Abnormal Psychology: Clinical Perspectives on Psychological Disorders Chapter 12 Notes
Chapter 12: Substance-Related and Addictive Disorders
- Case Study: Carl Wadsworth
- Demographic information: Carl is a 32-year-old African American male.
- Presenting problem: Carl's sister Janice made an appointment for him to see a therapist at a local outpatient therapy clinic following an arrest for public intoxication. Janice stated that the family was “sick of being worried” about him. She reported that Carl had been drinking much more frequently over the past few years than ever before, culminating in his recent arrest for public intoxication. Janice also reported that Carl has bipolar disorder, although he is not on medication currently, about which she and the family were concerned. During the intake session, the therapist noticed that Carl appeared intoxicated. She decided not to confront him about this during the appointment. When he presented for the next appointment intoxicated again, the therapist asked him directly if he had been drinking prior to the session, as she was concerned that his alcohol usage would interfere with therapy. Carl's reply was, “Maybe … just a little.” The therapist asked Carl to refrain from drinking before their next appointment, to which he agreed. When he showed up to the third appointment intoxicated yet again, the therapist decided that she needed to address his alcohol use before he could make any progress in therapy. Carl had expressed that he was ashamed of his alcohol use, but that he found himself unable to cut down on his drinking. He described symptoms of withdrawal such as shaking and feeling nauseous if he did not have a drink within the first few hours of waking up in the morning. Carl stated that he had been working in a liquor store for the past 4 years, and it was difficult for him to refrain from drinking when he could so easily access alcohol. He agreed with the therapist that it would be important to address his issues with alcohol before beginning psychotherapy. Janice called the therapist the following week to tell her that Carl had been in a car accident and was arrested for driving while under the influence of alcohol. Carl had driven into a lamppost near her home and reportedly had a blood alcohol level over three times the legal limit at the time of the accident. Janice reported that Carl sustained only a minor concussion and a few scratches. While he was in the hospital for observation, he told Janice that he was ready to quit drinking for good and wanted to go to therapy. Janice explained that Carl had lost his job after his first arrest for public intoxication, and he and the family were “willing to try anything” to help him quit drinking. The therapist agreed to see Carl, and he attended the following session sober. Carl told his therapist about his experiences with bipolar disorder and with lithium, a medication that clinicians typically prescribe to treat the disorder. Carl described that he preferred drinking to taking medication because he did not experience side effects, and he found weekly blood testing while on lithium “annoying.” Carl stated that he had never really drunk much alcohol, as his parents are both former alcoholics and he worried that he might be susceptible to alcoholism. His drinking began 4 years prior when he began working at a liquor store. At the time, he was stable on medication and had not experienced any significant psychological impairment for several years. “I wasn't planning on drinking at work ever, but my boss sure liked to, so we started getting drunk together after closing up for the night,” Carl reported. Since he found it difficult to drink heavily while on lithium, he decided to stop taking his medication so that he could drink with his boss, who would taunt Carl to drink if he declined his offer. Since Carl was drinking mostly at night and was living by himself, no one in Carl's family had noticed that he was drinking. After a few months of drinking every day at work, Carl reported that he started to experience withdrawal symptoms when he woke up in the morning, and so he began drinking immediately when he woke up and while he was at work. He continued with this routine for the next 2 years. Although he was working during this time, he was essentially unable to perform any activities outside of work. His family grew increasingly worried, especially when he repeatedly showed up intoxicated at his parents' house. They urged him to try AA and warned him of the dangers of his drinking, although Carl denied that he was having any problems. To show his family that he did not have a problem, Carl would stop drinking for 1 or 2 weeks, although his desire to drink was too intense to allow him to go any longer than that. Carl grew increasingly depressed as he went without medication, and his drinking grew more severe; however, instead of seeking treatment, Carl only drank more when he was feeling particularly depressed. While at work one day, Carl was arrested for public intoxication for verbally haranguing a customer. Occasionally he would get into an argument at work, although his boss typically did not take much notice. However, during this particular incident he threatened violence against a customer, and Carl's boss had no choice but to fire him and report him to the police. The police held Carl overnight and released him the next day, as the customer chose not to press charges. Without an income, Carl was forced to move out of his apartment and move in with Janice, who luckily for Carl lived nearby. Worried that Carl had spun out of control and unsure how she could help him, Janice called the clinic for an appointment. “She had me on lockdown,” Carl stated about living with his sister during this time. After Carl showed up for therapy intoxicated, Janice removed all alcohol from her home and forbade Carl to leave the house unaccompanied. At first, Carl struggled with severe withdrawal symptoms, “and then all of a sudden,” he said, “I felt great. I felt invincible, actually. It was then that I knew that I was becoming manic.” He described pacing around the house and an inability to sleep for 3 days due to racing thoughts and an abundance of energy. After convincing Janice that he needed to borrow her car to go to the grocery store, Carl drove to a nearby liquor store, purchased a bottle of whiskey, and drank the entire bottle within a matter of minutes. On his way back to Janice's home, he drove into a lamppost and was subsequently arrested.
- Relevant history: Carl reported that clinicians diagnosed him with bipolar disorder when he was 18 years old, following a manic episode in which he had slept for about 4 hours over a period of 6 days. “I was living on my own, so no one noticed what was going on,” he stated. He eventually checked himself into the hospital, convinced that he was having a heart attack. He entered the hospital psychiatric unit for 1 week and began taking lithium. Over the next 10 years, Carl occasionally struggled with some mood symptoms such as depression or racing thoughts, although these symptoms did not significantly interfere with his life. Of note, however, is the fact that Carl has had limited interpersonal and adult romantic relationships. “I'm too messed up to have any friends, so I just like to keep to myself,” he explained. When Carl was 28, the telecom company for which he worked downsized and he lost his job. Carl became so depressed that he attempted suicide at his parents' home, where his mother discovered him. He re-entered the hospital for about 1 month and began receiving disability, which allowed him to receive medication and therapy. While relaying his history, Carl noted that he rarely drank alcohol during this time, due mainly to the medication he took, but also because his parents were both former alcoholics and he reported feeling worried that he would follow the same path should he start drinking. His heavy drinking only began after starting the job at the liquor store. Because Carl made enough money at the job to afford his own apartment, he felt hesitant to let his boss down by refusing to drink with him.
- Case formulation: An important distinction to make in Carl's case is whether his alcohol use occurred secondarily, as a result of his bipolar disorder, or whether it arose independently, which would qualify for a dual diagnosis. As Carl stated regarding the episode of drinking that occurred while at his sister's, he began drinking heavily while he was manic, believing that he could handle drinking a large quantity of alcohol and still be able to drive safely. However, this was the only instance in which he reported drinking while experiencing mood symptoms. After careful consideration of his case, it appears that Carl's initial problems with alcohol began in the absence of mood symptoms. Additionally, his alcohol consumption did not appear to cause his mood symptoms. Because of these two distinctions, Carl qualifies for a dual diagnosis of Alcohol Use Disorder, Severe, and Bipolar Disorder. Furthermore, Carl meets the criteria for Bipolar I Disorder due to the presence of manic, rather than hypomanic, episodes, which required hospitalization and severely impacted his functioning.
