6 Facts about Heart Attack
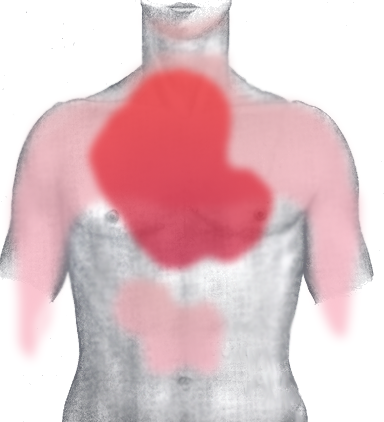
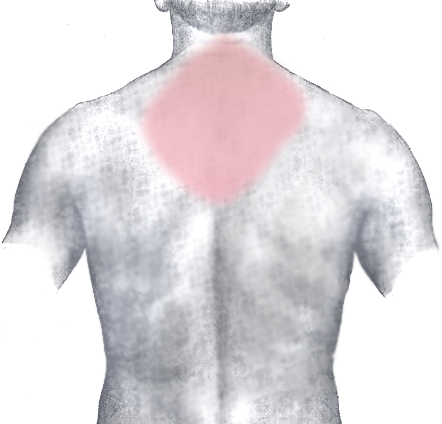
Acute MI-Pain Distribution-Chest
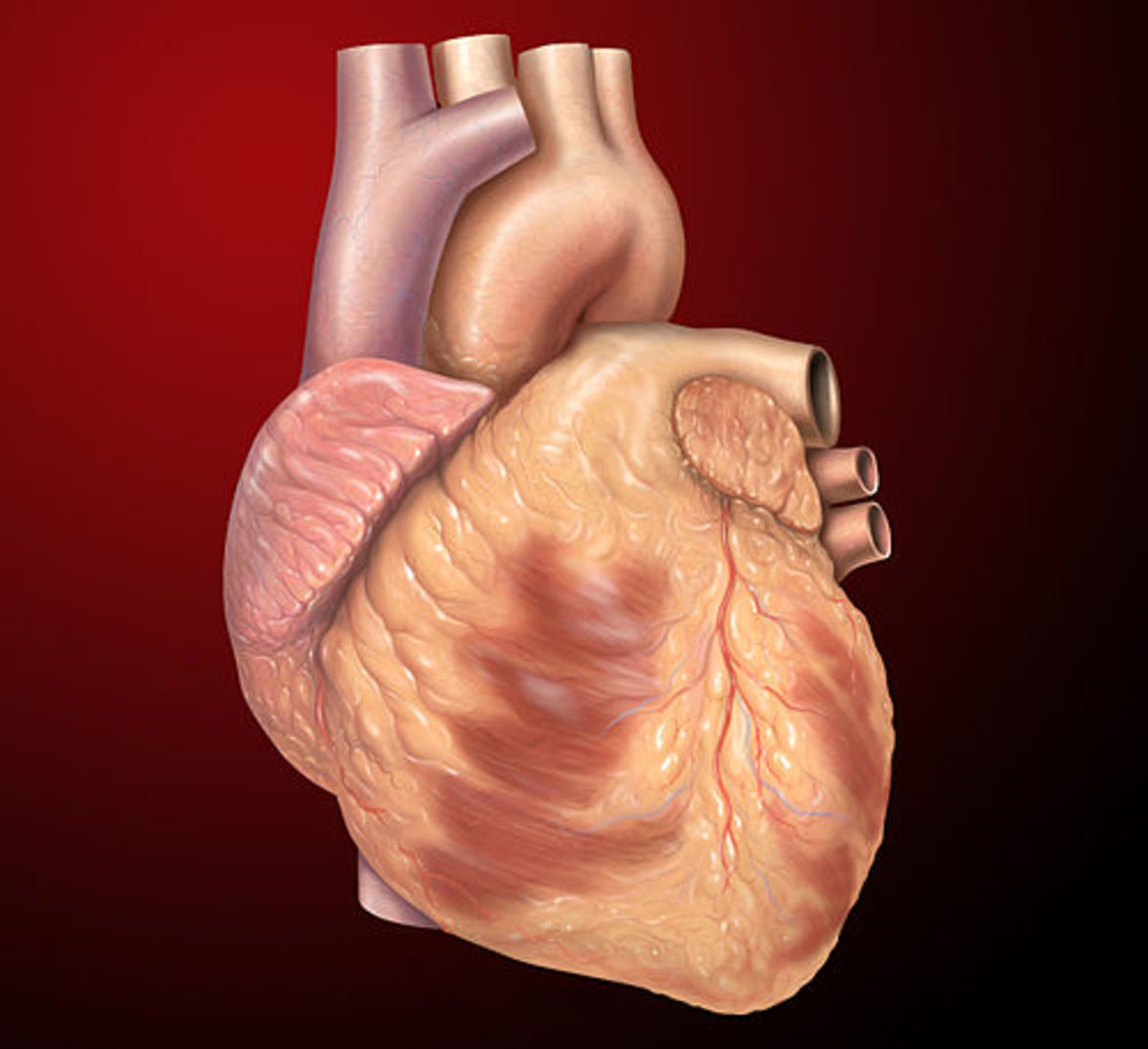
Myocardial Infarction (Heart Attack) - Introduction
Myocardial Infarction (Heart Attack) results from the acute occlusion of one of the coronary arteries causing death/necrosis of myocardium supplied by that particular vessel. When the blood vessel is occluded it may result in complete deprivation of blood supply to the area.
Coronary arteries are the blood vessels supplying the heart.
Prevent Heart Attack
What Measures Do You Take to Prevent Heart Attack?
1. How do we get Pain in Myocardial Infarction?
When the blood supply to the myocardium is deprived, it will result in inadequate oxygen to the myocardium and the myocardial tissue dies.
-
The inadequate blood supply or in other terms, ischemia can activate anaerobic metabolism because of the lack of oxygen.
-
Anaerobic metabolism produces lactate which irritates the nerve endings in the myocardium.
-
Patient experiences retrosternal chest pain and the pain may radiate to neck, jaw, left shoulder and anterior aspect of forearm.
-
Pain of Myocardial infarction is very severe and usually lasts for more than 30 min.
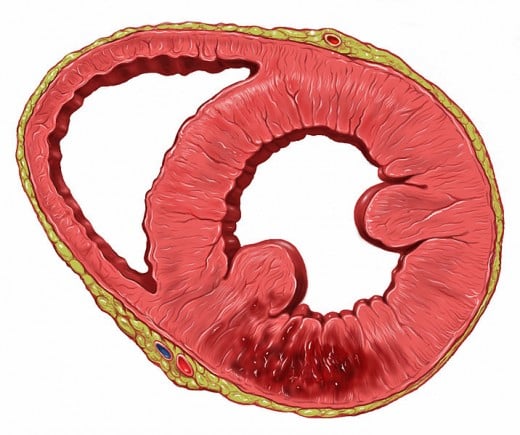
