The Science behind Over the Counter Pain Relievers

The advances in drug discovery these days are amazing. There are not only life-saving drugs in the realm of cardiovascular disease and lung disease but also palliative medicines vastly improving the quality of life for patients living with arthritis and cystic fibrosis. Drug mechanism of action is fascinating because when you get down to the simplest drugs, over the counter (OTC) pain relievers, there is still a complex internal process and mode of action in order to understand how your aspirin makes that pounding headache go away. Let’s look at analgesics- pain relievers-and see how they do what they do to relieve our aches and pains.
Brand Name
| Drug Name
|
|---|---|
Tylenol
| Acetaminophen
|
Bayer
| Aspirin
|
Advil
| Ibuprofen
|
Motrin
| Ibuprofen
|
Aleve
| Naproxen Sodium
|
All of the following are NSAIDs, non-steroidal anti-inflammatory drug, except acetaminophen.
The big four, in terms of OTC pain relievers, are acetaminophen, ibuprofen, aspirin, and naproxen sodium. All four are listed as fighting minor aches and pains, including headache and the common cold. So what’s the difference between them? Well a major difference is the drug class- a distinction that separates acetaminophen from the others. Aspirin, ibuprofen, and naproxen are all NSAIDs- Non-Steroidal Anti-Inflammatory Drugs, while acetaminophen is not. The pain relief NSAIDs provide comes with serious potential side effects- severe stomach bleeding and kidney failure. Acetaminophen on the other hand has very few side effects when taken appropriately.
Indications of OTC Pain Relievers
Minor Aches and Pains
| Headache
| Toothache
|
Inflammation
| Minor Arthritis
| Menstrual Cramps
|
Fever Reducer
| Common Cold
|
Aspirin & Prostaglandins
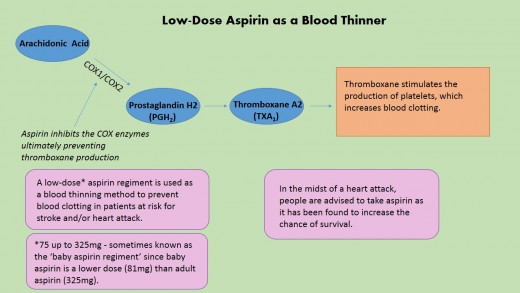
Aspirin is the one that started it all, discovered just before 1900; it comes from the family that includes salicylate and indomethacin. Aspirin or acetylsalicylic acid is an analgesic, meaning pain-reliever, an antipyretic, meaning fever-reducer, and an anti-inflammatory. In the early 70s the mechanism of action of aspirin was fully pinned down and it was proven to cause dose-dependent inhibition of prostaglandin (PG) production. The rate limiting enzyme in the PG synthesis process is cyclo-oxygenase (COX), which also goes by several varieties of the name prostaglandin synthase. The COX enzyme allows for two structural changes in arachidonic acid, a fatty acid, converting it first to Prostaglandin G2 (PGG2) and then reducing it to Prostaglandin H2 (PGH2). PGH2 can then be shuttled to a variety of different enzymes to form many different types of prostaglandins.
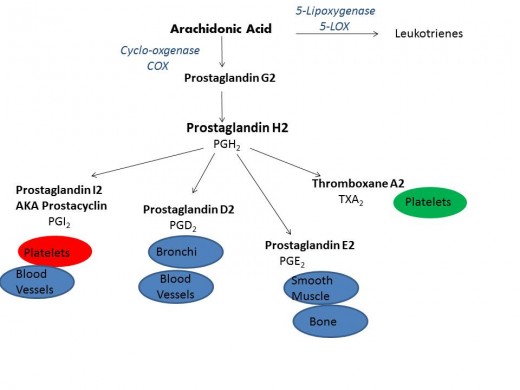
Prostaglandins are a class of chemical signals- a cousin to hormones- that mediate a variety of bodily functions. Pertinent to this conversation PGs are involved in pain, inflammation, platelet aggregation, kidney function, and mucous production in the gastrointestinal (GI) tract. But overall PGs have many diverse roles in many different body systems and processes including the reproductive cycle, bone metabolism, and nerve function. Prostaglandins protect the lining of the stomach, both by inhibiting acid synthesis and by secreting a protective layer of mucus on the tract. The blanket inhibition of PG synthesis by NSAIDs comes with the potentially life-threatening damage to the GI tract as well as impaired kidney function. The risk to benefit ratio may seem skewed; it is dangerous to inhibit an initial step of a major pathway that leads to PGs of all different varieties and functions. One thing that is important to mention is PGs are made from other pathways as well, not just the cyclo-oxygenase pathway. Namely the lipoxygenase pathway and cytochrome P450 give rise to PGs as well, since there is some redundancy between the three blocking one pathway is not enough to cause complete shutdown of prostagladin synthesis.