- Treatment plan: Carl agreed to attend a local Alcoholics Anonymous (AA) meeting on a daily basis in conjunction with weekly psychotherapy. Carl also agreed to see a psychiatrist for a medication evaluation.
- 12.1: Key Features of Substance Disorders
- A substance is a chemical that alters a person's mood or behavior when the person smokes, injects, drinks, inhales, snorts, or swallows it in pill form. Substance-related disorders reflect patterns of use (and abuse), intoxication, and withdrawal.
- DSM-5 combines abuse and dependence into a single dimensional rating. Individuals receive a diagnosis based on meeting only two criteria, but they are rated according to the degree of severity of their symptoms.
- A person in a state of substance withdrawal shows physiological and psychological changes that vary according to the actual substance involved.
- Tolerance occurs when an individual requires increasingly greater amounts of the substance in order to achieve its desired effects or when the person feels less of an effect after using the same amount of the substance.
- A substance use disorderis a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues using a substance even though it causes significant problems in his or her life. Clinicians diagnose substance use disorders by assessing the individual in four categories of symptoms: impaired control, social impairment, risky use, and pharmacological changes. They then count the number of symptoms the individual demonstrates and use this number to assign a severity rating of from mild to severe.
- Although many people commonly refer to these disorders as representing an “addiction,” the DSM-5 authors prefer the more neutral term of “substance use disorder.” They believe that substance use disorder, specifying mild to moderate, is more precise and has fewer negative connotations than the term “addiction.” Similarly, people with these disorders are not referred to as “addicts,” but instead as individuals with substance use disorders.
- People with substance use disorders suffer a range of significant effects on their daily life. Often they neglect obligations at work, and their commitments to home and family start to erode. In addition to letting their work and family life slide, they may begin to take risks that are personally dangerous and put others in jeopardy, such as driving or operating machinery while intoxicated. Legal problems can arise for people who abuse substances. In addition to arrests for driving while intoxicated, they may face charges of disorderly conduct or assaultive behavior. These disorders also frequently involve interpersonal problems due to the fact that abuse and dependence on drugs create strains on relationships with family, friends, and co-workers. In extreme cases, these disorders can also lead to health problems and even premature death.
- People receive a diagnosis of substance intoxicationwhen they experience a drug's effects on their physiological functioning and show signs of significant impairment. The extent of substance intoxication that an individual may experience depends on the specific drug, how rapidly it acts, and the duration of its effects. Efficient absorption of intravenous or smokable drugs into the bloodstream is likely to lead to a more intense kind of intoxication than are drugs taken in pill form.
- Substance intoxication- The temporary maladaptive experience of behavioral or psychological changes that are due to the accumulation of a substance in the body.
- The second category of substance-induced disorders includes those that reflect the effects of withdrawal in which individuals develop behavioral changes that are specific to the particular substance. These changes include physiological and cognitive alterations that are associated with the discontinuation of the particular substance in question. Other disorders can also be associated with substance use including psychotic disorder, mood disorder, anxiety disorder, sexual dysfunction, and sleep disorder. People may also show comorbidity of the substance-related disorder with another condition, such as an anxiety disorder or a mood disorder.
- 12.2: Disorders Associated with Specific Substances
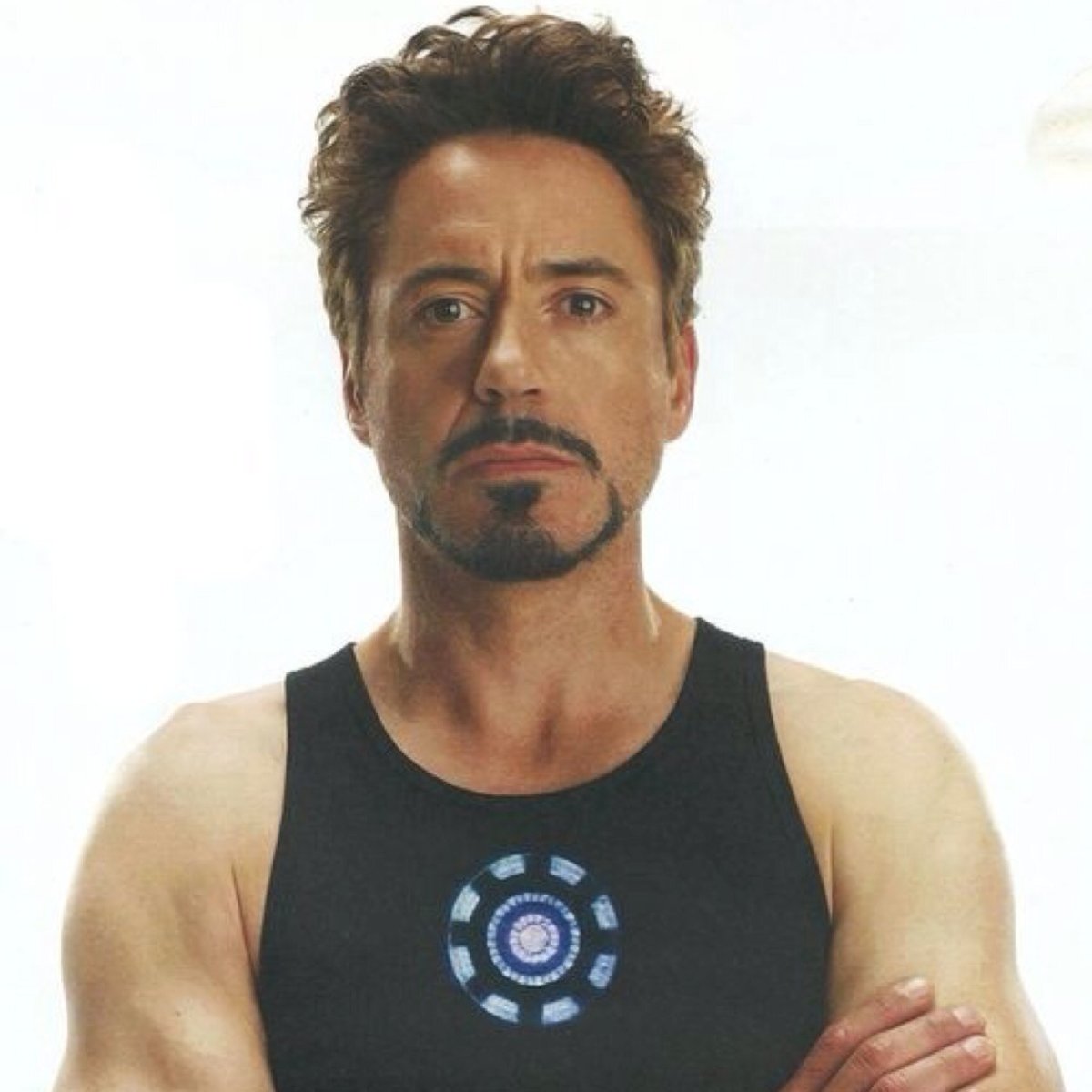
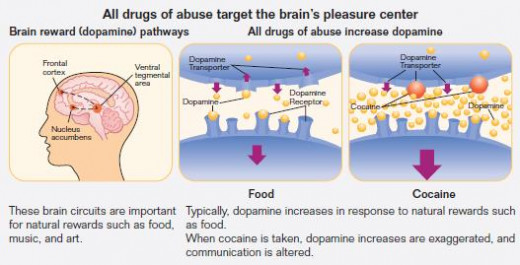
- Most drugs of abuse directly or indirectly target the reward center of the brain by flooding its circuits with dopamine.
