on added sugars in terms of health focus, absolutely neglecting the greater ill that are starchy foods.
Calculations (approximative) for starch consumption by US adults: Now, the USDA is not making things easy when estimating this and it is incomplete because we only have numbers for refined grains (5,63 ounces), whole grains (0,83 ounces) and potatoes (0,37 cups). So,
- Refined grains is 5.63ounce*28gr*71%starch content*4 Kcal/gr = 447Kcal a day;
- Whole grains 0.83*28**63%*4 = 59Kcal a day;
- Potatoes 16*0.37*28*44%*4 = 291Kcal a day.
This is a total of 797Kcal a day of starches per US adult. This implies 200 grams of Glucose from starches a day. If we included all starchy foods (for exemple other starchy root vegetable and legumes), the number could be quite higher. Remember that this is an average, some may eat less, which means others eat more. For added sugar, the USDA (USDA website - NHANES 2007-2010 report) estimates that an adult consumes 17,5 teaspoons a day. Again,
- Added Sugars 17,5tsp*4grams/tsp*4 Kcal/gram = 280Kcal a day.
This can be approximated as being composed half glucose and half fructose. Therefore, Glucose from added sugars add up to approximatly about 35 grams of Glucose a day and 35 grams of Fructose a day. That is 235 grams of Glucose against 35 grams of Fructose from these 2 food sources alone. Obviously, both together add up to monstrous amounts of Glucose, yet the added sugars may be better metabolized because they are paired fructose-glucose mollecules. As you see, in this calculations, starches are way more than 25% of the estimated recommended 2000Kcal a day for an average adult. But people do overeat.
In England, it is estimated that an adult eats on average 110 to 135 grams of starches a day from all sources.6
Starchy foods need be the principal object of focus in the context that coupled sugars of differing type are better metabolized than single sugars.
One must be careful here and I will explain to avoid any confusion. When we ingest sugars, referred to as saccharides (more recently called glycans in the scientific litterature), they come in different structures.8 Their nomenclature is based on the number of attached unit they present. Saccharides bound between them from one of their Carbon atoms. Almost all sugars from our diets are hexose, meaning they are a six carbon structure. When one of these carbon is conjoined to another sugar, they share a common carbon atom at that site, this is the carbon bond of the saccharides chain. So, in our most common foods, they are very little free sugars, mostly glucose and fructose from fruits. Otherwise, most sugars are of di-, tri-, Oligo-, Poly-saccharides structures. This means you have 2, or 3, or more attached molecules between them forming a chain. Oligo-Saccharides are sugars that form chains of from 3 to 9 carbons bonds. And Poly-saccharides are chains of more than 10 carbons bonds. Sometimes, litterature will refer to both oligo and poly-saccharies simply as polysaccharides. The most common di-saccharides from our diets are Sucrose (Fructose-Glucose), Maltose (Glucose-Glucose) and Lactose (Galactose-Glucose).
The Nutrition Fact Labels subcategory Sugars from the Carbohydrate category do not include Digestible Starches but sugars with 3 carbon bonds and less (that is mono-, di-, tri-, and tetra-saccharides). The digestible starches were included in a general oligo- and poly-saccharides called other carbohydrates (but which excluded fibers which are undigestible starches and are specifically described). The "Other Carbohydrate" category won't be presented anymore on New Labels.
Now, back to metabolization. One must make the distinction between ingestion, digestion and metabolization. Ingestion is when the food enters the mouth and its pathway down the gut. From its ingestion a breakdown (digestion) of structure occurs mechanistically from chewing and biologically from saliva. As the food founds its way to the Gut and lower, it is progressively dcomposed into smaller units by gut enzymes. All sugar structures that we ingest and that are categorized as digestible are broken down to simple unbounded molecules9. Then they are ready to be metabolized by going through the lumen (Brush Broder membrane for Glucose). Other non-digestible sugars, such as fibers, find their way towards the colon where they ferment. Rarely, a sugar structure greater than a single molecule will be metabolized.
