Understanding the Dynamics of Proving Medical Malpractice Claims

A Plaintiff has the Burden of Proof

The Plaintiff Has The Burden of Proving Medical Malpractice Claims
Medical malpractice claims are filed by plaintiffs asserting that a healthcare professional deviated from the standard of care and caused them harm. Despite the frequency of these claims, many people are unaware of the dynamics involved in resolving them.
In the American legal system, the burden of proof required for medical malpractice claims always remains on the plaintiff. In many cases, a patient may be unaware that a health care professional was acting negligently. Patients at times are unaware of acts of negligence while they are being cared for. At times, a patient may be asleep, unconscious or under anesthesia and may have no knowledge of what is going on around them. As such, proving a case is not always easy.
If you are alleging medical malpractice, you must show that the health care professional breached a duty of care that was owed to you (acted negligently), causing injuries that now entitles you to damages.
Negligence

Negligence
Negligence is defined as failure to do something that a person of ordinary prudence would do in a given situation, or doing something that a person of ordinary prudence would not do in a given situation. The patient asserting that he or she was injured by a health care professional must show that the actor was negligent.
In the case of healthcare professionals, their actions will be compared to the actions of other medical professionals within their particular specialty. Medical professions are expected to stay informed and to keep abreast of advancement in their specialty.
For example, if a brain surgeon acted negligently, his actions or inactions would be compared to the actions or inactions of other brain surgeons and not to the acts of surgeons in general.
Breach of Duty
Duty of Care Owed

Right Leg Amputated instead of R Arm?

Breach of Duty
As a plaintiff in a medical malpractice case, you must establish that the health care professional acted negligently by breaching a duty of care that was owed to you
In order for a breach of duty to exist, there must be some sort of relationship between you and the health care professional. This commonly exists via an agreement such as the general consent that is signed on admission to a hospital.
Simply put, it must be reasonably foreseeable to the professional that if he or she fails to perform a duty owed to you, that harm would occur, making it reasonable to impose liability upon that professional.
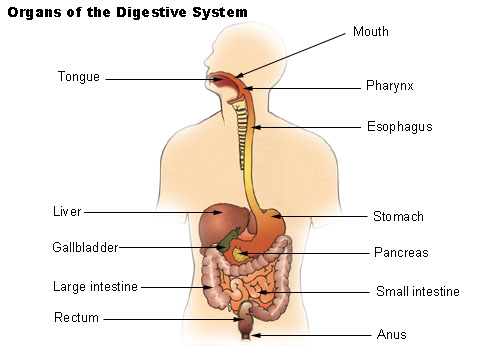
For example, your primary or consulting physician has a duty to properly diagnose a cancerous growth, prescribe the correct antibiotic, properly treat an illness or order the correct test to screen a condition. Your surgeon has a duty to prevent perforation of other organs during surgery. If your physician or surgeon fails to do these acts, or provides care below a certain expected standard, he or she may be accused of breaching the duty of care owed to you.

Medical Malpractice
Have you Ever filed a Medical Malpractice Claim
A Duty of Care May Not Always be Owed
A medical professional may not always owe you a duty of care if he or she was not directly involved in your care.
For example, your surgeon asks another surgeon whom he met at a convention about his opinion on the best approach to repairing a small injury in your reproductive tract. The surgeon with whom you have no patient- surgeon relationship, described a new technique that is allegedly faster and easier to perform that would allow rapid healing without scars.
Your surgeon impressed by this new technique, fails to conduct further research and performs the technique in such a manner that it results in a traumatic gynecologic fistula that leaves you permanently incontinent of bowel and bladder.
Upon suing both surgeons, the jury may disagree that the advising surgeon from the convention owed you a duty of care. The jury may come to a different conclusion if that other physician had evaluated you and was listed as a consulting physician in your care.
Proximate Cause

Proximate Causation
In order to be successful in your claim, you must show that the defendant’s actions or inactions proximately caused your injuries.
Proximate cause is defined as a cause that is legally sufficient to result in liability. It is also defined as the cause that directly produces an event and without which the event would not have occurred. [1]
Plaintiffs are not always able to prove proximate causation in medical malpractice cases. To prove causation, you must show that the defendant specifically engaged in an act or failed to perform an act that were a proximate cause of your specific injuries.
Negligent administration of Penicillin (your allergen) Causing death from Anaphylactic Shock may satisfy the "but for" Causation test
But For Causation