- Overstimulation of the reward system produces the euphoric effects that abusers seek and leads them to repeat the behavior in order to repeat the experience. Drugs are more addictive than natural “highs” produced by such activities as eating and sex because they release far more dopamine (2 to 10 times as much) than do natural rewards, and the effects last much longer. Over time, the neurons in these dopamine pathways “down-regulate” in response to these surges in dopamine, meaning that they produce less dopamine themselves or reduce the number of dopamine receptors. Users then need to take drugs to raise their dopamine levels back up to normal. In order to experience the effects they experienced initially from the drugs, they also need to take higher and higher levels; in other words, they develop tolerance.
- Because users learn to associate the pleasurable feelings of using the drug with the cues in the environment that were there when they took the drug, they develop classically conditioned responses that maintain their addiction. In addition to involving dopamine, some drugs of abuse involve glutamate, a neurotransmitter involved in memory and learning. Consequently, long-term drug abuse can lower the individual's level of glutamate and therefore lead the individual to experience impairments in memory.
- The three possibilities for this comorbidity are (1) drugs of abuse lead users to experience symptoms, such as psychosis in marijuana users; (2) psychological disorders can lead to drug abuse as individuals attempt to self-medicate; (3) similar factors, such as genetic predisposition, early exposure to stress and trauma, or structural brain abnormalities, cause both drug abuse and psychological disorders (National Institute on Drug Abuse, 2010).
- Drug use typically begins in adolescence, which is also the time of heightened vulnerability to other psychological disorders. Early drug use is also a risk factor for later substance use disorder and may also be a risk factor for the subsequent development of other disorders. The risks are particularly likely to occur in individuals who have high genetic vulnerability. In one study following adolescents into early adulthood, only the heavy marijuana users with a particular gene variant had significantly higher risk of developing schizophreniform disorder (Caspi et al., 2005).
- Higher rates of substance use disorders also occur in physically or emotionally traumatized individuals. This is a matter of particular concern for the veterans returning from the Iraq and Afghanistan Wars. As many as half of veterans who have a diagnosis of PTSD, also have a comorbid substance use disorder. In addition, researchers estimate that 45 percent of offenders in state and local prisons have a comorbid mental health and substance use disorder. People with a comorbid substance disorder and either PTSD or a criminal history may have difficulty receiving treatment. Veterans with PTSD and substance disorders may not receive treatment for the PTSD until the substance use disorder is treated; however, traditional substance disorder clinics may defer treating the PTSD. Incarcerated criminals may also have difficulty receiving appropriate treatment in the prison system. Consequently, individuals with comorbid disorders face particular challenges in treating their substance use disorders (National Institute on Drug Abuse, 2010).
- Alcohol
- Alcohol use is associated with several categories of disorders including use disorders, intoxication, and withdrawal. Statistics based on the United States show that alcohol is a commonly used substance. More than half (51.8 percent) of Americans over age 12 reported that they had had at least one drink in the month prior to being surveyed. Nearly one-quarter (23.1 percent) of Americans 12 and older reported that they engaged in binge drinking, meaning that they had had five drinks on one occasion in the past 30 days. Heavy drinking, defined as consuming five or more drinks on the same occasion on at least 5 days in the month, was found in 6.7 percent of Americans 12 and older. Variables associated with higher rates of alcohol consumption were as follows: being male, white, married, a smoker, employed, and having a higher educational level and a higher income (Moore et al., 2005).
- Patterns of alcohol use are also associated with age (Figure 12.4). Young adults ages 18 to 25 have the highest rates of binge drinking and heavy drinking. Of that group, adults ages 21 to 25 have the highest rates of drinking, with 45.5 percent engaging in binge drinking. The rates of binge and heavy drinking decline sharply throughout adulthood; among people 65 and older, 7.6 percent engage in binge drinking and 1.6 percent in heavy drinking.
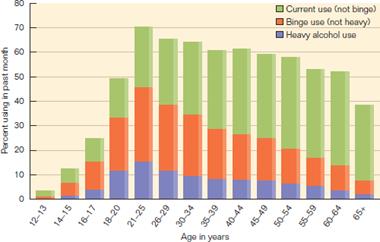
- The decline in binge and heavy drinking are part of a larger picture of “maturing out,” similar to the maturation hypothesis of age and personality disorders. However, the pattern of age-related changes in drinking patterns is not that clear-cut. Longitudinal studies show that, although people are less likely to start drinking after the young adult years, many people continue to persist in their previously established patterns of alcohol use disorder throughout adulthood. Certain life transitions are associated, however, with decreases in alcohol use. For men, parenthood is associated with lower rates of alcohol use after the age of 38; women show the opposite pattern. Men who lose their jobs have the highest rates of alcohol use after age 38; for women, there are no relationships between job status and alcohol-use persistence. These findings suggest that the relationships among alcohol use, life transitions, and gender are complex so that maturation alone is not sufficient for understanding age-related changes in alcohol use disorders. (Vergés et al., 2011).
- Mini case
- Rhona is a 55-year-old homemaker married to a successful builder. Every afternoon, she makes herself the first in a series of daiquiris. On many evenings, she passes out on the couch by the time her husband arrives home from work. Rhona lost her driver's license a year ago after being arrested three times on charges of driving while intoxicated. Although Rhona's family has urged her to obtain treatment for her disorder, she denies that she has a problem because she can “control” her drinking. The mother of three grown children, Rhona began to drink around age 45, when her youngest child left for college. Prior to this time, Rhona kept herself extremely busy through her children's extracurricular activities. When she found herself alone every afternoon, she took solace in having an early cocktail. Over a period of several years, the cocktail developed into a series of five or six strong drinks. Rhona's oldest daughter has begun lately to insist that something be done for her mother. She does not want to see Rhona develop the fatal alcohol-related illness that caused the premature death of her grandmother.
- Clinicians classify alcohol as a nervous system depressant. Its effects vary by the amount that the drinker ingests. In small amounts, alcohol has sedating effects, leading users to feel relaxed. As people ingest more alcohol, they may begin to feel more outgoing, self-confident, and uninhibited. As people drink beyond that point, the depressant effects become apparent, leading users to experience sleepiness, lack of physical coordination, dysphoria, and irritability. Continuing past this point, excessive drinking can be fatal as the individual's vital functions completely shut down. More severe effects also occur when the individual mixes alcohol with other drugs, a situation referred to as potentiation, meaning that the effects of two drugs taken together are greater than the effect of either substance alone. Combining alcohol with another depressant, for example, can be a fatal outcome of such potentiation.