So, when scientists tested, in empty stomachs, how different sugar structures were metabolized, they tested free glucose, free fructose, free galactose, sucrose, lactose, maltose, etc...A recent study has made a meta analysis of past research on the subject. They observed that when more than one variety of sugar molecule is present in the diet, the sugars were metabolized quicker and at a greater rate.7 For example, 50 grams of sucrose, or 50 grams of glucose polymer were not metabolized identically. The sucrose or a fructose + glucose solution was metabolised at a rate of 40 to 65%, while the Glucose monomer was metabolized at between 30 to 40%. Which indicates that a heigthen level of plasma glucose will persist longer with a single kind of sugar in your diet than when you ingest structures that are paired or coupled of different mollecules. This is because the different sugars don't follow the same pathway. The fructose finds its way quickly to the liver where it is either used for energy or stored for fat, while the glucose travels through the blood and is directed, in preference towards organs that are insulin dependant for the glucose to metabolize, such as muscles.10
When the diet procures an excessive load of glucose in our diets, mostly through the ingestion of starchy foods, then, the insulin dependent organs are incompetent at handling the load, a state of hyperglycemia occurs. That is a state of heighten plasma and metabolic glucose. In this case, glucose must find new metabolic paths. It is actively redirected towards none insulin dependent tissue and organs where it will accumulate and eventually create inflammation by provoking a steril endocrine reaction. The excessive glucose concentrations are perceived by the endocrine system as a threat and inflammation is a line of defense aginst metabolic threats.11
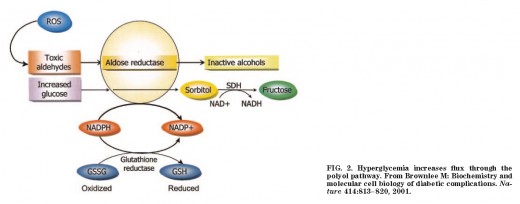
Un-metabolized excessive glucose from hyperglycemia also agonizes the polyol pathway11, which converts some of the excess glucose to fructose. Now, for many years, scientific medical research had identified fructose as the enemy substrate in our diets, but this is largely believed to be inexact now.
Polyol Pathway is activated during Hyperglycemia bouts but at yet an undetermined level in humans.The reason that fructose appears to have created liver damage, non-alcoholic-fatty-liver steatosis (condition encountered in most obesity and diebetes patient at differing degree of pathogenesis), is precisely, not because of the dietary fructose, but because of the excessive amounts of dietary glucose from starches that metabolically are converted, in part, to excess fructose, by the polyol pathway. Further, if glucose level are excessive, and the liver has met its energy needs, the fructose thus produced is converted to fat in the liver and accumulates in it. And in a context of impaired beta-oxidation of lipids, which hyperglycemia is now known to effect, these fatty deposits are never reconverted to fructose or glucose for energy, nore decomposed in free fatty acids or ketone bodies, they just accumulate.. As you know, it is accepted knowledge now, that hyperglycemia, especially chronic hyperglycemia, induces impaired beta-oxidation, and impaired ketolysis also.
Cahill (2006)12 gives a good overall view of the increasing understanding of Ketone Esters metabolism. In this review, the mechanisms and differences between Starvation and Glucose starvation, the place of Ketone Esters (refrred to as Ketone Bodies or Ketones which are AcetoAcetate, Acetone and Beta-hydroxydutyrate) metabolism are simply explained. It also concludes, and rightly so that Carbohydrates are not essential to the diet. Describes the Inuit diet made simply of meat and blubber (adipose tissue) which allowed this population to survive the harsh climate of the North for thousands of years. Cahill also explains that the human body needs about 100 gr. of Glucose a day, but all this glucose can be produced endogenously through the Glucose - Glycerol cycle, no need for eating carbs.