Heart-Inferior wall Infarct
Heart Attack-Pain Distribution-Back
Prevent Heart Attack
2. Factors contributing to the development of Myocardial Infarction
Certain non-modifiable risk factors contributing to the development of Myocardial Infarction are
-
Age – Men and women who are older are 50 years of age more likely to get Myocardial Infarction than younger people
-
Sex- Males are more at risk than females
-
Family historyof premature coronary artery disease–Family history is another risk factor which cannot be modified
Modifiable risk factors include
-
Diabetes
-
Tobacco usage
-
Hypercholesterolemia
-
High blood pressure
-
Obesity
-
Stress
-
Lack of physical activity
3. Cause for Myocardial Infarction
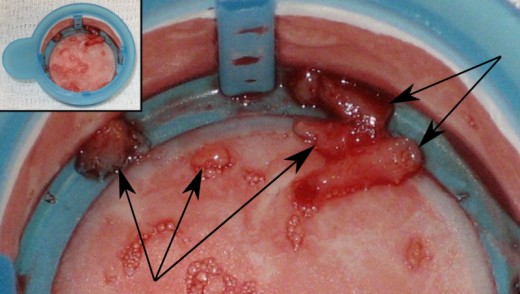
Atherosclerosis or deposition of fat within the wall of the blood vessels supplying the heart is the most important cause for the development of Myocardial Infarction. Deposition of fat streaks within the blood vessel wall will reduce the lumen of the vessel wall and reduce the blood supply. Many changes like fissuring and ulceration can occur to the fatty plaque. This results in fatty core of the plaque coming in contact with blood and as a result the development of thrombus starts. Thrombus formation further reduces the blood supply to the myocardium.