- The rate at which alcohol absorption occurs in the bloodstream depends in part on a number of factors, including how much a person consumes, over what time period, and whether the person has food present in the digestive system. Another factor is the drinker's metabolic rate (the rate at which the body converts food substances to energy). The average person metabolizes alcohol at a rate of one-third of an ounce of 100 percent alcohol per hour, which is equivalent to an ounce of whiskey per hour. Following a bout of extensive intake of alcohol, a person is likely to experience an abstinence syndrome, or the phenomenon commonly called a “hangover.” The symptoms of abstinence syndrome include a range of phenomena including nausea and vomiting, tremors, extreme thirst, headache, tiredness, irritability, depression, and dizziness. As with alcohol absorption, the extent of abstinence syndrome reflects the amount and rate of alcohol consumption and the individual's metabolic rate.
- Alcohol affects almost every organ system in the body, either directly or indirectly. Long-term use of alcohol can lead to permanent brain damage, with symptoms of dementia, blackouts, seizures, hallucinations, and damage to the peripheral parts of the nervous system. Two forms of dementia are associated with long-term, heavy alcohol use: Wernicke's disease and Korsakoff's syndrome.
- Wernicke's disease is an acute and potentially reversible condition involving delirium, eye movement disturbances, difficulties in movement and balance, and deterioration of the peripheral nerves to the hands and feet. It is not the alcohol but a deficiency of thiamine (Vitamin B1) that causes Wernicke's disease. Long-term heavy use of alcohol has deleterious effects on the body's ability to metabolize nutrients, and such alcohol users often have an overall pattern of poor nutrition. Adequate thiamine intake can reverse Wernicke's disease.
- Korsakoff's syndrome is a permanent form of dementia in which the individual develops retrograde amnesia, an inability to remember past events, and anterograde amnesia, the inability to remember new information. The chances of a person recovering from Korsakoff's syndrome are less than one in four, and about another one in four people who have this disorder require permanent institutionalization.
- Chronic heavy alcohol consumption also causes a number of harmful changes in the liver, gastrointestinal system, bone density, muscles, and immune system. When people abruptly stop ingesting alcohol after periods of chronic usage, they can experience sleep disturbances, profound anxiety, tremors, and hyperactivity of the sympathetic nervous system, psychosis, seizures, or death.
The Alcohol Use Disorders Identification Test (“AUDIT”)-Scoring the AUDIT
Questions
| 0
| 1
| 2
| 3
| 4
| |
1. How often do you have a drink containing alcohol?
| Never
| Monthly or less
| 2 to 4 times a month
| 2 to 3 times a week
| 4 or more times a week
| |
2. How many drinks containing alcohol do you have on a typical day when you are drinking?
| 1 or 2
| 3 or 4
| 5 or 6
| 7 to 9
| 10 or more
| |
3. How often do you have 5 or more drinks on one occasion?
| Never
| Less than monthly
| Monthly
| Weekly
| Daily or almost daily
| |
4. How often during the last year have you found that you were not able to stop drinking once you had started?
| Never
| Less than monthly
| Monthly
| Weekly
| Daily or almost daily
| |
5. How often during the last year have you failed to do what was normally expected of you because of drinking?
| Never
| Less than monthly
| Monthly
| Weekly
| Daily or almost daily
| |
6. How often during the last year have you needed a first drink in the morning to get yourself going after a heavy drinking session?
| Never
| Less than monthly
| Monthly
| Weekly
| Daily or almost daily
| |
7. How often during the last year have you had a feeling of guilt or remorse after drinking?
| Never
| Less than monthly
| Monthly
| Weekly
| Daily or almost daily
| |
8. How often during the last year have you been unable to remember what happened the night before because of your drinking?
| Never
| Less than monthly
| Monthly
| Weekly
| Daily or almost daily
| |
9. Have you or someone else been injured because of your drinking?
| No
| Yes, but not in the last year
| Yes, during the last year
| |||
10. Has a relative, friend, doctor, or other health care worker been the last year concerned about your drinking or suggested you cut down?
| No
| Yes, but not in the last year
| Yes, during the last year
| |||
Total
| ||||||
Record the score for each response in the blank box at the end of each line, then total these numbers. The maximum possible total is 40.
Total scores of 8 or more for men up to age 60 or 4 or more for women, adolescents, and men over 60 are considere
- Twin, family, and adoption studies consistently point to the importance of genetic factors as contributors to alcohol-related disorders, with an estimated heritability of 50 to 60 percent. However, trying to pinpoint the genes involved in alcohol-related disorders is a great challenge to researchers, particularly for those who want to find genes that control the amount of alcohol consumption (Heath et al., 2011).
- Researchers are attempting to connect variations in some of these genes not only with patterns of alcohol use, but also with psychological factors, such as personality traits, and physiological factors, such as alcohol-related organ damage (Kimura & Higuchi, 2011). Large-scale analyses using genome-wide association studies are beginning to identify a large number of potential genes associated with alcohol use disorder that may pave the way toward understanding how the disorder develops (Wang et al., 2011). Using these new discoveries, researchers have already identified a relatively large number of genes, suggesting that alcohol use will not show a simple pattern of genetic transmission (Frank et al., 2012).
Physicians prescribe medications increasingly as biological treatment for alcohol use disorder if not as the sole form of treatment, then in conjunction with psychologically based therapies. A large number of well-controlled studies support the use of naltrexone as an aid in preventing relapse among people with alcohol use disorder. As an opioid receptor antagonist, it blocks the effects of the body's production of alcohol-induced opioids, perhaps through involving dopamine (Hillemacher, Heberlein, Muschler, Bleich, & Frieling, 2011). The individual who takes naltrexone is less likely to experience pleasurable effects of alcohol and even less likely to feel pleasure thinking about alcohol. As a result, people taking naltrexone feel less of an urge to drink and therefore will be less likely to suffer a relapse in which they engage in heavy drinking. An injectable form of naltrexone called nalmefene seems to be effective in promoting total abstinence (Garbutt et al., 2005).
Disulfiram is a medication that operates by the principles of aversion therapy. An individual taking disulfiram who consumes alcohol within a two-week period will experience a variety of unpleasant physical reactions, including flushing, palpitations, increased heart rate, lowered blood pressure, nausea and vomiting, sweating, and dizziness. Disulfiram works primarily by inhibiting the action of an enzyme that normally breaks down acetaldehyde, a toxic product involved in ethanol metabolism. Although not as effective as naltrexone, highly motivated individuals, particularly those treated in supervised settings who are also older, have a longer drinking history, and participate in Alcoholics Anonymous meetings, have used disulfiram effectively (Arias & Kranzler, 2008).
