Can You Breast Feed With Implants?

If you’ve ever asked the question ‘Can you breast feed with implants?’ then you may have been told the following; as breast implant surgery does not usually involve repositioning the nipple or cutting the milk ducts, it is entirely possible to breast feed. This is great news for the estimated one million women each year who undergo breast augmentation and may later want to breast feed. But is this the whole truth?

Can you breast feed with implants?
Researchers Schiff and colleagues set about to answer this question with a systematic review of the evidence-base. Their paper, published in 2014, investigated breast feeding in women who’d had implant surgery, comparing their experiences to those of women with natural breasts. In undertaking the review, Schiff meticulously combed through thousands of studies. Only three studies were deemed as appropriate to answer the research question about the impact of cosmetic implants on breast feeding.
The first paper reviewed was a 1996 study by Hurst and colleagues which recruited participants from a hospital in Texas. The study investigated breast feeding in 42 women with breast implants, as well as 42 women without implants. Of the 42 women with implants, 27 (64%) had insufficient breast milk for exclusive breast feeding. Of the women without implants, only 3 out of 42 (less than 7%) had insufficient breast milk. The study suggested that women who have had breast enlargement surgery are much more likely to struggle with poor breast milk supply than women whose breasts are au naturel.
It should be noted that the participants in Hurst’s study were chosen from a group of women who had all been referred to the Texan hospital’s lactation program for support. It is likely that many of the study population were experiencing breast feeding problems, regardless of whether or not they had implants. Furthermore, the participants were all mothers whose infants were hospitalised, many due to being born prematurely with low birth weight. Having the study participants recruited from such a group raises questions on how applicable the study’s conclusions would be across the general population.
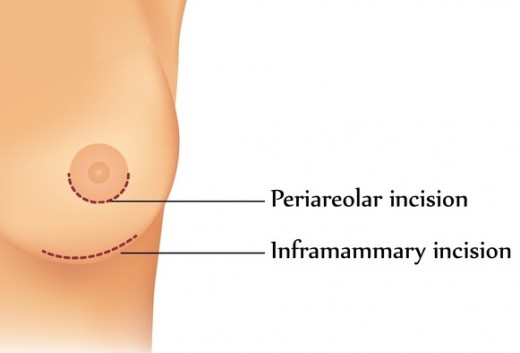
Amongst the study’s investigations, Hurst explored whether the different types of surgical incision had an effect on breast-milk supply. Of the two types of incision; submammary (underneath the breast) and periareloa (around the nipple); a periareloa incision was more strongly linked to producing insufficient breast milk. However, when researchers Cruz and Korchin investigated the same thing in 2010 they found that the surgical approach used had little effect on breast feeding outcomes.
The next paper mentioned in Schiff’s review was a study carried out in Brazil in 2010. Researchers Andrade and colleagues investigated breast feeding in 24 women with implants, as well as 24 women with natural breasts. The study found that one month after giving birth, the probability of a mother exclusively breast feeding her infant was 54% in the group of mothers with breast implants. In the group of mothers with natural breasts, the probability of them exclusively breast feeding was far more; 80%. Again, the research suggested that women with breast implants are more likely to suffer problems with inadequate breast milk supply.
Confounding variables
The problem with researching breast feeding after implant surgery is that the evidence-base is formed only from cohort studies. That is, observational studies of women who have or haven’t had breast surgery, as they go about living their lives. With cohort studies it’s almost impossible to eliminate all the confounding variables.
Potential confounders identified by Schiff include maternal age, strength of the mother’s intention to breast feed, mothers’ breast feeding expectations, gestational age of the baby at birth, number of times the mother had undergone breast surgery, breast hypoplasia, material used in the implants, type of incision used for placing the implants, health of the mother, health of the baby, and whether breast milk was given directly from the breast or expressed. Schiff could not have eliminated all of these confounders from the systematic review. For a start, the three studies reviewed did not all disclose values such as mother’s age or number of times the mother had undergone breast surgery. Secondly, had Schiff and colleagues discounted these three studies because they were less than happy with the population descriptions, there would be no studies left to review.
One confounder that is intrinsic to this field of research is the issue of breast hypoplasia. Breast hypoplasia is the medical name given to the condition of having small breasts and insufficient breast tissue. Having hypoplastic breasts can significantly reduce a mother’s breast milk supply. And whilst there are no statistics to confirm the matter, it could be argued that women with small hypoplastic breasts are much more likely to undergo breast implant surgery than women with larger breasts.

