Pyrexia Of Unknown Origin (PUO) And Diagnostic Methods In Infectious Diseases
Severity Of Fever

Etiology And Diagnosis Of Pyrexia
When the temperature is raised above 38.30C for more than two weeks without the cause being detected by physical examination or laboratory tests, it comes under the definition of PUO. This presents one of the most difficult diagnostic problems in medicine. Atypical manifestations of common illnesses are responsible for the majority of such cases. Though in the vast majority of cases, the cause can be detected by repeated investigations and observation, in a few the cause may be obscure even at autopsy.
Etiology
- Occult tuberculosis: Affection of the lymph nodes, vertebrae, joints, intestines, mesentery, liver and rarely the lungs and pleura may remain latent without any obvious local symptoms. Fever may be the only presenting symptom, and all investigations including the tuberculin test may be negative. The local lesions may become evident only after several weeks or months.
- Chronic suppurative lesions of the liver, pelvic organs, urinary tract, peritoneum, gall bladder, brain, lungs and bones and joints may all manifest as prolonged fever without producing local symptoms. Other foci of suppuration which are likely to be missed are the perinephric, subdiaphragmatic and pelvic absecces, and paranasal sinuses. Dental sepsis, which is likely to be considered insignificant, may at times be the cause of prolonged pyrexia.
- Viral Infections: Infectious mononucleosis, cytomegalovirus infections, viral hepatitis.
- Connective tissue disorders: Systemic lupus erythematosus, polyarteritis nodosa, rheumatoid arthritis, rheumatic fever, giant cell arteritis.
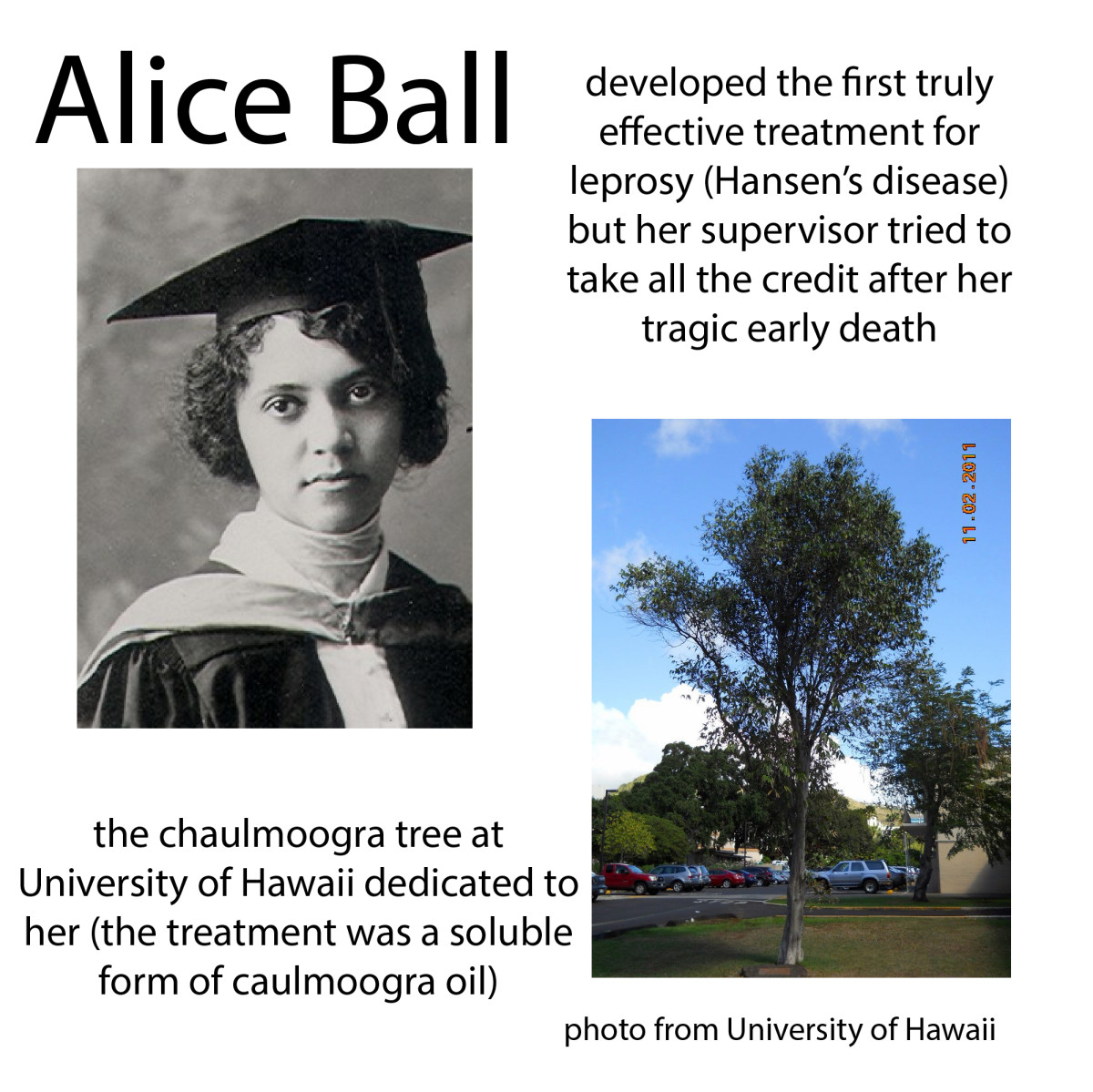
- Chronic infections: syphilis, hepatic amoebiasis, malaria, filariasis, leprosy, recurrent bacteremias in cirrhosis, liver infective endocarditis, bruccellossi and sarcoidosis.