The third medication shown to be effective in treating alcohol use disorders is acamprosate, an amino acid derivative. Acamprosate reduces the risk of relapse by reducing the individual's urge to drink and thereby reducing the drive to use alcohol as a way of reducing anxiety and other negative psychological states. Acamprosate appears to work by modulating glutamate receptors and other reactions within the cell. Individuals who seem to benefit the most from acamprosate are those who are older when they become dependent on alcohol, have physiological signs of higher dependence, and have higher levels of anxiety, although in general, the evidence in favor of acamprosate is positive (Arias & Kranzler, 2008). People who are more highly motivated to become fully abstinent at the start of treatment are more likely to comply with remaining on the medication and therefore more likely to improve (Koeter, van den Brink, & Lehert, 2010).
- Researchers consider other medications used in the treatment of alcohol use disorders as less effective based on the available evidence. These include anticonvulsant medications, SSRIs, lithium, and baclofen, which works on GABA receptors (Arias & Kranzler, 2008).
- According to dual-process theory, one system involves fast, automatic processes that generate an impulse to drink alcohol. The more positive the associations that people have to alcohol, the more likely they are to consume it. Dual-process theory predicts that as individuals become better able to inhibit the automatic impulse to consume alcohol, they should also reduce their drinking behavior.
- The second system involves the controlled, effortful processing that regulates these automatic impulses. The more the individual can inhibit the automatic impulse, the less likely the individual is to consume excessive amounts of alcohol
- In general, alcohol expectancies involve an “if–then” set of contingencies: if I consume alcohol, then I can expect certain behaviors and effects to follow. Individuals develop alcohol expectancies early in life, even before they first taste alcohol. These expectancies can include the potential for alcohol to reduce tension, cope with social challenges, feel better, feel sexier, and become more mentally alert.
- According to alcohol myopia theory, as individuals consume greater amounts of alcohol, they are more likely to make risky choices because the immediate temptation of the moment (such as risky sex) overcomes the long-term consequences of the behavior (such as developing a sexually transmitted disease) (Griffin, Umstattd, & Usdan, 2010).
- There are several well-tested psychological approaches to treating alcohol use disorders. The most successful approaches involve cognitive-behavioral interventions, motivational approaches, and expectancy manipulation (Arias & Kranzler, 2008). Part of effective treatment for alcohol use disorders also involves relapse prevention, in which the clinician essentially builds “failure” into treatment. If the client recognizes that occasional slips from abstinence are bound to occur, then he or she will be less likely to give up on therapy altogether after suffering a temporary setback.
- The COMBINE project developed the most comprehensive protocol for psychological treatment as part of a project funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA). In this treatment, known as Combined Behavioral Intervention (CBI) (Miller, 2002), participants receive up to 20 sessions, according to their needs, beginning semiweekly and then eventually biweekly or less, for up to 16 weeks. The primary emphasis of CBI is on enhancing reinforcement and social support for abstinence. Clinicians assign motivational enhancement therapy at the outset, meaning that the clinician attempts to draw out the client's own motivation to change. The clinical style used in CBI follows from the motivational interviewing perspective (Table 12.2), in which the clinician uses a client-centered but directive style.
CLIENT: I guess I do drink too much sometimes, but I don't think I have a problem with alcohol.
CONFRONTATION: Yes you do! How can you sit there and tell me you don't have a problem when …
QUESTION: Why do you think you don't have a problem?
REFLECTION: So on the one hand you can see some reasons for concern, and you really don't want to be labeled as “having a problem.”
CLIENT: My wife is always telling me that I'm an alcoholic.
JUDGING: What's wrong with that? She probably has some good reasons for thinking so.
QUESTION: Why does she think that?
REFLECTION: And that really annoys you.
CLIENT: If I quit drinking, what am I supposed to do for friends?
ADVICE: I guess you'll have to get some new ones.
SUGGESTION: Well, you could just tell your friends that you don't drink anymore, but you still want to see them.
REFLECTION: It's hard for you to imagine how life would be without alcohol.
- Researchers and theorists working within the sociocultural perspective regard stressors in the family, community, and culture as factors that, when combined with genetic vulnerability, lead the individual to develop alcohol use disorder. Researchers gave support to the sociocultural perspective in a landmark longitudinal study in the early 1980s. Researchers followed individuals from childhood or adolescence to adulthood, the time when most individuals who become alcohol dependent make the transition from social or occasional alcohol use to have an alcohol use disorder (Zucker & Gomberg, 1986). Those most likely to develop alcohol use disorder in adulthood had a history of childhood antisocial behavior, including aggressive and sadistic behavior, trouble with the law, rebelliousness, lower achievement in school, completion of fewer years of school, and a higher truancy rate. These individuals also showed a variety of behaviors possibly indicative of early neural dysfunction, including nervousness and fretfulness as infants, hyperactivity as children, and poor physical coordination. Researchers concluded that these characteristics reflected a genetically based vulnerability, which, when combined with environmental stresses, led to the development of alcohol use disorder.
- The category of drugs called stimulants includes substances that have an activating effect on the nervous system. These differ in their chemical structure, their specific physical and psychological effects, and their potential danger to the user. Stimulants are associated with disorders involving use, intoxication, and withdrawal.
- Amphetamine is a stimulant that affects both the central nervous and the autonomic nervous systems. In addition to waking or speeding up the central nervous system, it also causes elevated blood pressure, heart rate, decreased appetite, and physical activity. It may be used for medical purposes, such as to treat ADHD or as a diet pill. Even when used for medical purposes, however, amphetamine drugs can cause dependence and have unpleasant or dangerous side effects. In increasingly large doses, users can become hostile, violent, and paranoid. They may also experience a range of physiological effects including fever, sweating, headache, blurred vision, dizziness, chest pain, nausea, vomiting, and diarrhea.
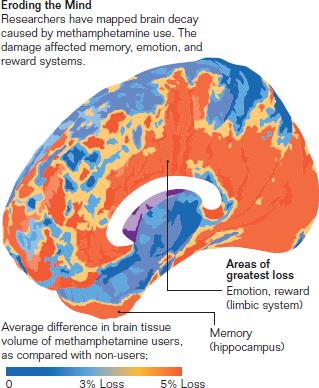
- Methamphetamine is an addictive stimulant drug that is related to amphetamine but it provokes more intense central nervous system effects. Whether taken orally, through the nose, intravenously, or by smoking, methamphetamine causes a rush or feeling of euphoria and becomes addictive very quickly. Methamphetamine overdose can cause overheating of the body and convulsions, and, if not treated immediately, it can result in death. Long-term use of methamphetamine can lead users to develop mood disturbances, violent behavior, anxiety, confusion, insomnia, severe dental problems (“meth mouth”), and a heightened risk of infectious diseases including hepatitis and HIV/AIDS. The long-term effects of methamphetamines include severe brain damage
- Cocaine is a highly addictive central nervous system stimulant that an individual snorts, injects, or smokes. Users can snort the powdered hydrochloride salt of cocaine or dissolve it in water and then inject it. Crack is the street name given to the form of cocaine that is processed to form a rock crystal which, when heated, produces vapors that the individual smokes. The effects of cocaine include feelings of euphoria, heightened mental alertness, reduced fatigue, and heightened energy. The faster the bloodstream absorbs the cocaine and delivers it to the brain, the more intense the user's high. Because this intense high is relatively short (5 to 10 minutes), the user may administer the drug again in a binge-like pattern.