Ketone bodies are the product of triglyceride decomposition. They are another principal metabolic fuel, together with glucose and lipids (fatty acids). These 3 fuels form the Triumvirat of principal fuel substrates. Other subtrates are used marginally in certain tissues, for exemple Vitamin C (Absorbic acid). As a person accumulates hyperglycemic bouts, the body shifts progressively to give preference to glucose (no unique theory of these mechanisms appear to have imposed themselves up to now) as the unique fuel metabolite, and this is when pathologies start to occur. Our body need these 3 fuels for different processes, and when one fuel dominates over the 2 others, then metabolic balance is prevented. The most impotant contribution of Ketone bodies are their capacity to rebalance the mitochondrial redox (reduction-oxidation) complex, where metabolic stress translates in the accumulation of overexpresion of free radicals such as SuperOxide and Peroxynitrite. Beta-Hydroxybutyrate has been demonstrated to specifically neutralize inflammasome NLRP3.13,14,15,16,17
So, our diets contain very few uncoupled fructose mono-saccharides or polymers (this surprises again most health practitioners who mostly believe that most fruits are pure fructose, while in fact most contain some sucrose, some fructose and some glucose to different proportions. Very few have high fructose concentrations. Among fruit commonly part of the North American diet, pears appear to have the greatest fructose to glucose ratio, and is about 3,5:1. While the majority of fruits have a ratio of about 1.25:1 to 1.5:1, and a few have ratios under 1. And so by far Glucose occupies the greates density on the North American diet.
Galactose in our diet mostly always comes coupled (most common form being galactose-glucose referred to as lactose). It is the sugar of dairy products.
Information for these "sugar content" comes from an FDA publication that are used as reference for food labels: Sugar Content of Selected Foods: Individual and Total sugars (USDA, Human Nutrition Information Service, Home Economics Research Report 48, September 1987, R.H. Matthews, Pamela L. Pehrsson and Mojgan Farhat-Sabet.). Note here that sugars (on the Nutrition Facts Label) excludes digestible starches, again, which is incredible, because the whole USDA excludes digestible starches from their descriptive calculations of sugars, yet it is composed of glucose, a saccharides. Why include digestible mono-, di-, tr-, tetra- saccharides while excluding digestible starches is incomprehensible.
The reason is certainly political. The metabolic syndrome, and associated pathologies such as Type 2 Diabetes Mellitus (T2DM) costs the American health system an estimated $250 Billion annually, yet the most important contributor source to the Syndrome from the North American diet, GLUCOSE from starches, is ignored.
Only dietary glucose, in our diet, comes in very high density. Yet, these glucose polymers from digestible starches are to ones we cannot find explicitly on nutrition fact labels.
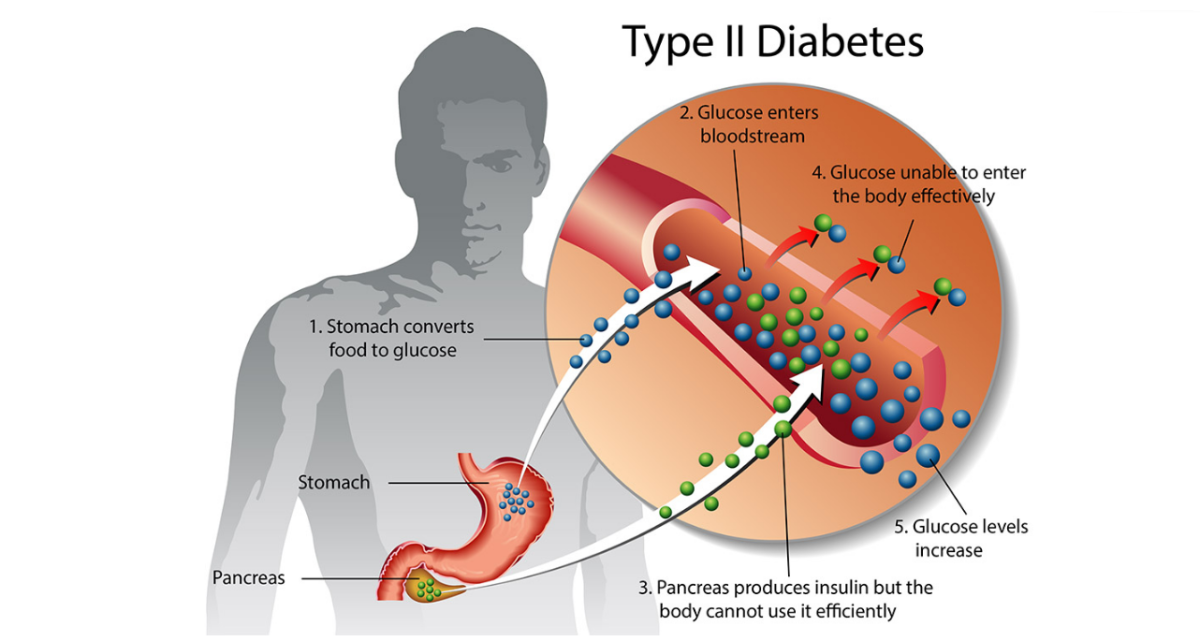
To understand the Metabolic Syndrome, Obesity and (T2DM), one effectively has to understand T2DM differently. For decades now, Diabetic "Complications", cardiovascular diseases and neuropathies being the principal, were conditions believed to originate from the diabetic state. This implies that there must be somewhat of a causetive relationship between the complication pathologies and diabetes, from the metabolic changes provoked by T2DM in the appearance of these "complications".
