Acute Pancreatitis - Causes, Risks, Treatments, and Prevention
What Is Pancreatitis?
Pancreatitis means "inflammation of the pancreas".
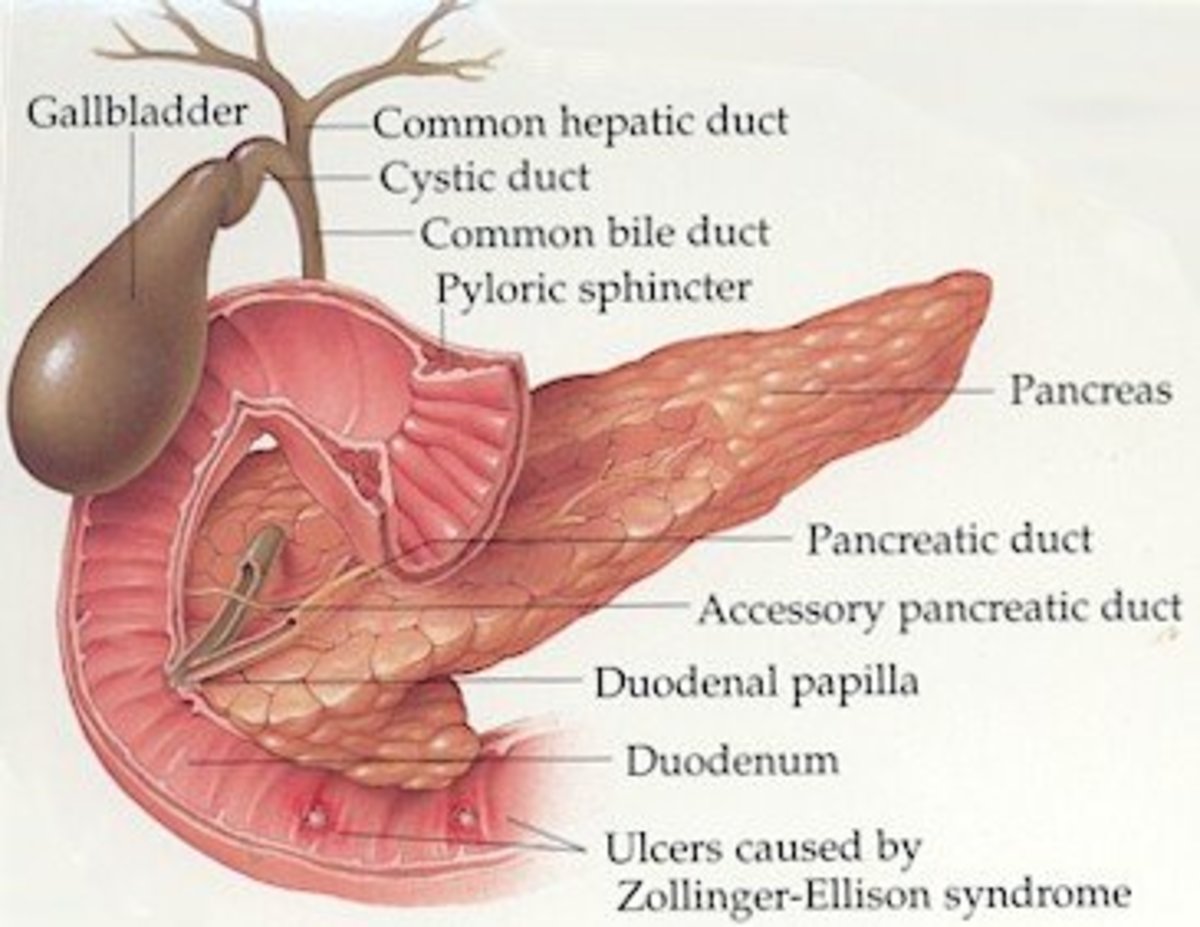
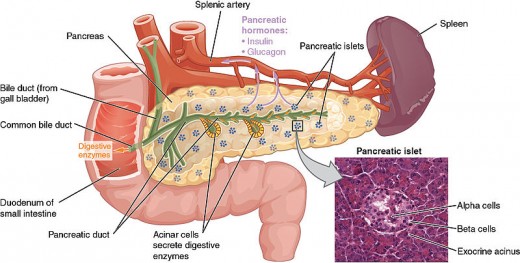
The pancreas is located in the upper abdomen, and is found behind the stomach. It plays a large role in aiding digestion as the pancreas gland produces two types of substances - digestive juices, and digestive hormones
The digestive juices include enzymes and bicarbonate which help break down the proteins and fats from the foods you have eaten. They do this in your small intestine, or duodenum. The digestive hormones are mainly insulin and glucagon which help to control your blood sugars (blood glucose) a major source of energy and play a role in the causes of diabetes.