- Mini Case
- Catherine is a 23-year-old salesperson who tried for 3 years to lose weight. Her physician prescribed amphetamines but cautioned her about the possibility that she might become dependent on them. She did begin to lose weight, but she also discovered that she liked the extra energy and good feelings the diet pills caused. When Catherine returned to her doctor after having lost the desired weight, she asked him for a refill of her prescription to help her maintain her new figure. When he refused, Catherine asked around among her friends until she found the name of a physician who was willing to accommodate her wishes for ongoing refills of the prescription. Over the course of 1 year, Catherine developed a number of psychological problems, including depression, paranoid thinking, and irritability. Despite the fact that she realizes that something is wrong, she feels driven to continue using the drug.
- Like amphetamines, cocaine increases bodily temperature, blood pressure, and heart rate. Cocaine's risks include heart attack, respiratory failure, stroke, seizures, abdominal pain, and nausea. In rare cases, the user can experience sudden death on the first use of cocaine or unexpectedly afterwards. Other adverse effects on the body develop over time and include changes within the nose (loss of sense of smell, chronically runny nose, and nosebleeds), as well as problems with swallowing and hoarseness. Users may also experience severe bowel gangrene due to a reduction of blood flow to the digestive system. Cocaine users may also have severe allergic reactions and increased risk of developing HIV/AIDS and other blood-borne diseases. When people use cocaine in binges, they may develop chronic restlessness, irritability, and anxiety. Chronic users may experience severe paranoia in which they have auditory hallucinations and lose touch with reality (National Institute on Drug Abuse, 2011b).
- Cannabis is associated with disorders involving use, intoxication, and withdrawal. Marijuana is a mix of flowers, stems, and leaves from the hemp plant Cannabis sativa, a tall, leafy, green plant that thrives in warm climates. Although the plant contains more than 400 chemical constituents, the primary active ingredient in marijuana is delta-9-tetrahydrocannabinol (THC). Hashish, containing a more concentrated form of THC, comes from the resins of the plant's flowers. The marijuana and hashish that reaches the street is never pure THC; other substances, such as tobacco, are always mixed in with it. Individuals use synthetic forms of THC for medicinal purposes, such as treating asthma and glaucoma and reducing nausea in cancer patients undergoing chemotherapy.
- Mini Case
- Gary, age 22, has lived with his parents since dropping out of college 3 years ago, midway through his freshman year. Gary was an average student in high school and, although popular, was not involved in many extracurricular activities. When he entered college, Gary became interested in the enticing opportunities for new experiences, and he began to smoke marijuana casually with his roommates. However, unlike his roommates, who limited their smoking to parties, Gary found that a nightly hit helped him relax. He started to rationalize that it also helped him study, because his thinking was more creative. As his first semester went by, he gradually lost interest in his studies, preferring to stay in his room and listen to music while getting high. He realized that it was easy to support his habit by selling marijuana to other people in the dorm. Although he convinced himself that he was not really a dealer, Gary became one of the primary suppliers of marijuana on campus. When he received his first semester grades, he did not feel particularly discouraged about the fact that he had flunked out. Rather, he felt that he could benefit from having more time to himself. He moved home and became friendly with some local teenagers who frequented a nearby park and shared drugs there. Gary's parents have all but given up on him, having become deeply discouraged by his laziness and lack of productivity. They know that he is using drugs, but they feel helpless in their efforts to get him to seek professional help. They have learned that it is better to avoid discussing the matter with Gary, because violent arguments always ensue.
Summary of Effects of Cannabis on Executive Functions
Executive Function Measured
| Acute Effects
| Residual Effects
| Long-Term Effects
|
|---|---|---|---|
Attention/concentration
| Impaired (light users)
| Mixed findings
| Largely normal
|
Decision making and risk taking
| Mixed findings
| Impaired
| Impaired
|
Inhibition/impulsivity
| Impaired
| Mixed findings
| Mixed findings
|
Working memory
| Impaired
| Normal
| Normal
|
Verbal fluency
| Normal
| Mixed findings
| Mixed findings
|
- Included in hallucinogen-related disorders are use and intoxication, but not withdrawal. Hallucinogens are drugs that cause people to experience profound distortions in their perception of reality. Under the influence of hallucinogens, people see images, hear sounds, and feel sensations that they believe to be real but are not. In some cases, users experience rapid, intense mood swings. Some people who use hallucinogens develop a condition called hallucinogen persisting perception disorder, in which they experience flashbacks or spontaneous hallucinations, delusions, or disturbances in mood similar to the changes that took place while they were intoxicated with the drug. The specific effects and risks of each hallucinogen vary among the four major categories of hallucinogens (National Institute on Drug Abuse, 2011c).
- Mini Case
- Candace is a 45-year-old artist who has used LSD for a number of years, because she feels that doing so enhances her paintings and makes them more visually exciting. Although she claims to know how much LSD she can handle, she is occasionally caught off guard and experiences disturbing side effects. She begins sweating, has blurred vision, is uncoordinated, and shakes all over. She commonly becomes paranoid and anxious, and she may act in strange ways, such as running out of her studio and into the street, ranting incoherently. On more than one occasion, the police have picked her up and taken her to the emergency room, where doctors prescribed antipsychotic medication.
- People take lysergic acid diethylamide (LSD) in tablets, capsules, and occasionally liquid form. Users show dramatic changes in their sensations and emotions. They may feel several emotions at once or swing rapidly from one emotion to another. At larger doses, users can experience delusions and visual hallucinations. In addition, they may feel an altered sense of time and self. Users may also experience synesthesia in which they “hear” colors and “see” sounds. These perceptual and mood alterations may be accompanied by severe, terrifying thoughts and feelings of despair, panic, fear of losing control, going insane, or dying. Even after they stop taking LSD, users may experience flashbacks, leading them to be significantly distressed and impaired in their social and occupational functioning.
- Unlike other substances, LSD does not seem to produce compulsive drug-seeking behavior, and most users choose to decrease or stop using it without withdrawal. However, LSD produces tolerance, so users may need to take larger doses to achieve the effects they desire. Given the unpredictable nature of LSD's effects, such increases in doses can be dangerous. LSD can also affect other bodily functions, including increasing body temperature, blood pressure, and heart rate, sweating, loss of appetite, dry mouth, sleeplessness, and tremors.
- Peyote is a small, spineless cactus whose principal active ingredient is mescaline. In addition to its naturally occurring form, individuals can also produce mescaline artificially. Users chew the mescaline-containing crown of the cactus, or soak it in water to produce a liquid; some prepare a tea by boiling the cactus in water to rid the drug of its bitter taste. Used as part of religious ceremonies by natives in northern Mexico and the southwestern United States, its long-term effects on these and recreational users are not known. However, its effects on the body are similar to LSD, with increases in body temperature and heart rate, uncoordinated movements, extreme sweating, and flushing. In addition, peyote may cause flashbacks, much like those associated with LSD.