But this may be a errounous understanding of the biology of Diabetes. Yet, it is true, that under the etiology of Diabetes, a progressive degeneration of the self regenerating rate of beta cells from the Pancreas, insulin secretion becomes impaired. With insufficient insulin secretion, glucose is progressivly not metabolized and provokes hyperglycemic bouts. Yet, diet alone, with heavy starch loading, creates such metabolic demand that insulin production is insufficient. It is these bouts of hyperglycemia, when repeated over and over, often on a daily basis that will eventually damage the pancreas endocrine tissues lodging the endocrine beta cells. But yet, one may not need to ever develop diabetes or have beta cell insufficency to suffer metabolic damage from hyperglycemia. Elevated glucose levels, independant of insulin secretion, creates damage to most sites of the human body. The litterature is deep in knowledge with this. This is why diabetes is referred to as as multi-metabolic dysfonctional state. 18,19,20, 21, 22,23,24,25,26
Yet, it has progressively become clear that the "complications" can be diagnosed in the pre-diabetic phase and even in the absence of any diabetic etiology. And less evident, is that what often appear to be idiopathic conditions of cardiovascular or neuropathic origin can also be associated with another unifying factor, and this is hyperglycemia bouts.
This means if one ceases to view cardiovascular diseases and neuropathies as complications of diabetes (which implies as a consequence of), but rather the consequence of chronic hyperglycemia bouts, than one can understand T2DM as also a consequence of hyperglycemia bouts. And at the origin of hyperglycemia bouts are dietary starches. This would be a novel and useful way to understand the Metabolic Syndrome and T2DM and would have interested parties focus a lot more on lifestyle modifications first instead of pharmacological intervention therapies when the disease, and hyperglycemia events, have often aleady created irreparable damages.
It is primordial here that hyperglycemic bout should not be understood in a bureaucratic manner as by consensus thresholds as established by the World Health Organization, or the different Diabetes Association across the western world. These criteria were not meant to set exclusionary standards of treatment or considerations. But rather increase awarness of the caracteristics of the disease and perceived by biological markers. Yet, most clinical research tests in animals offer supradosages for analysis, but the opposite for humans where does of 50 and 75 grams of carbohydrate are the standards, even when the North American diet, for some people, often can contain 300 to 400 grams of carbohydrates in a meal.
In this view, not being restricted by the protocol, may allow quick modification of lifestyle choices.
This is a small exemple I prepared in my communications with the FDA to demonstrate the necessity to include total digestible starches on the Nutrition Fact Label. A fast food meal: A Big MAC, a Large Fry (without ketchup) and a Large regular Coke; Just looking at the Total Carbohydrate category of the Nutrition Fact Label (actual versus suggeted change in 2018) :
Before (now until 2018) :
- Total Carbohydrate 192 grams
- Total Fibers 7 grams
- Total Sugars 77 grams
New Label (2018) :
- Total Carbohydrate 192 grams
- Total Fibers 7 grams
- Total Sugars 77 Grams
- Added Sugars 77 grams
Now one would think then that taking a Diet Coke would solve the health problem concerning sugars..bringing total and added sugars to 3 grams. But this is inexact...because food labels don't explicitly describe digestible starches. Therefore, if, as I have proposed, Digestible starches are explicitly described on the label, you would get something like this :
- Total Carbohydrate : 192 Grams
- Total Digestible starches (glucose) 108 grams
- Total Fibers 7 grams
- Total Sugars 77 grams
- (the FDA could add added sugars if they pleased)
The consumer can now see clearly his total consumption of monosaccharides the total glucose, added to the sugars, he consumes in this meal approximatly 146,5 gr of glucose and 38,5 gr of fructose. " But he could simply read it as 185 grams of monosaccharides or 108 grams of glucose and 77 grams of added sugars. Incontestably, he is better informed...Would you like an apple struddel with your order....". The argument of the FDA that starches are not considered, according to them, a threat to health, that there is no need to put them on the label, is ignoring there on logic. They put salt because if you put too much it may be dangerous, yet this agurment is progressively loosing steam in the scientific community. They put cholesterol because they believe that too much cholesterol in the diet is harmful. Yet we need cholesterol, women to produce Estradiol (estrogen) and men to produce Testosterone. Also, we can synthetise cholesterol in our body, therefore we don't need to eat it. Yet, if our metabolisms are not impaired, we can eat too much of it and excrete the excess.