Intracoronary thrombus removed from a coronary artery during a percutaneous coronary intervention to abort a myocardial infarction. Five pieces of thrombus are
4. TYPES OF MI and the changes in ECG leads in each type
Myocardial Infarction affects the different areas of the heart depending on which blood vessel is occluded.
¨ Anterior wall- V3 &V4
¨ Lateral Wall-1, aVL, V5, V6
¨ Inferior wall-II, III, aVF
¨ Septum-V1 & V2
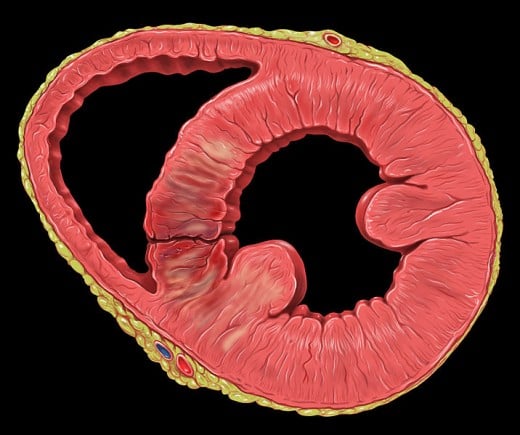
Heart-Posterior wall infarct with VSD
5. Symptoms of Myocardial Infarction
- Pain –Pain of myocardial infarction is severe lasting more than 30 minutes. Usually pain is felt substernally or retrosternally (behind the sternum). Pain may also radiate to the jaw, shoulder and arm.
There may also be associated discomforts like
-
Difficulty in breathing
-
Pallor
-
Nausea, vomiting
-
Fatigue
-
Increased heart rate and fall in blood pressure
-
Excessive sweating
6. Management of Myocardial Infarction
The first aim of treating MI is to restore blood supply (perfusion) to the damaged myocardium.
The treatment can be different in to the phases like
Pre hospital care
-
Alert the emergency department
-
Oxygen administration
-
ECG and Pulse oximetry monitoring
-
Nitroglycerin sublingual
-
Aspirin
-
Establish an IV line
-
Transport the patient to the emergency room as early as possible
Management at the emergency department
-
Continue with supplemental oxygen, pulse oximetry and ECG monitoring
-
Nitroglycerin may need to be continued; observe for hypotension, bradycardia
-
Intractable pain is treated with Morphine
-
Differentiate between STEMI, NSTEMI or Unstable Angina and treatment to be initiated accordingly (thrombolysisVs. PCI)
In-Hospital treatment
The aim is to observe, minimize the damage to the myocardium and to recanalise the affected arteries.
Patient may be given beta blockers, morphine, aspirin, nitroglycerin and statins to reduce cholestrolemia. Depending on the need patient may be taken for PCI or CABG.
Other health related hubs
- Cancer Related Fatigue – Factors Influencing
Fatigue can be a side effect of cancer treatment. Generally, the treatments of cancer include surgery, chemotherapy, radiation therapy and hormone therapy. Even though there are many other side effects of cancer therapy, cancer related fatigue is the - Chemotherapy for cancer; Fear of side effects;Would ...
Chemotherapy is one of the mainstay treatments for cancer. The fear of development of side effects and the cost of getting chemotherapy should not prevent you from seeking treatment if you have cancer. Studies have proved that chemotherapy can extend