- Psilocybin (4-phosphoryloxy-N,N-dimethyltryptamine), and its biologically active form, psilocin (4-hydroxy-N,N-dimethyltryptamine), is a substance found in certain mushrooms. Users brew the mushrooms or add them to other foods to disguise their bitter taste. The active compounds in psilocybin-containing mushrooms, like LSD, alter the individual's autonomic functions, motor reflexes, behavior, and perception. Individuals may experience hallucinations, an altered sense of time, and an inability to differentiate between fantasy and reality. Large doses may cause users to experience flashbacks, memory impairments, and greater vulnerability to psychological disorders. In addition to the risk of poisoning if the individual incorrectly identifies the mushroom from other mushrooms, the bodily effects can include muscle weakness, loss of motor control, nausea, vomiting, and drowsiness.
- Researchers developed phencyclidine(PCP) in the 1950s as an intravenous anesthetic, but it is no longer used medically because patients became agitated, delusional, and irrational while recovering from its effects. Users can easily mix the white crystalline powder with alcohol, water, or colored dye. PCP may be available on the illegal drug market in pill, capsule, or colored powder forms that users can smoke, snort, or take orally. When individuals smoke PCP, they may apply the drug to mint, parsley, oregano, or marijuana.
- PCP causes users to experience a sense of dissociation from their surroundings and their own sense of self. It has many adverse effects including symptoms that mimic schizophrenia, mood disturbance, memory loss, difficulties with speech and thinking, weight loss, and depression. Although these negative effects led to its diminished popularity as a street drug, PCP appeals to those who still use it because they feel that it makes them stronger, more powerful, and invulnerable. Furthermore, despite PCP's adverse effects, users can develop strong cravings and compulsive PCP-seeking behavior.
- Within MDMA-related disorders, the chemical named MDMA (3,4-methylenedioxymethamphetamine), known on the street as ecstasy, is a synthetic substance chemically similar to methamphetamine and mescaline. Users experience feelings of increased energy, euphoria, emotional warmth, distorted perceptions and sense of time, and unusual tactile experiences. Taken as a capsule or tablet, MDMA was once most popular among white teens and young adults at weekend-long dances known as “raves.” The drug is now used by a broader range of ethnic groups including urban gay males. Some users combine MDMA with other drugs including marijuana, cocaine, methamphetamine, ketamine, and sildanefil (Viagra), among other substances.
- Within opioid-related disorders are opiod use, intoxication, and withdrawal. An opioid is a substance that relieves pain. Many legally prescribed medications fall within this category, including hydrocodone (e.g., Vicodin), oxycodone (e.g., OxyContin, Percocet), morphine (e.g., Kadian, Avinza), codeine, and related drugs. Clinicians prescribe hydrocodone products most commonly for a variety of painful conditions, including dental and injury-related pain. Physicians often use morphine before and after surgical procedures to alleviate severe pain.
- Mini Case
- Jimmy is a 38-year-old homeless man who has been addicted to heroin for the past 10 years. He began to use the drug at the suggestion of a friend who told him it would help relieve the pressure Jimmy was feeling from his unhappy marriage and financial problems. In a short period of time, he became dependent on the drug and got involved in a theft ring in order to support his habit. Ultimately, he lost his home and moved to a shelter, where workers assigned Jimmy to a methadone treatment program.
- Heroin is a form of opioid. It is a pain-killing drug synthesized from morphine, a naturally occurring substance extracted from the seed pod of the Asian opium poppy plant. Users inject, snort, sniff, or smoke heroin. Once ingested, the body converts heroin to morphine and then it binds to the opioid receptors located in areas throughout the brain and body, particularly those involved in reward and pain perception. Opioid receptors are also located in the brain stem, which contains structures that control breathing, blood pressure, and arousal.
- Heroin is a form of opioid. It is a pain-killing drug synthesized from morphine, a naturally occurring substance extracted from the seed pod of the Asian opium poppy plant. Users inject, snort, sniff, or smoke heroin. Once ingested, the body converts heroin to morphine and then it binds to the opioid receptors located in areas throughout the brain and body, particularly those involved in reward and pain perception. Opioid receptors are also located in the brain stem, which contains structures that control breathing, blood pressure, and arousal.
- Users experience a surge of euphoric feelings along with a dry mouth, warm flushing of the skin, heaviness in the arms and legs, and compromised mental functioning. Shortly afterward, they alternate between feeling wakeful and drowsy. If users do not inject the drug, they may not feel euphoria at all. With continued use of heroin, users develop tolerance, meaning that they need larger amounts of the drug to feel the same effect. Heroin has a high potential for addiction with estimates as high as 23 percent of all users developing dependence (National Institute on Drug Abuse, 2011d).
- A sedative has a soothing or calming effect, a hypnotic induces sleep, and an anxiolytic is used to treat anxiety symptoms. These central nervous system depressant drugs can be useful for treating anxiety and sleep disorders. Their sedating effects are due to the fact that they increase the levels of the neurotransmitter GABA, which inhibits brain activity and therefore produces a calming effect. Disorders within this category include use disorder, intoxication, and withdrawal.
- Disorders included in the caffeine-related category are intoxication and withdrawal, but not caffeine use disorder. Caffeineis a stimulant found in coffee, tea, chocolate, energy drinks, diet pills, and headache remedies. By activating the sympathetic nervous system through increasing the production of adrenaline, caffeine increases an individual's perceived level of energy and alertness. Caffeine also increases blood pressure and may lead to increases in the body's production of cortisol, the stress hormone.
- The symptoms of caffeine withdrawal include headache, tiredness and fatigue, sleepiness and drowsiness, dysphoric mood, difficulty concentrating, depression, irritability, nausea, vomiting, muscle aches, and stiffness. Caffeine withdrawal is estimated to cause significant distress and impairment in daily functioning among 13 percent of people in experimental studies (Juliano & Griffiths, 2004).
- Mini Case
- Carla is a 19-year-old college sophomore who felt compelled to excel at every endeavor and to become involved in as many activities as time and energy would permit. As her commitments increased and her studies became more burdensome, carla became more and more reliant on coffee, soda, and over-the-counter stimulants to reduce her need for sleep. During final examination week, carla overdid it. For 3 days straight, she consumed approximately 10 cups of coffee a day, along with a few bottles of Aeroshot. In addition to her bodily symptoms of restlessness, twitching muscles, flushed face, stomach disturbance, and heart irregularities, carla began to ramble when she spoke. Her roommate became distressed after seeing carla's condition and insisted on taking her to the emergency room, where the intake worker recognized her condition as caffeine intoxication.