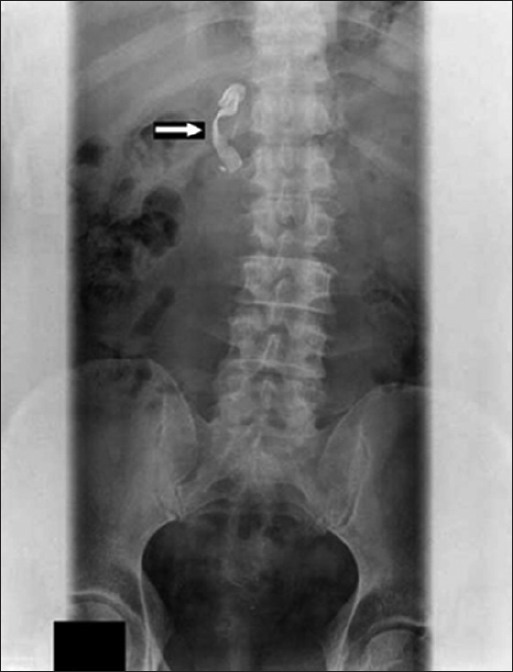
Extracted Tooth found in Stomach

"But For" Causation
The traditional approach or basic test of proximate causation is the “but for” test. The "but for" causation test is appropriate in cases where there is one defendant and no preexisting injuries. The “but for” test is applicable in situations where the particular injury could not have occurred “but for” the negligence.[2] The “but for” causation test may not be appropriately applied in situations where more than one negligent actors bring about a certain injury or where there are pre-existing conditions.
For example, a “but for” proximate causation test may be appropriately used in a case where a nurse forgot to document your loved one's allergies, then administers penicillin to your relative causing an anaphylactic shock that led to death.
A "but for" proximate cause may also be appropriate, where your thoracic surgeon was performing a common chest procedure on you, accidentally used his scapula to rupture your thoracic aorta causing you to hemorrhage severely and die within minutes. The autopsy reveals severe hemorrhage as the cause of death. In this case, it may be easy to argue that “but for” the severed aorta you would not have hemorrhaged and died.
Statistics on Medication Errors
Substantial Factor Test

Substantial Factor Test
Courts such as New Jersey have adopted the substantial factor test to satisfy proximate causation in medical malpractice cases where there are concurrent or pre-existing acts of negligence that lead to injuries. [3]
The substantial factor test requires that you prove that:
(1) a particular deviation from the established standard of care occurred;
(2) that the deviation increase your risk of harm or diminished your chance of survival and;
(3) that such an increased risk was a substantial factor in bringing about the ultimate harm.
The substantial factor standard requires the jury to determine whether a deviation that occurred concurrently with other forces is sufficiently significant in relation to the resulting harm to satisfy the requirement of proximate harm.
Failure to diagnose situations triggering the substantial factor test may arise in cases that include cancer.
For example, if your doctor failed to diagnose your cancer that had already metastasized beyond the point of treatment, the jury could find that the failure to diagnose was not a substantial cause of your injuries.
A jury may come to a different conclusion where a doctor failed to diagnose treatable cancer in its early stages causing it to progress subjecting you to the adverse effects of the disease. Where that cancer then worsens into an advanced stage where it becomes un-treatable the jury may find that the physician's failure was a substantial cause of your injuries.
A court may entertain an argument where a plaintiff shows that she suffered psychologically during the period of cancerous growth, where the physician failed to provide proper treatment and where the delayed treatment caused the cancer to become advanced. [4]
Perforated Colon During Surgery
Issues of Substantial Factor Causation May Not Always be Clear
Where there are multiple actors or preexisting conditions, issues of substantial causation may not always be clear.
For example, after years of procrastination, you finally agreed to take your Gynecologist’s advice and allowed Dr. Ming (surgeon) to perform a hysterectomy. A few days after the procedure at Duke’s Hospital, you develop chills, a temperature of 104F,rapid respirations, internal bleeding, a very low blood pressure, severe abdominal pain, nausea, vomiting diarrhea, decreased urination and a rapid heartbeat. Despite your complaints, Mary your nurse, who was overwhelmed due to staff shortage gave you Tylenol and told you to stop complaining so much. She did not measure your blood pressure which was now 61/23. Your normal blood pressure is within the range of 120/80.
Dr. Smart, your Gynecologist, stopped by the unit, looked at your last documented temperature of 103F and verbally ordered Vancomycin prophylactically as well as blood cultures. He did not physically assess you because he was late for another appointment. Had he assessed you he would have noted that you had a major change in mental status, symptoms of septicemia, that your had a large abdominal swelling with severe pain and guarding, warmth. Had he evaluated you he could have ordered stat testing and repeated vital signs.
Your nurse who was overwhelmed, forgot to write the verbal order for Vancomycin. As such the Vancomycin order was never written, never scanned to the pharmacy and never administered. No abdominal scans were ordered post procedure by your surgeon. Post surgical orders for scans and ultrasounds were the sole responsibility of Dr. Robin who assisted your surgeon. Dr. Robin inadvertently ordered scans on the wrong patient who had a similar procedure that day.
After Dr. Ming departed, you moaned inaudibly for a bed pan, but the Nursing Assistants were all busy. In response to your overwhelming bowel urge, you slowly got out of bed and tried to go to the bathroom without assistance.
After exiting your bed, you became so hypotensive that you passed out, fell and hit your head against a new high powered vacuum cleaner that the hospital housekeeper had forgotten at your bedside. You died instantly. Jose, the housekeeper had forgotten to press the switch that retracted the large sharp blade that was used for scraping calcium deposits from the floor. Jose was never taught how to use the new vacuum cleaner. The Autopsy reveled that you had a perforated colon, seepage of feces in the abdomen, a lacerated skull linked to the blade of the vacuum cleaner and a massive cerebral bleed. The cause of death was traumatic brain injury, cerebral edema, septic shock with multi-organ failure of lungs, liver, myocardium and kidneys. Your husband consults an attorney about filing suit against the Dr. Smart who he disliked intensely for encouraging you to have the hysterectomy that he had opposed.
As your Attorney will explain, there are many defendants in this case apart from Dr. Smart. Due to the chain of events in this case, the substantial factor analysis may be more appropriate than the “but for” analysis in determining whether Dr. Smart’s actions caused the outcome.
A jury could find that Dr. Smart deviated from the standard of care by failing to conduct a proper assessment on you, and that the failure led to an increased risk of your ultimate harm. However, the jury could find that the increased risk was not a substantial factor in your death. A jury could conclude that the failure to measure your blood pressure led to an increase risk of the ultimate harm and may deliberate for days trying to determine if it was a substantial factor in your death.
Despite starting the chain of events that led to your death, Dr. Ming will look towards Dr. Robin who performed the post surgical scan and ultrasound on the wrong patient and may also argue that the vacuum cleaner was an intervening and superseding cause of your death that was not even remotely foreseeable.
Doctrine of Intervening or Superseding Cause

