An Episode of Moral Distress in Nursing
Key Values and Factors in the Event
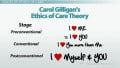
Chinn and Kramer (2011) recognized that values assist us to form moral questions and actions (p. 99). The nursing staff for this mentally handicapped man saw that he was not fully informed of his health using appropriate age-related methods. He did not understand that death was imminent because his education level was not considered when the healthcare team spoke with him. The nursing unit caring for the patient was an adult unit that did not commonly care for the mentally handicapped. Also, the patient did not have a trusted support person present at the bedside that he could seek comfort in. His sister was his only family and she did not want to be present for the end of her brother’s life. The nursing staff took turns at the bedside attempting to comfort him while he was awake, but he remained anxious and fearful until large amounts of medication was given. These factors support that the medical staff lacked the emancipatory and aesthetic knowing required to prevent this event of moral distress.
Moral Distress with Death and Dying
Action is not always clear as ethical situations can be complex (Chinn & Kramer, 2011, p. 87). One particular situation that caused moral distress involved end-of-life care for a 60 year old mentally handicapped male. The patient was diagnosed with end stage chronic obstructive pulmonary disease after smoking 3 packs per day for an estimated 40 years. He was experiencing respiratory distress, requiring mechanical ventilation, and was not able to fully understand possible outcomes. His sister was his power of attorney for healthcare and chose to sign a do not resuscitate order and make the patient comfort measures only. The physicians and residents made attempts to explain prognosis and the care plan to the patient, but he never fully understood. The patient experienced fear, anxiety, and loneliness as his sister did not stay with him at the hospital after meeting with the healthcare team. The patient was treated for pain and anxiety, but he continued to cry and yell out until he was unresponsive. The most memorable event during comfort care was the patient crying out “I don’t want to die” on a repetitive basis making the nursing staff emotional and uncomfortable with the situation.

Article Review: Moral Distress
I reviewed an article that studied the perceptions and responses to moral distress by critical care nurses. Some of the conflicts discussed involved teaching institutions with physicians in training and inaccurate and incomplete information given to patients and families. (Gutierrez, 2005). The moral distress situation I presented occurred in a teaching hospital and the patient was cared for by a physician teaching team. The physician team did not have experience working with the mentally handicapped population to ensure information was presented properly. Gutierrez states that moral conflicts can impact nurses professionally by decreasing their desire to come to work, decreasing their interactions with families, and by decreasing their willingness to care for the patient involved in the conflict (2005). Furthermore, nurses described having feelings of sadness, frustration, and anger following moral conflicts and the sole support in coping was other staff nurses (Gutierrez, 2005).
The article assisted me to identify several ways the distress experienced by the nursing staff could have been impacted. Nursing management has a primary role of supporting the bedside nurse with care issues and attention should be demanded (Gutierrez, 2005). The Unit Manager was not involved with the situation of the dying patient but could have sought out further resources for the staff had she been notified. Next, Gutierrez recommends improved communication and collaboration within the healthcare team with the use of ethics rounds (2005). Many institutions I have visited, including the teaching hospital the situation occurred in, currently partake in interdisciplinary rounding which usually exclude the patient and family. The ethics rounds that Gutierrez describes involve the patient and families with the healthcare team, giving them the opportunity to discuss openly any moral concerns and give coping support (2005). Also, development of organizational guidelines for palliative care and forums for ethical discussions are recommended (Gutierrez, 2005). Increasing nursing knowledge of ethical situations can raise awareness of support and resources. A forum would provide nurses a place to voice concerns and develop coping abilities (Gutierrez, 2005).
Impact of Higher Education
Nurses in the healthcare profession look to their leaders for guidance and direction. Transitioning to the role of MSN will involve not only growth in knowledge and critical thinking, but maturity in performing as a professional. According to Chinn and Kramer (2011), “moral/ethical comportment requires the consideration of all other knowing patterns in the moment of practice” (p.103). Moral distress among nurses can cause burnout, increased turnover, and abandonment of the profession (Gutierrez, 2005). It is the nursing leader, acting as the change agent, which can impact these issues and support a system of healthcare that focuses on patient needs and goals that utilizes collaboration among healthcare providers (Gutierrez, 2005).