The problem with cholesterol, as with other fats, its that their metabolization is impaired by the High Glucose diet. If cholesterol increases in the blood as a marker, it is because its use is impaired by too much glucose. This is why Low testosterone is a strong predictor of Diabetes in men, and High testosterone is a strong predictor of Diabetes in women (in women Estradiol metabolism is dysregulated by impaired cholesterol metabolizatiion which leads to higher levels of testosterone).
Since nutritionists always explain, as does the FDA, that the only problem with starches is when you eat excessive amounts, then their reasonning is that there is no reason to put them on the labels, then why put salt or cholesterol or anything else for that matter. Digestible Starches is the nutrient that has increased the most in caloric value and as a percentage of our diets in the past 20 years.
It is again mind boggling, to an outsider, a low information participant to this debate, that almost no research has been done to identify thresholds of hyperglycemia in humans where metabolic damage occurs, where metabolic mechanism are switched to pathological ones (polyol pathway for example). I have found one single animal research were a threshold of 180 mg/dL plasma glucose for 60 minutes activates the polyol pathway in rabbits.
Most animal models otherwise use supradosage to obtain clear readings of certain processes. Yet an increasing amount of litterature does observe the damage of high concentrations of glucose in all major organs, including the brain (brain atrophy for exemple31), the clear signaling center to our metabolism through hypothalamic functions, glucose sensing neurons, and from the limbic system.
What metabolic damage occurs with the accumulation of glucose, fructose, myo-inositol, and other sugars, "en masse" in certain tissues and organs, which don't necessitate insulin for glucose metabolization? For example, nerve system tissues can metabolizes glucose, at a slow rate though, without insulin. But a large accumulation of glucose and other sugars creates an endocrine defense reflex, either steril or RAMP. responsible for triggering inflammasome NLRP3. This is the principal Inflammasome of the Diabetic etiology. An Inflammasome is a complex that releases substrates that are a first line of defense to protect the integrity of our body. Subtrates such as Interlukins and Necrotic Nuclear Factors. Inflammation sets in the tissue, often locking fluids in certain compartments, preventing proper osmolality, and unbalancing ionic metabolite (sodium, potassium, and even metals such as zinc). 27, 28
On the short term horizon, inflammation is a beneficial reaction, but when it persists, it is the opposite, it weakens the metabolism, making it even more vulnerable to diseases.
Remember, that which often is forgotten by the scientific community, that glucose is a polarized substrates, and this is why, among other ills, hyperglycemia is responsible for osmollality dis-regulation. Glucose doen't transport itself within the human body but is assited by 2 classes of Transporter, the non sodium dependent diffusin Transporters (GLUT family..GLUT1 to GLUT8 have now been identified) and at least 2 Sodium-Glucose Co-Transporters (SGLT1 nd SGLT2). As glucose loads increase in the Stomach, SGLT1 and SGLT 2 are geneticly expressed at a greater rate to meet Glucose supply. SGLTs are small molecules which mobilize 2 sodium molecules. When transported in this fashion, SGLTs by their sodium mobilization, effect changes in sodium gradient and in electric potential. This in turn modifies osmolallities locally as SGLT also displace water in their structure : "While these experiments clearly demonstrated that there is a close relationship between Na+/glucose cotransport and the initial rate of water transport, controversy remains as to the interpretation of the results. We have favored the water cotransport hypothesis, while others favor a strict osmotic coupling, i.e., water flowed in response to the osmotic gradients set up by Na+/sugar cotransport into the cell."29 and when Glucose is in excessive quantities, disregultates the capacity of the Hypothalamus to properly manage basoreceptor signaling, dysregulating water metabolism, from a multitude of mechanism, of which Arginin Vasopressin Secretion (Anti-Diuretic Hormone) is principal.30
Diabetes and Obesity are both Chronic Inflammed Conditions. Tissues suffering inflammation in diabetes, among others : adipose tissue, muscle tissue, cardiovascular tissue, nervous system tissue, epithelial lumen tissue, etc...it should be clear by now...if one single metabolite must be identified as central in the context of diet induced diseases in general, but particularly in the context of the Metabolic Syndrome, Obesity and Type 2 Diabetes Mellitus...IT IS GLUCOSE..
