Infections: Pathogenesis, A General Clinical Overview And Health Relevance To Man
A Model Showing Blood Bound Pathogens Causing Infections
Pathogenesis
After gaining access to the body, the infecting organisms adhere to their site of primary attack by finbriae (pili) or surface antigens. The next step is to multiply and produce a local lesion. Further spread occurs by contiguity to tissues and tissue spaces. Distant spread occurs through the lymphatics and blood stream. Once the organisms have multiplied to reach sufficient numbers and the target organs have sufficient numbers and the target organs have been involved, clinical disease manifests. Some organisms like C. diphtheria and cl. Tetani do not spread but they multiple locally and elaborate toxins which are absorbed into the system. The exotoxins cause the adverse effects. The body’s mechanisms to prevent and overcome infections are the local defences, phagocytic cells and nonspecific defecne aids such as lysozyme, complement and properdin. If the organism overcomes these initial defences, it multiplies and invades the tissues. At this stage, the body mounts it humoral and cellular defence mechanisms. The ultimate outcome of the infection depends on the interaction between the microbe and the defecne forces of the host. If the latter fails, the host succumbs.
The ability of the host to put up defence forces depends on seeral factors such as the genetic make up, age, nutrition, hormonal influences, constitutional diseases and drug therapy. The factors pertaining to the parasites are its pathogenecity, virulence and dosage. The capacity of the parasite to produce disease is its pathogenicity which is a qualitative character and the degree of pathogenecity of an organism is its virulence. Virulence is a quantitative character. Pathogenecity is a characteristic of the species of microbes whereas virulence is a characteristic of any particular strain.
The Anopheles Stephensi As An Example Of An Infection Causing Vector

Health Significance To Man
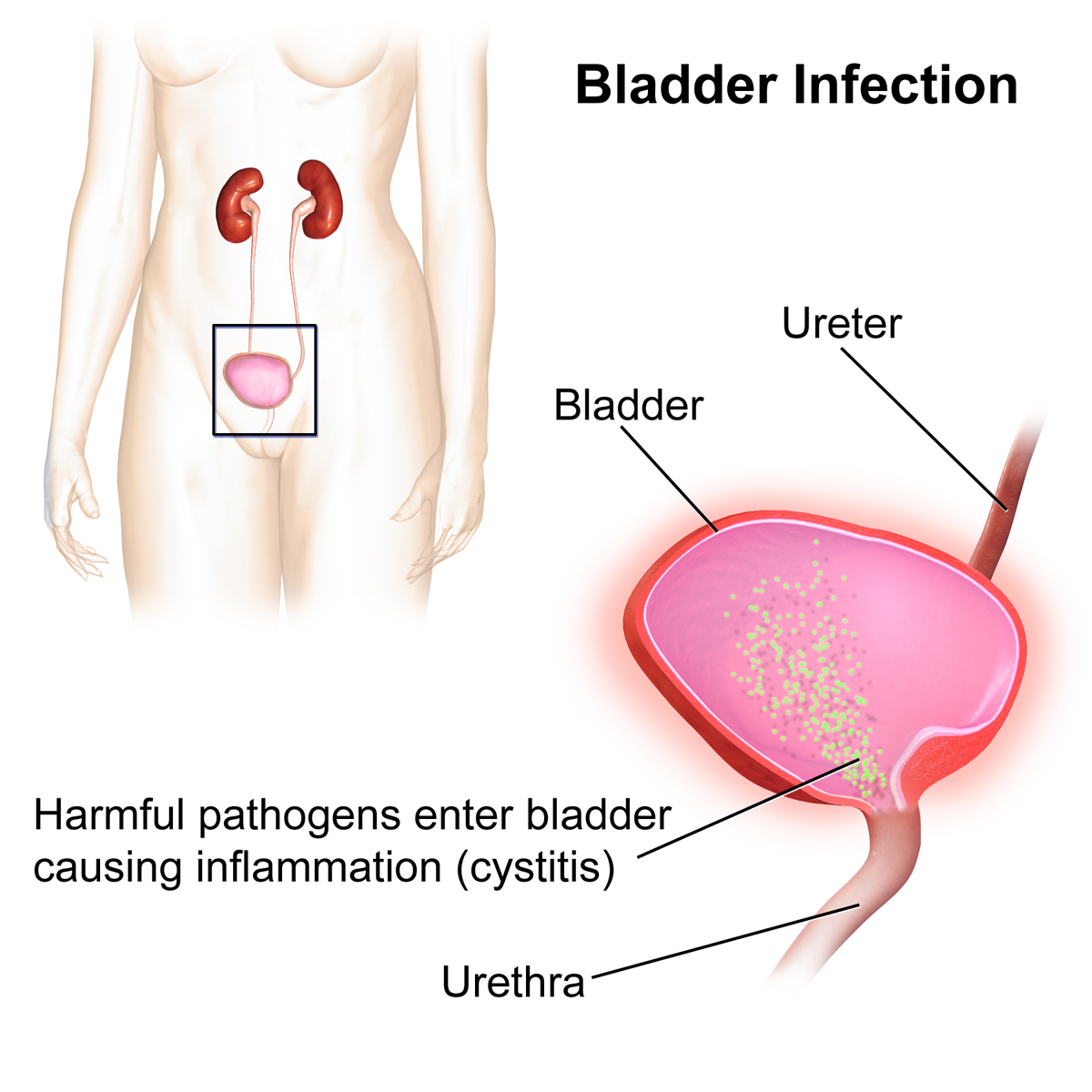
In some instances, the host defences may be suppressed, mainly on account of therapeutic procedures. Such a host is called compromised host. The abnormality in the host defence mechanism may involved the leucocytes, immunoglobulins, complement, vascular supply, mucosal and epithelial barriers, alterations in the normal bacteria flora or presence of foreign bodies such as a catheter, endotracheal tuber or artificial heart valve. Suppression of normal bacterial flora may lead to superinfection with pathogens such as Pseudomonas and Candida Spp. Microorganisms acquire resistance to antibiotics through transfer of plasmids from other coexistent resistant bacteria or by developing alternate metabolic pathways.
Infections acquired in hospitals are causing considerable morbidity and mortality all over the world in the present era of extensive use of antibiotics and invasive methods of investigations and treatment. Mainly, these are caused by Gram- negative bacilli, but staphylococci, streptocci and Candidia spp. Are also frequent offenders. The common nosocomial infections are urinary tract infections, wound infections, pneumonia, hepatitis and septicemia.
Most nosocomial infections are preventable if the important fact that antibiotics are not the alternative to restrict sepsis is born in mind. Provision of infection control teams which must monitor and investigate all outbreaks of nosocomial infections and advise and initiate all remedial and corrective measures will go a long way to reduce nosocomial infection in all major hospitals. Indisciminate use of antibiotics should be discouraged. Every major hospital must have an antibiotic policy laying down the guidelines for employment of antibiotics. At least a few antibiotics should be reserved for use against resistant organisms.