- Hematological malignancies: Leukemias, lymphomas, multiple myeloma
- Other malignant lesions: Tumours of the gastrointestinal tract, liver, lungs and kidneys
- Allergic conditions: Drug allergy, other external allergens.
- Miscellenious conditions: Hemolytic anemia, multiple venous thrombosis, recurrent pulmonary embolism, anxiety state, dehydration in infants.
- Fictitious fever: Fever may be self induced by patients with psychological abnormalities with a view to deceive the physician and gain sympathy. Such patients may either infect themselves with bacteria to produce fever or they may devise methods to make the thermometer record a high temperature even when they are normal.
Diagnosis
Careful attention to history and repeated physical examination serve to reveal the etiology in many cases. The investigations have to be repeated at weekly intervals and any fresh clinical clue such as appearance of a lymph node or local tenderness should suggest the appropriate investigation. Despite prolonged observation and repeated investigations, a small proportion of cases remain undiagnosed. In them, the fever may subside either spontaneously or with symptomatic treatment.
A Child With Mild Fever

Diagnostic Methods In Infectious Diseases
Laboratory tests commonly undertaken in the diagnosis of infections include the following:
- Microscopic examination to detect the causative organisms in exudates, secretions, excretion and body fluids by staining, immunofluorescent procedures, phase contast, dark ground or electron microscopy.
- Isolation of the organism by culture/animal inoculation.
- Demonstration of antibodies by serology.
- Demonstrating hypersensitivity states by skin tests.
- Histopathology and isolation of the organism using biopsy specimen.
List of Materials To Be Sent To The Laboratory For Isolation Of Common Bacterial Pathogens
Probable infecting agent
| Specimen to be sent
|
|---|---|
Staphylococci
| Exudates, tissue, blood, serum, swabs from anterior nares and throat (in case of carriers)
|
Streptococci
| |
i. streptococcus Pyogenes
| Exudates, throat swabs, high vaginal swab, blood, serum
|
ii. other beta and alpha hemolytic streptococci
| Exudates, blood culture
|
Pneumococci
| Sputum, CSF, blood culture, exudates, throat swab.
|
Meningococci
| CSF, blood cultures, postnasal swabs (in carriers)
|
Gonococci
| Exudates from urethra, cervix, rectum, throat swab, conjunctiva, serum
|
Bacillus Anthracis
| Exudate, blood culture, sputum, feces
|
Corynebacterium diphtheriae
| Membrane (exudates) throat swab, nasal swab, ulcer swab
|
Clostridia
| Exudate, tissue, blood culture, food, feces
|
Mycobacteria
| |
i. Tuberculosis
| Sputum, exudates, CSF, urine, biopsy material
|
ii. Leprosy
| Skin- clipping, sputum, biopsy nerve and nasal swab.
|
Leptospirae
| Blood, Serum, Urine
|
Treponema Pallidum
| Exudate, Serum
|
Salmonella
| |
i. Enteric fever
| Blood, feces, urine, serum
|
ii. Food poisoning
| Feces, vomit, food, blood cultures
|
Shigella
| Feces
|
Vibrio cholera and Eltor strain
| Feces
|
Brucella
| Blood, serum
|
Yersinia Pestes
| Exudate, aspirate from bubo, blood, sputum, serum
|
Hemophilus Influenzae
| Sputum, CSF, blood, exudates from eye
|
Bordetella Pertussis
| Pharyngeal or laryngeal swab, cough plate, throat washings
|
Pseudomonas And Proteus
| Urine, exudates, CSF and Urine, exudates
|
Careful recording of history, physical examination and necessary supportive laboratory investigations form the cornerstone of proper diagnosis. A provisional diagnosis has to be concluded on history of patient, clinical examinations and preliminrary investigations such as urinalysis, blood counts and X-rays. Further investigations have to be planned depending on the provisional diagnosis. To get reliable laboratory reports, the collection and transport of the specimen should be properly done. Laboratory results should be interpreted in the light of the clinical findings.
© 2014 Funom Theophilus Makama