I am a huge fan of the saying correlation does not mean causation. Indeed, I love to trot out this favourite expression at every appropriate opportunity; this being one of them. Yes, research shows a correlation between women having breast implants and women struggling with breast milk supply. But this doesn’t mean that it was breast implant surgery that caused the reduced milk supply. Maybe the population of women who tend to have breast implants are the same population of women who tend to struggle with inadequate breast milk supply anyway. Schiff noted this and stated that given the current evidence, hypoplastic breasts cannot be ruled out as being the main cause for poor breast milk supply after implant surgery.
Having said all of that, there was one study reviewed, by Cruz and Korchin in 2010, that rather cleverly managed to eliminate the confounder of hypoplastic breasts. This study recruited 212 women known to a cosmetic surgery clinic. Approximately half of the women (105 of them to be precise) had undergone breast surgery to have saline implants. The other half, the control cohort, (107 women) did not have breast implants. But what made the study particularly interesting is that all of the women without implants, wanted implants. They were all awaiting evaluation by the breast surgeon with the plan to undergo breast implant surgery soon. By using a study population selected only from the type of women who tend to have breast implants, Cruz and Korchin were able to eliminate hypoplastic breasts, or indeed any other pre-surgical condition or tendency that exists in women wanting implants, as a confounding variable.
In Cruz and Korchin's study, the group of women who were awaiting breast implants were asked about their previous experiences breast feeding. These were then compared to the experiences of the woman who had breast implants and later went on to breast feed. In the group of women with implants, 63% reported successful breast-feeding. In the group of women without implants, far more; 88%, reported successful breast-feeding. Even with the confounder of hypoplastic breasts eliminated, Cruz and Korchin’s results suggested the same as the other two studies; women with breast implants may struggle to exclusively breast feed their infants.

Schiff and colleagues pooled the results of all three studies in order to put a figure to the alleged milk-stifling effect of breast implants. They concluded that breast implant surgery may reduce a woman’s likelihood of being able to exclusively breast feed by about 40%.
So, what’s stopping the breast milk?
Schiff gave various suggestions as to why women might struggle to breast feed after implant surgery. These were:
- The milk ducts, glandular tissue and nerve supply around the breast may have been damaged during the implant surgery.
- Whilst in position, the implant may place pressure on the breast tissue and block some of the milk ducts.
- The implant surgery may have lead to post-surgical complications such as infection or haematoma (a pool of blood occurring within the body).
- As part of the body’s immune response, collagen fibres form a capsule around the implant. If the collagen fibres contract, the breast and the breast implant will be squeezed under pressure. This is called ‘capsular contracture’.
- Breast feeding may be painful after breast implant surgery.
- Women’s attitudes towards breast feeding may be different after they have had breast implant surgery.
Women’s attitudes and breast feeding
You might wonder how the last listed point could possibly affect breast feeding. After all, ‘women’s attitudes’ is not a physical, anatomical or tangible factor. But let’s consider an example: two breast feeding mothers, Beverley and Alicia, are both struggling to produce enough breast milk. Beverley has breast implants following augmentation surgery three years ago, whilst Alicia has natural breasts.
Beverley
Beverley puts her breast feeding struggles down to the fact she has breast implants. She remembers that, at antenatal group, one of the women shared a story about a friend who’d had a ‘boob job’ and so could only bottle feed. Beverley always intended to breast feed but now she doesn’t feel she has a choice; it’s not like she can rewind time and not have the implant surgery! Beverley speaks to her midwife for advice and then switches over to formula feeding.

