Understand Surgery: Repairing an Ulnar Collateral Ligament (UCL) Injury
What causes an Ulnar Collateral Ligament (UCL) injury?
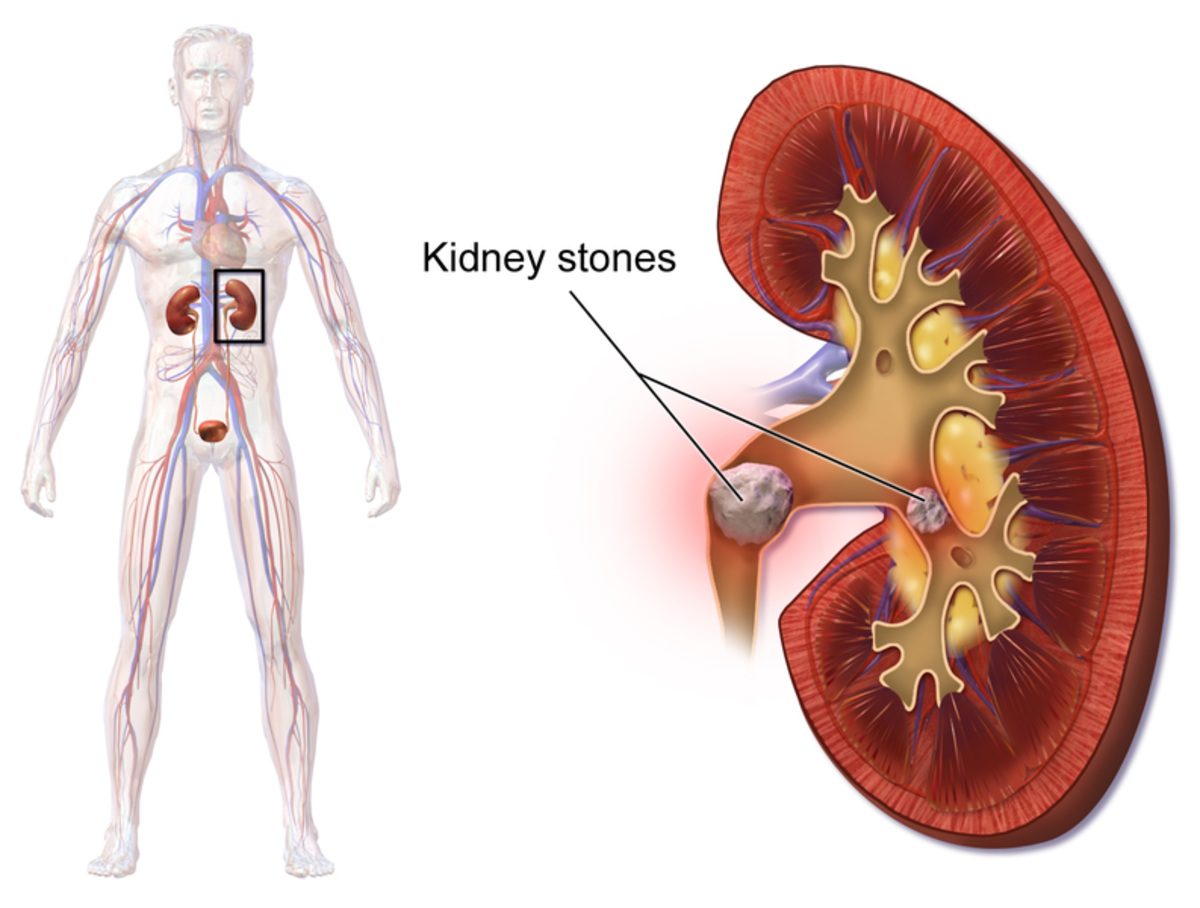
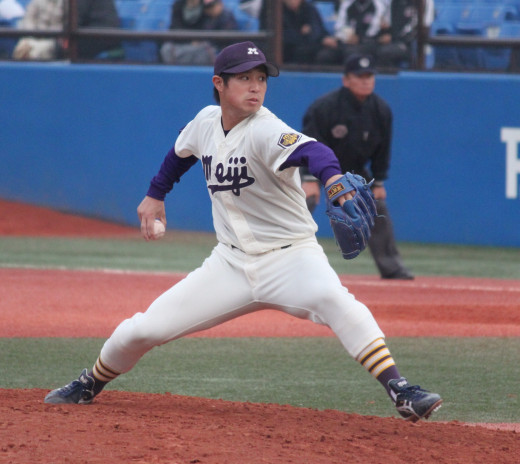
A ligament is a tough, fibrous connective tissue that keeps bones attached to one another. Over time, repetitive overhead motion weakens the Ulnar Collateral Ligament (UCL), which may cause it to rupture. Unfortunately, this means that baseball players, tennis players, volleyball players, and other athletes are some of the most common victims of UCL injuries.