- The health risks of tobacco are well known; these risks are primarily associated with smoking cigarettes, which contain tar, carbon monoxide, and other additives. Nicotine is the psychoactive substance found in cigarettes. Readily absorbed into the bloodstream, nicotine is also present in chewing tobacco, pipe tobacco, and cigars. The typical smoker takes 10 puffs of a cigarette over a 5-minute period; an individual who smokes 1-1/2 packs of cigarettes therefore gets 300 “hits” of nicotine per day (National Institute on Drug Abuse, 2011a). Individuals can be diagnosed with tobacco use disorder or tobacco withdrawal, but not tobacco intoxication.
- When nicotine enters the bloodstream, it stimulates the release of adrenaline (norephinephrine), which activates the autonomic nervous system and increases blood pressure, heart rate, and respiration. Like other psychoactive substances, nicotine increases the level of dopamine, affecting the brain's reward and pleasure centers. Substances found in tobacco smoke, such as acetaldehyde, may further enhance nicotine's effects on the central nervous system. The withdrawal symptoms associated with quitting tobacco use include irritability, difficulties with concentration, and strong cravings for nicotine.
- Inhalants are a diverse group of substances that cause psychoactive effects by producing chemical vapors. These products are not in and of themselves harmful; in fact, they are all products commonly found in the home and workplace. There are four categories of inhalants: volatile solvents (paint thinners or removers, dry-cleaning fluids, gasoline, glue, and lighter fluid), aerosols (sprays that contain propellants and solvents), gases (butane lighters and propane tanks, ether, and nitrous oxide), and nitrites (a special category of products that individuals use as sexual enhancers). Young teens (ages 12 to 15) tend to inhale glue, shoe polish, spray paint, gasoline, and lighter fluid. Older teens (ages 16 to 17) inhale nitrous oxide, and adults (ages 18 and older) are most likely to inhale nitrites. Within the category of inhalant disorders, individuals can be diagnosed as having inhalant use disorder or intoxication, but not inhalant withdrawal.
- The effects of an inhalant tend to be short-lived; consequently, users try to extend their high by inhaling repeatedly over a period of several hours. Inhalants have similar effects as alcohol including slurring of speech, loss of coordination, euphoria, dizziness, and, over time, loss of inhibition and control. Users may experience drowsiness and headaches but, depending on the substance, may also feel confused and nauseous. The vapors displace the air in the lungs, causing hypoxia (oxygen deprivation), which is particularly lethal to neurons in the central nervous system. Long-term use may also cause the myelin sheath around the axon to deteriorate, leading to tremors, muscle spasms, and perhaps permanent muscle damage. The chemicals in inhalants can also cause heart failure and sudden death (National Institute on Drug Abuse, 2011e).
- Theories and Treatment of Substance Use Disorders
- Since all psychoactive substances operate on the reward and pleasure systems in the brain, similarities exist between the mechanisms through which individuals develop dependence on substances other than alcohol and the mechanisms involved in alcohol dependence itself. However, there are important differences related to the specific substance; for example, which receptor pathways the substance involves, the psychosocial factors associated with how users acquire dependence, and, ultimately, which methods are best suited to treatment.
- Biological Perspectives Research evidence clearly supports the importance of genetics in the development of serious substance problems. Extensive studies on humans and laboratory animals (mice) suggest possible genetic abnormalities in the opioid receptor on chromosome 1 (OPRM1) that may be involved in susceptibility to alcohol and other substances as well as sensitivity to pain. A second genetic abnormality appears on chromosome 15 in a cluster of nicotinic receptor subunits (CHRNA-3, 5, and 4) involved in nicotine dependence. The third is a widely studied abnormality affecting catechol-O-methyltransferase (COMT), which is associated with pain sensitivity, anxiety, and substance abuse (Palmer & de Wit, 2011). Researchers have linked alterations in the gene that codes the adenosine A2A receptor on chromosome 22 to individual differences in the consumption of caffeine and caffeine's effects on sleep, EEGs, and anxiety (Reissig et al., 2009).
- Compared to biological treatments for alcohol dependence, weak evidence exists for the efficacy of pharmacotherapies (Arias & Kranzler, 2008). There are no FDA-approved treatments for dependence on cocaine, methamphetamines, marijuana, hallucinogens, ecstasy, or prescription opioids. There are, however, several treatments for heroin dependence that are particularly effective when combined with behavioral interventions.
- Medically assisted detoxification is the first step in treatment of heroin dependence. During detoxification, individuals may receive medications to minimize withdrawal symptoms. To prevent heroin relapse, clinicians may use one or more of three different medications. Methadone is a synthetic opioid that blocks the effects of heroin by binding to the same receptor sites in the central nervous system. The proper use of methadone involves specialized treatment that includes group and/or individual counseling along with referrals for other medical, psychological, or social services. Developed over 30 years ago, methadone is not considered an ideal treatment because of its potential for dependence, even when combined with psychosocial interventions. Buprenorphine, approved by the FDA in 2002, produces less physical dependence, a lower risk of overdose, and fewer withdrawal effects. Originally developed as a pain medication, buprenorphine is also approved for treatment of opiate dependence. The FDA has also approved Naltrexone for heroin dependence, but it is not widely used because patients are less likely to comply with treatment.
- For nicotine dependence, clinicians may use biologically based treatments. Nicotine replacement therapies (NRTs), including nicotine gum and the nicotine patch, were the first FDA-approved pharmacological treatments. These deliver controlled doses of nicotine to the individual to relieve symptoms of withdrawal. Other FDA-approved products include nasal sprays, inhalers, and lozenges. However, the ability of the nicotine patch to treat nicotine dependence has come under question. In a follow-up study of almost 800 smokers, there were no differences in relapse rates among those who did and did not use the patch (Alpert, Connolly, & Biener, 2012). Other biological approaches to nicotine dependence are medications that do not involve delivery of nicotine, including bupropion (Wellbutrin), an antidepressant, and Varenicline tartrate (Chantix), which targets nicotine receptors in the brain.
- Psychological Perspectives The cognitive-behavioral approach to understanding substance use disorders provides an important counterpart to biological theories and treatments. Whether or not individuals with dependence on substances other than alcohol receive biologically based treatment, cognitive-behavioral therapy (CBT) is now widely understood to be a crucial component of successful treatment (Arias & Kranzler, 2008).
- The principles of treating substance use disorders other than alcohol through CBT are similar to those involved in treating alcohol dependence. As noted earlier in the chapter, there is also a high degree of comorbidity between alcohol and substance dependence. Well-controlled studies support the efficacy of CBT for populations dependent on a wide range of substances. Clinicians may combine CBT with motivational therapies, as well as with behavioral interventions that focus on contingency management. In addition, clinicians can readily adapt CBT to a range of clinical modalities, settings, and age groups. Given the limitations of medication-only treatment, CBT also provides an effective adjunct in both inpatient and outpatient clinics. The ability to help clients develop coping skills is also useful in fostering compliance with pharmacotherapies such as methadone and naltrexone. Because these interventions are relatively brief and highly focused, they are adaptable to clients treated within managed care who may not have access to longer-term treatment (Carroll, 2011).