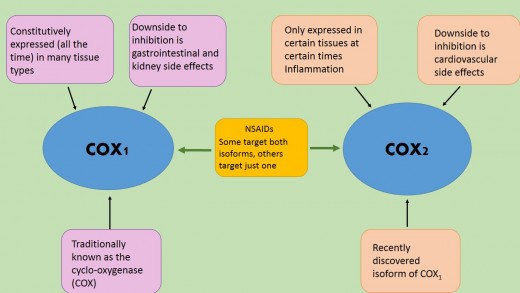
NSAIDS and COX isoforms
All 'newer' NSAIDs evolved from aspirin and function in their analgesic mechanism by inhibiting COX-1 and COX-2 like their predecessor. Historically speaking COX-2, an isoform of COX-1, is somewhat new to this party, confirmed to exist in 1991, and has added several layers to the pain reliever story. Though very similar in structure, several differences between the two enzymes were exploited with the intent of better pain management. These differences are highlighted in the table below. Since the negative side effects from inhibitors of COX-1 are not present in COX-2 specific inhibitors drug researchers believed a selective COX-2 inhibitor, meaning it would inhibit only COX-2 not COX-1, would be a better anti-inflammatory medicine. Several drugs were approved- Celebrex, Bextra, and Vioxx- as selective COX-2 inhibitors. Merck pulled Vioxx off the market in 2004 after it showed serious cardiovascular side effects, specifically stroke and heart attack in users. This prompted the FDA to do a thorough examination of all NSAIDS, both prescription and OTC, selective and non-selective, for similar dangers. Ultimately the FDA asked Pfizer to take Bextra off the market because of the combination of the potential cardiovascular risks and severe skin reactions, unique to this particular drug, as well as the stomach side effects that all NSAIDS have in common. The FDA allowed Celebrex, also a Pfizer drug, to stay on the market with beefed up warnings and precautions to prescribing doctors of the potential risks.

Acetaminophen
Like the other drugs in this article acetaminophen,which often goes by paracetamol in science circles, is both an analgesic and an antipyresis. The pathway for its antipyretic effects is figured out for the most part but its analgesic mechanism of action is not totally nailed down. There are several proposed pathways for acetaminophen including the known pathway for NSAIDs- COX inhibition. Other potential mechanisms include a number of direct or indirect ways, inhibition of Nitric Oxide Synthase (NOS), indirect effects on the endo-cannabinoid pathway, or activation of the serotonin pathway to name a few. As you might expect these pathways all play a role in pain.
What makes locking down the mechanism of action of acetaminophen tricky is direct inhibition of most of these pathways has been ruled out. The alternative- indirect inhibition- could be by any number of ways for each of these separate pathways making it exponentially more difficult to nail the mechanism down. And why is figuring it out so important? Well there is the ‘if it ain’t broke, don’t fix it’ saying which is true but drug discovery is all about improving upon the previous formulation. Improvement could simply be taking a smaller dose of the drug which would further reduce the chances of side-effects. In order to come up with a better version of a drug, scientists need to know the exact mechanism of action in order to set up experiments in the lab to test for new compounds, either similarly structured or totally different, to compare the standard to. Without the mechanism of action, we are stuck with acetaminophen. One has to wonder if the makers of Tylenol aren’t so upset with this predicament. Conspiracy theories anyone?
Several things distinguish Acetaminophen from the NSAIDs class. For one, in the clinical setting acetaminophen has not been consistently proven to cause a reduction in inflammation. Also it does not come with the adverse effect warning of GI complications and kidney problems. Since acetaminophen does not cause these side effects, it seems clear its mechanism of action must be different from NSAIDs'.
Drug Mechanism of Action & Side Effects
Drug
| How it works
| Side Effects
|
|---|---|---|
Aspirin
| direct COX1 & 2 inhibition
| Gastrointestinal and/or Kidney damage
|
NSAIDs
| direct COX1 & 2 inhibition
| Gastrointestinal and/or Kidney damage
|
Acetaminophen
| ???
| When dosed appropriately very little side effects reported
|
Pain itself is meant to be useful, the nervous system takes in harmful stimuli and the signals, like substance P and glutamate, are sent and ultimately changed over to pain. For some things- like putting your hand on a hot stovetop, this pain is useful as it lets us know to remove our hand. Other pain is, in a way, not that helpful, an achy knee from a run or a pounding headache from a room full of screaming toddlers. In many cases removing the stimuli isn’t feasible and thus we want to remove the response-the pain. A similar situation occurs with inflammation, since again it is part of our body’s protection against injury as well as infection. But many times inflammation can be too much of a good thing, arthritis is an auto-immune disorder where inflammation is uncontrollable and is the root of much of the pain experienced in the individual. These over the counter pain relievers all treat pain, and the NSAIDs target inflammation as well.
It is important to take an active role in our health, and many of us take OTC pain relievers from time to time. But these pain relievers illustrate an important point- even what we perceive to be harmless non-prescription drugs can drastically impact our internal health in a negative way. NSAIDs come with the heavy warning of gastrointestinal wear and tear and kidney complications. The fact that aspirin’s full mechanism has not been elucidated is a major reason to use it only when necessary. Adhering to the dosage recommendations is critical and long-term use is not advisable for any of the OTC pain relievers. Seeking out alternative pain relieving methods whenever possible is a great idea, a glass of water to rule out dehydration in the case of a headache, or an ice pack or heat pack in the case of muscle aches and pains. Because even seemingly simple pain relievers involve complex pathways in our bodies, some intentionally targeted by these drugs and some not.