Extreme Valgus- Distorted Elbow

Healthy Ulnar Collateral Ligament
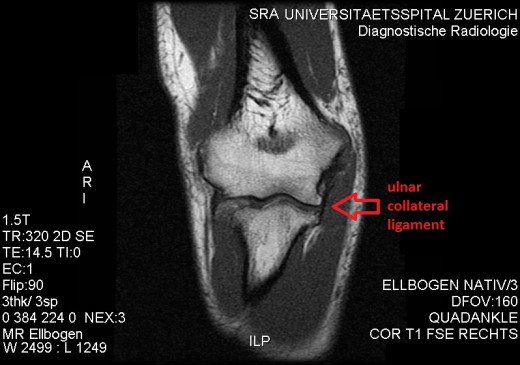
How a UCL Injury is diagnosed.
A UCL injury is typically caused when the abnormal displacement of a part of a limb away from the center of the body (extreme valgus) part is placed on the elbow.
In order to properly diagnose a UCL injury the doctor must first: evaluate the patient's history, conduct a physical exam, and order x-ray imaging. If the patient is nominated for surgical intervention he must undergo an arthrogram. This allows the medical team to measure the amount of damage caused to the ligament by determining whether or not there is a partial or complete tear in the UCL.
If the patient qualifies for surgical intervention his/her elbow is arthroscoped and evaluated for biological debris, spurring, synovitis, and chondral breakdown. A doctor will administer one final stress test over the ligament and once deficiency is confirmed reconstructive surgery can begin.
Acute Vs. Chronic UCL Injury
UCL Injury
| Origin & Symptoms
| Treatment
|
|---|---|---|
Acute
| The patient hears and/or feels a loud "pop" and the ligament fails. Patients may have tingling and/or numbness in their fourth and fifth fingers. The patient is likely to feel excruciating pain on the medial aspect of the elbow.
| Nonoperative treatment includes: rest, ice, anti-inflammatory medication, and physical therapy (typically lasting 3-6 months).
|
Chronic
| The patient's ligament fails over a period of time. An athletic patient may notice a loss of velocity, pitching control, and fatigue.These patients may also feel dysesthesias (abnormal sensation) when they throw an object. Patients with chronic UCL injury may also have mild pain in the posteromedial aspect of the elbow. The majority of pain (if any) is typically felt directly above the UCL when direct pressure is applied.
| Surgical intervention
|
*Platelet Rich Plasma Therapy , at times, can prove to be an excellent alternative to surgery.*
Athletes that commonly throw in an over head motion (such as baseball players, javelin throwers, and tennis players) are the most common victims of UCL
Depiction of UCL Reconstruction
Surgical Procedure Summarized
Once the ligament deficiency is confirmed the surgeon may commence with the procedure. The surgeon makes his initial incision over the medial aspect of the elbow and along the course of the ulnar nerve. The surgeon takes the incision down through the skin and subcutaneous tissue. The muscle is split and the ulnar nerve is protected. The surgeon identifies the anatomical position of the UCL. The surgeon drills into the full length of the ulna using a 4.5-mm drill and then measures the length of the ulnar tunnel. The surgeon obtains a palmaris longus or gracilis graft from the patient by using a suspension technique. A k-wire is drilled across the length ulna to obtain the graft.The surgeon prepares the site by using a 7-mm reamer to drill 15-mm into the ulna. The graft is then placed in the loop of the suspension device. The ligament and suspension device are pulled through the 4.5-mm hole and into the 7-mm hole. While the suspension device passes through the 4.5mm hole it is flipped; this holds the ligament taut onto the cortex of the ulna. Once completed, the ligament is placed into the 7-mm hole via ZipLoop technology. Once the ligament is situated in the hole the surgeon puts tension on the graft; this allows him to properly adjust the graft for the correct anatomical the position of the medial epicondyle. The surgeon begins to close surgical site by drilling a 15-mm hole (using a 7-mm reamer) into the medial epicondyle and two small holes to accommodate the suture. Using an interrupted Ethibond suture, the surgeon brings the main component of the graft through the 7-mm hole and the two limbs with subsequent sutures are pulled into the small holes. The surgeon uses a Hewson suture retriever to tie the two limbs over the bone bridge in the medial epicondyle.
Postoperative Care
After the surgery is completed the patient will be placed in a bulky dressing and a posterior splint. On either the fourth or fifth day the patient returns to the office and is given a light elbow brace locked at 90 degrees, and on day five the patient begins physical therapy. Physical therapy initially includes limited full extension and flexion, but is gradually increased to a wider range of motion over the next four to six weeks.
Once the patient's full range of motion and strength have returned physical therapy culminates into an interval throwing program to strengthen the posterior shoulder, medial elbow, and core.
It is particularly important for athletic patients to pay extra attention to their ipsilateral shoulder.
Prognosis and Complications
Athletic patients are often allowed to return to sports between 6-12 months after their surgery, depending on their position within the sport. Functional results typically range from 85%-90% in comparison to the patient's pre-injury status.
Complications may include ulnar nerve symptoms, a graft that is either too tight or too loose, postoperative infections, and sensory nerve paresthesias.
References
1. Lehman, Richard, MD. "Ulnar Collateral Ligament Reconstruction." The Surgical Technologist. Pages 401-407, September 2013.
2.Kacprowicz, Robert, MD. "http://emedicine.medscape.com/article/97451-treatment"