Poll: Formal Ethics Committees
Does Your Workplace Have an Ethics Committee?
What About an Ethics Course?
I attended a BSN program that incorporated ethics education as part of the senior second semester Perspectives course. It was taught by an individual who was not a nurse, but had his Doctorate in Philosophy and was involved in many committees both in the hospital my school was affiliated with and the Catholic churches in the area. The instructor taught directly from the Code of Ethics and incorporated some ideals from the Catholic Church as well. I do not remember specifics involved with the Catholic teachings, but he included many situations and case studies that the Ethics Committee was involved in.
The course did give a framework of knowledge to build on. I at least had knowledge of the Ethics Committee, how it was used and consulted, and what situations to consider it for. According to Chinn and Kramer (2011), background and situational experiences largely determine morality (p. 90). As a new nurse emerging from my BSN program, I incorporated my values and beliefs already existing with those presented in my ethics course. “Nursing’s mortality is, in large measure, an everyday ontology” (Chinn & Kramer, 2011, p. 98).

Functions of Ethic Committees
- Preserve respect for human dignity
- Preserve the right to self-determination
- Primacy of the patient's interests
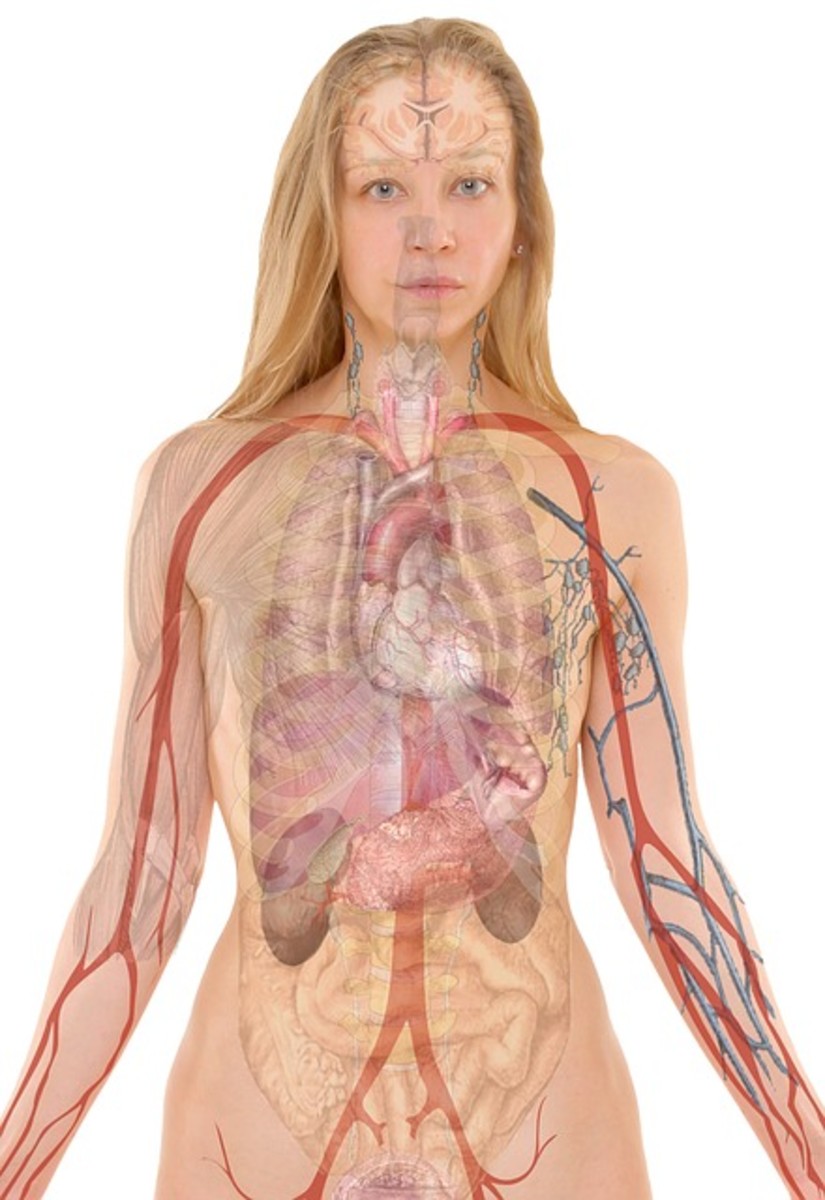
Illegal Substances and Terminal Cancer
. I admitted a patient that was being cared for at home with hospice, having terminal nasopharyngeal cancer. She was still able to speak in a whisper, but was unable to eat and used enteral feedings through a gastric tube due to her condition. She told her husband while at home that she had taken several of his blood pressure pills, crushed them, and administered them in her gastric tube. He notified hospice who in turn notified emergency services. The patient was admitted to the hospital, full code status, and a toxicology screen done per protocol. She was found to be positive for cocaine in addition to other medications that were prescribed. When attempting to have therapeutic discussion with this patient, she also disclosed that she used cannabis and crack and was using beer instead of her prescribed enteral feedings. She also denied wanting to hurt herself or die, but admitted to using these substances for coping with the situation. The situation caused moral distress due to the patient being terminal and using illegal substances to cope.