My FDA Food Labeling proposition is therefore:
in the category carbohydrates:
Total Carbohydrates......................................x gr.
Total digestible starches.................x gr.
Total Fiber.......................................x gr.
Total Sugars (excluding starches)....x gr.
-(They could add "Added sugars" if the want as a subcategory)
This should guarantee better and adequate information yet must be accompanied by proper nutritional education from the health community. Then and only then, will the public be truly well equipped to better their health situation and provoke a quick and massive drop in the upper mentioned conditions tied to bad nutritional habits.
References:
1. High Carbohydrate intake from starchy foods is positively associated with Metabolic disorders: A Cohort study from a Chinese Population (Rennan Feng et al.) 2015 - Nature
2. Refined Grain comsumption and the Metabolic Syndrome in Urban Indians (Ganesan Radhika et al.) 2009 - Metabolism, Clinical and Experimental
3. Carbohydrate intake and Refined grain Consumption are associated with the Metabolic Syndrome in Adult South Korean Population (MS SuJin Song et al.) 2013 - Journal of the Academic of Nutrition and Dietetics
4. Fat: The new health paradigm (Stefano Natella, Vamil Divan and Marcella Geraldo) 2013 - Research Institute, Credit Suisse Research. (Please take note here that this is produced by an investment house as an economic perspective on new scientific insights that could strongly modify some sectors of the economy). It does not directly sell any investment products or services, it is meant for Investment decision Makers. It is well written, with excellent references, and very accessible in terms of content. I am not associated in any way with Credit Suisse orrganization).
5. Acunte Metabolic Response to High carbohydrate, High starch meals compared with Moderate Carbohydrate, Low starch meals in Type 2 Diabetic Patients, (MC Gannon, S Fang, FQ Nuttal, N Ercan-Fang, SA Westphal) 1991 - Diabetes care 21: pp. 1619-1626
6. Carbohydrates and Health, 2015, Scientific Advisory Committee on Nutrition, England
7. Fructose Metabolism in humans - What Isotropic Tracer studies tell us. (Sam Z Sun and Mark W Empie) 2012 - Nutrition and Metabolism 9:89
8. Essentials of Glycobiology 2nd Edition - Editors: Ajit Varki, Richard D Cummings, Jeffrey D Esko, Hudson H Freeze, Pamela Stanley, Carolyn R Bertozzi, Gerald W Hart, and Marilynn E Etzler -2009, The Consortium of Glycobiology Editors, La Jolla, California (available online as Open Access at: https://www.ncbi.nlm.nih.gov/books/NBK1908/?report=printable) Excellent, it covers all aspects of carbohydrates.
9. Hypoglycemia as a pathological result in Medical Praxis (G. Bjelakovic et al.) 2011 - Chapter from the book available online: Type 1 Diabetic Complications ( http://www.intechopen.com/books/type-1-diabetes-complications) Edited by Professor David Wagner
10. Normal Glucose Homeostatis (MZ Shrayyef and JE Gerich) 2010- Principles of Diabetes Mellitus L. Poretsky Ed. - Chapter 2
11. The pathobiology of Diabetic Complications : A Unifying Mechanism (Micheal Brownlee) 2005 - Diabetes
12. Fuel Metabolism in Starvation ( George F. Cahill) 2006 - Annual Review of Nutrition 26:1-22
13.The Determination of the Redox States and Phosphorylation Potentialin Living Tissues and Their Relationship to Metabolic Control of Disease Phenotypes (Richard L. Veech) 2006 - Biochemistry and Molecular Biology Education Vol 34 No 3 pp 169-179
14.Ketone body β-hydroxybutyrate blocks the NLRP3 inflammasome-mediated inflammatory disease (Yun-Hee Youm, Kim Y. Nguyen et al.) 2015 - Nature Medicine. 2015 March ; 21(3): 263–269. doi:10.1038/nm.3804.