Doctrine of Intervening or Superseding Cause
The doctrine of intervening cause acts to relieve a negligent individual from liability when an independent and new act that was unforeseeable by the actor, produces a result that the defendant or actor could not have reasonably foreseen.
Many jurisdictions resolve questions of superseding cause by focusing on whether the intervening cause is so closely linked (or are normal incidents of the created risk) with the defendant’s negligent conduct that the defendant should not be absolved of responsibility, or whether the resulting injury is so far removed from the Defendant’s negligent conduct that it would be unfair to impose responsibility. [5]
Courts such as New Jersey have provided that Issues of intervening causes are usually left to the jury which would warrant a trial in your case. [6] The basic question is whether the injury was foreseeable.
Are severe hypotension, a lacerated scull and cerebral bleed foreseeable consequences of a negligently perforated hysterectomy? As a plaintiff in the above hypothetical, you may argue that the hypotension was certainly foreseeable. Arguably, a lacerated skull followed by cerebral bleed may be foreseeable consequences of a fall against an improperly stored vacuum cleaner. Jose may still argue that the septicemia that caused your hypotension was the only reason why you passed out and landed on his vacuum cleaner that day.
Foreseeability

Foreseeability
Foreseeability means the quality of being reasonably anticipatable. The courts looks at foreseeability along with actual cause to resolve issues of proximate cause of an injury. The courts have held that an injury need not be foreseeable in the precise way in which it happened, nor does it have to affect any particular person to be foreseeable. [7]
In an ideal world, the staff at Duke’s Hospital would meet to discuss the case and agree amicably on their own proportion of fault. They would then compensate your next of kin accordingly without need for a lawsuit or filed complaint. However, our system of justice does not function in such a manner. As such, despite knowledge of their fault, the defendants will still expected your family to prove that the defendants were at fault. This is why medical experts are usually required to help resolve medical malpractice cases
Expert Witness

Expert Witnesses
Medical malpractice cases usually warrant the involvement of expert witnesses. In many jurisdictions including New Jersey, an expert witness is usually required where damages can be linked to several causative factors. [8]
An expert witness can help evaluate your case or provide expert testimony at trial. An expert witness in a medical malpractice case is usually a medical professional with specialized knowledge in a field who is qualified to act in that role based on knowledge, skill, experience, education or training. Your medical experts will basically identify deviations from or compliance with the established standard of care.
As a plaintiff filing a medical malpractice claim, you are required in many jurisdictions to file an affidavit of merit after the defendant files his or her answer to your complaint. The affidavit of merit is prepared by a medical expert and basically states that there exists a reasonable probability that the professional service outlined in the complaint deviated from the acceptable standards of care.
The medical expert can also explain whether deviations occurred without being a substantial cause of your condition. In the above hypo, an expert may opine on whether a particular test should have been ordered; what early testing could have revealed; and whether early repairs could have prevented the death. A medical exert may opine as to whether the Vancomycin could have altered the process; whether it was appropriate for the particular infection or whether a colon repair was the only solution. A medical expert will help the jury in understanding whether Mary’s failure to measure the blood pressure was a substantial factor in your death.
An expert could also opine on whether your gynecologist was required to perform an assessment during his visit to the unit, what the likely assessment findings would have been and how your condition could have been managed based on his assessment findings.
Your medical expert can testify as to what might have occurred had Dr. Robin ordered the post procedure scans or ultrasound and provided an opinion as to causation.
Damages
As a plaintiff, you must show that you are entitled to damages as a result of the defendant’s negligence.
Medical malpractice damages include awards for medical and hospital expenses, pain, suffering, disability impairment or aggregation of preexisting illness or injury.
In the situation above that involved wrongful death, damages include amounts that are fair and just. They take into account hospital, medical and funeral expenses,loss of future earnings, loss of services, society and companionship. An economist may provide expert evidence on projected earnings.
Jury