As a nurse, how do I teach a patient the dangers of illegal substances when the patient is terminal? According to Chinn and Kramer (2011), “care must be balanced with a concern for justice; rules must be used in the context of doing the least harm or benefiting people in some way” (p. 104). I refrained from my standard drug lecture and instead discussed support systems and coping mechanisms. I found through our discussions that her husband, who did not accompany her to the hospital, shared in her despair and was coping by using drugs. I worked very hard to develop rapport with this patient in my shift, but did not work again for several days after. I found myself worried during the next shift I worked, thinking about this patient, what happened to her, and how social services may have helped. Ethical issues that remain unresolved contribute to moral distress, burnout, errors, and potentially harmful decisions (Pavlish, Brown-Saltzman, Hersh, Shirk, Nudelman, 2011). Because of this, ethics and quality care should remain inseparable (Pavlish et al., 2011).
A Witch Doctor in the Hospital?
The patient was a roofer that suffered hyperthermia and was not found for 6 hours. He was no longer neurologically intact and required continuous ventilator support. The length of stay had reached 30 days when the family brought to the attention of the physician that they were flying in a witch doctor and wanted to withdraw care upon arrival.
The mention of witch doctor caused immediate outrage with the physicians on the case. The family’s culture was unknown to the healthcare team and one physician judgmentally stated he envisioned a man in a bone costume that would perform blood-letting. The nursing staff were segregated in acceptance, with one group dismissing the idea as absurd while the other group showing the family support in embracing their culture and grieving the loss of the person he used to be. The moral distress of the situation not only involved the disagreement of the healthcare team with each other, but included was caring for a young man who was now vent dependent and would no longer function as he did before.
Another mentionable factor was the hospital was catholic and the ethics committee was mostly the pastoral care staff. The nursing staff was sure the ethics committee would prevent the witch doctor from performing any rituals. The hospital however, always advertised that they did not discriminate against any culture or religion and had representatives from various cultural backgrounds on call for unique patient situations. They determined that the witch doctor may perform rituals that were non-invasive, did not involve fire, and a member of the healthcare team must be present to enforce institutional safety standards.

References
Chinn, P., & Kramer, M. (2011). Integrated theory and knowledge development in nursing (8th Ed.). Mosby Elsevier: St. Louis, Missouri.
Gutierrez, K. M. (2005). Critical Care Nurses5 Perceptions of and Responses to Moral Distress. Dimensions of Critical Care Nursing, 24(5), 229-241. Retrieved from EBSCOhost.
Pavlish, C., Brown-Saltzman, K., Hersh, M., Shirk, M., & Nudelman, O. (2011). Early Indicators and Risk Factors for Ethical Issues in Clinical Practice. Journal of Nursing Scholarship, 43(1), 13-21. doi:10.1111/j.1547-5069.2010.01380