15. Nutritional, Dietary and Postprandial Oxidative Stress (Helmut Sies, Wilhelm Stahl, and Alex Sevanian) 2005 - American Society for Nutrition Sciences
16.Type 2 diabetes mellitus and inflammation: Prospects for biomarkers of risk and nutritional intervention (Badawi et al.) 2010- Dovepress
17. Diabetic cardiac autonomic neuropathy, inflammation and cardiovascular disease (Aaron I Vinik, Tomris Erbas, Carolina M Casellini) 2013 - The Journal of Diabetes Investigation Volume 4 Issue 1
18. Hyperglycemia in Critical Illness: A Review (David Brealey and Mervyn Singer) 2009 - Journal of Diabetes Science and Technolog Volume 3, Issue 6
19. Ketogenesis prevents diet-induced fatty liver injury and hyperglycemia (David G. Cotter and Baris Ercal) 2014 - The Journal of Clinical Investigation
20. Pathogenesis of Chronic Hyperglycemia: From Reductive Stress to Oxidative Stress (Liang-Jun Yan) 2014 - Journal of Diabetes Research
21. Contribution of polyol pathway to arteriolar dysfunction in hyperglycemia. Role of oxidative stress, reduced NO, and enhanced PGH2/TXA2 mediation (Akos Keller et al.) 2007 - American Journal of Physiology - Heart and Circirculatory Physiology
22. Hyperglycemia Activates Caspase-1 and TXNIP-Mediated IL-1b Transcription in Human Adipose Tissue (Tim B. Koenen, Rinke Stienstra et al.) 2011 - Diabetes
23. Association of ketone body levels with hyperglycemia and type 2 diabetes in 9,398 Finnish men (Yuvaraj Mahendran) 2013 - Diabetes
24. Modulation of gastrointestinal vagal neurocircuits by hyperglycemia (Kirsteen M. Browning) 2013 - Frontiers in Neuroscience
25. Dietary Hyperglycemia, Glycemic Index and Metabolic Retinal Diseases (Chung-Jung Chiu and Allen Taylor) 2013 - Progress in Retinal and Eye Research
26. 50 years forward : Mechanisms of Hyperglycemia driven diabetic complications (Nicholas D. F. Russell and Mark E. Cooper) 2015 - Diabetologia
27. Upregulated NLRP3 Inflammasome Activation in Patients With Type 2 Diabetes (Hye-Mi Lee, Jwa-Jin Kim, Hyun Jin Kim, Minho Shong, Bon Jeong Ku and Eun-Kyeong Jo) 2013 - Diabetes Vol 62
28. Sterile inflammation: sensing and reacting to damage (Grace Y. Chen* and Gabriel Nuñez) 2010- Nature Reviews of Immunology
29. Biology of Human Sodium Glucose Transporters (Ernest M. Wright,, Donald D.F. Loo, and Bruce A. Hirayama) 2011 - Physiological Review 91: 733–794
30. Sugar for the brain: the role of glucose in physiological and pathological brain function (Philipp Mergenthaler et al.) 2013 - Trends in Neuroscience
31. Brain Atrophy in Type 2 Diabetes (Chris Moran, Gerald Munch et al.) 2013 - Diabetes Care 36:4036–4042
Figure 1. - Digestible Starch Structure
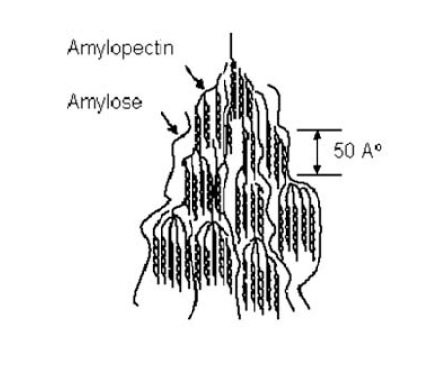
Figure 2 - The Polyol Pathway