Alicia
When Alicia struggles with breast feeding, she doesn’t immediately rationalise her struggles with a reason. She thinks back to her antenatal group and remembers a talk on breast feeding which explained that many women find it challenging. Alicia contacts two different support groups for advice, as well as talking things through with her midwife. She perseveres with breast feeding and, after a while, her body catches up with the demands of her hungry baby.

So, what actually happened?
Beverley’s struggle to breast feed may not be because of her breast implants. As for that ‘boob job’ mentioned at antenatal group; that could have been reconstruction surgery following a double mastectomy for all Beverley knows! But when she contacts her midwife, her mind is already set towards formula feeding. Guided by what Beverley wants, her midwife supports her with the switch.
Alicia is more open minded about her struggles as she doesn’t have anything as concrete as previous breast surgery to ‘explain’ or rationalise her poor milk supply. When she talks to support groups and her midwife she asks them for breastfeeding tips and advice. She is given support to persevere.
The story of Beverley and Alicia is just a made up example. But it clearly illustrates how different attitudes might affect outcomes, even if breast implants themselves aren’t physically to blame for breast feeding problems.
What’s the big deal?
Schiff’s systematic review of research suggested that having breast implant surgery may well affect a woman’s ability to exclusively breast feed. Schiff and colleagues did not attempt to explain why this effect occurs, and at present this remains a mystery. They did, however, put a figure on the milk stifling effect, suggesting that having breast implants reduces the likelihood of a woman being able to exclusively breast feed by about 40%. This conclusion was offered with caution however, as the studies analysed within the review had modestly sized study cohorts with questionable representativeness, as well as multiple confounding variables.
Amongst Schiff’s findings was the revelation that there has been very little research done about how breast augmentation affects breast feeding. This is both surprising and alarming given the fact that an estimated one million women each year choose to undergo the procedure. Schiff proposed that the lack of relevant studies is because, at the time of opting for surgery, women are not massively concerned about future breast feeding.
It could even be argued that at the time of investigating cosmetic surgery options, any questions that women do have about breast feeding with implants are answered with one token response: breast feeding is entirely possible as long as your surgery didn’t damage the nipple, nerves or milk ducts. After all, this is the response that you get if you do a quick online search. But as Schiff’s review points out, it’s a response that doesn’t tell the full story.
Clearly, much more research needs to be done to clarify the existence of, and the extent of, any milk stifling effect of breast implants. This research needs to consist of large scale studies involving cohorts that are representative of a wider population. The studies must also be designed in a way that eliminates confounding variables such as breast hypoplasia and women’s attitudes to breast feeding. Only with many more valid and reliable studies in the evidence-base can women truly make an informed decision about breast implant surgery when they later wish to breast feed.
___________________________________________________________________
References
Andrade RA, Coca KP, Abrão ACFV (2010) 'Breast feeding pattern in the first month of life in women submitted to breast reduction and augmentation.' Jornal de Pediatria. 86 (3), pp. 239-244. [Online] DOI: 10.2223/JPED.2002 (Last accessed 04th August 2017).
Cruz NI and Korchin L (2010) 'Breast feeding after augmentation mammoplasty with saline implants.' Annals of Plastic Surgery. 64 (5), pp. 530-533. [Online] DOI: 10.1097/SAP.0b013e3181c925e4 (Last accessed 04th August 2017).
Hurst NM (1996) 'Lactation after augmentation mammoplasty.' Obstetrics & Gynecology. 87 (1), pp. 30-34. [Online] DOI: 10.1016/0029-7844(95)00349-5 (Last accessed 04th August 2017).
Schiff M, Algert CS, Ampt A, Sywak MS and Roberts CL (2014) 'The impact of cosmetic breast implants on breast feeding: A systematic review and meta-analysis.' International Breastfeeding Journal. 9 (17). [Online] DOI: 10.1186/1746-4358-9-17 (Last accessed 04th August 2017).