Apportionment of Damages
In medical malpractice cases where there are pre-existing conditions or harm caused by several defendants, the issue may also arise as to proper apportionment of damages. In states such as New Jersey, the burden shifts to the defendant physician to show apportionment of damages to other injuries where there are pre-existing or concurrent causative factors. [9] If the defendant cannot provide evidence to support his assertions of apportionment, the jury may hold him or her liable for 100 percent of your damages.
In regular cases of negligence, a plaintiff usually has the burden of proving his or her own damages. As you can appreciate, the complexity of medical malpractice cases warrants this shift in burden of proof.
Most Common Underlying Cause Associated with Negligent Claims (Physicians Insurance Association of America Claim Data Analysis (1985-2000. Courtesy of R. Phill
Underlying Cause Associated with Negligent Claims
| Perentage
|
|---|---|
Diagnosis Error
| 34%
|
Failure to Supervise or Monitor Case
| 16%
|
Imprope Performancer
| 15%
|
Medication Error
| 8%
|
Failure Delay in Referral
| 4%
|
Non Performance
| 4%
|
Performed when Not Indicated or Contraindicated
| 4%
|
No Medical Misdventure
| 4%
|
Delay in Performance
| 3%
|
Failure Delay in Admission to Hospital
| 2%
|
Failure to Recognize Complication of Treatment
| 2%
|
Other
| 4%
|
Statistics on Medical Malpractice Case Resolution (Courtesy of Mark E. Crane-Medscape)
Dismissed
| Settled
| Resolved At Trial
| Decided by Mediation or Arbitration
|
|---|---|---|---|
65%
| 25%
| 5% (Physicians winning 80-90 % of cases
| 4.5%
|
Conclusion
Medical Malpractice cases are often complex. Medical professionals, especially doctors, worked very hard to attain the licenses and to establish their reputations. They will fight equally hard to protect them. Expert fees and depositions may cost tens of thousands of dollars. Before deciding how to proceed with your Medical Malpractice claim please consider the following statistics: Approximately 65% are dismissed by the courts or withdrawn by the plaintiff prior to trial; 25% settle; 4.5% are decided by mediation or arbitration; 5% are resolved before a trial where physicians usually succeed approximately 80-90% of the times. [11]
References
[1] Black’s Law Dictionary (7th ed. 2000)
[2] Verdicchio v. Ricca, 179 N.J. 1 843 A. 2d 1042 (2004)
[3] Scafidi v. Seiler 119 N.J. 93, 574 A.2d 398 (1990)
[4] Evers v. Dollonger, 95 NJ 399, 471 A2d 405 (1984)
[5] Lynch v. Scheininger, 162 N.J. 209, 227 (2000).
[6] State v. Pelham, 801 A.2d 488 N.J (App. Div. 2002)
[7] Hill v, Yankin, 75 N.J. 139, 143, 380 A2d. 1107 (1977)
[8] Schwarze v. Mulrooney, 291 N.J Super, 530, 541 (App. Div. 1996)
[9] Fosgate v. Corona, 66 N.J. 268, 330 A.2d 355 (1974)
[10] Phillips RL, Jr, Bartholomew LA, Dovey SM, et. al. Learning from Malpractice Claims about Negligent, adverse Events in Primary Care in the United States. Qual Saf Health Care 2004: 13:121-6. [PMC Free Article] [Pub Med]
[11]Crane, Mark E. Guide to Winning Your Malpractice Law suit. Medscape Pulse: Availabe at: http://www.medscape.com/features/slideshow/malpractice
Other Resources
Breach of Duty. Medical MalpracticeHelp.com. Available at: http://www.medicalmalpracticehelp.com/legal/breach-of-duty
Berg. David. Medical Malpractice. Available at: http://www.medicalmalpractice.com/resources/the-burden-of-proof-medical-malpractice-lawsuits.html
Traumatic Aortic Rupture. Available at: http://en.wikipedia.org/wiki/Traumatic_aortic_rupture