Inflammation of the pancreas can have numerous causes - including blockage of the duct by a gallstone, surgery, or no discernable cause. Once the pancreas becomes inflamed, it can cause swelling of the pancreas, the surrounding blood vessels, and cause bleeding, damage to the gland, and infection. If the juices from the pancreas become 'trapped' by the swelling - they may start to digest the pancreas. If this occurs, it may not be able to carry out it's normal functions.
The Pancreas
Types of Pancreatitis
Pancreastitis can be "acute" or "chronic"
Acute Pancreatitis:
- Acute pancreatitis begins soon after the damage to the pancreas occurs.
- Many attacks are mild, but approximately 20% can be severe - even life threatening.
- Most will resolve completely and the pancreas will return to it's normal functioning state.
- Most people who have an acute attack will generally only suffer the one attack.
- Acute attack can be mild or severe - severe attacks can be life-threatening.
Chronic Pancreatitis:
- This often begins as acute pancreatitis, but the damage to the pancreas may cause scarring.
- This means that the pancreas cannot return to it's normal state.
- The damage may gradually worsen over time.
Symptoms of Pancreatitis
Signs and symptoms of pancreatitis can vary slightly depending on which type of pancreatitis is experienced.
Common signs and symptoms are:
- Severe upper abdominal pain - often Left Upper Quadrant
- Pain radiating from abdomen into back
- Abdominal pain that feels worse after eating
- Nausea and/or vomiting
- Tender abdomen (on touching)
Chronic pancreatitis symptoms also include:
- Oily, smelly stools - also known as steatorrhea
- Losing weight without trying
Other symptoms may include:
- Fever
- Tachycardia (fast heart rate); hypotension (Low Blood Pressure)
- Abdominal distention (65%)
- Bowel sounds that are diminished or absent entirely - meaning the bowel is not working
- Jaundice (yellowing of the skin due to build up of bilirubin in the skin)
- Dyspnea (breathlessness); tachypnea (fast breathing)
- In severe cases, hemodynamic instability (blood unstable) and hematemesis (vomiting blood) or melena (blood in stools)
- Pale, sweaty, and listless appearance
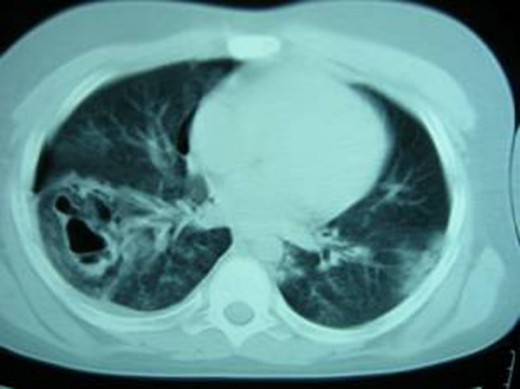
CT Image of Acute Exudative Pancreatitis

Diagnosis of Pancreatitis
Blood tests are usually ordered, as this can show up certain abnormalities in the blood caused through pancreatitis. Blood tests during acute pancreatitis will show very high levels of amylase and lipase - enzymes usually formed by the pancrease. Levels of glucose, calcium, magnesium, sodium, potassium and bicarbonate may also be affected.
An abdominal ultrasound may also be requested - this bounces sound waves off of the internal organs, and send information back to the handheld scanning device - this produces a picture that will also show the location of any gallstones.
Another test that may be ordered is a CT or computerised tomography scan. This scan is a non-invasive way to produce three-dimensional images of parts of the body. This can show gallstones, and any damage to the pancreas, as well as identify pockets of fluid.
An Endoscopic Ultrasound is an ultrasound done via endoscopy - or a tube camera down the patient's throat - this particular ultrasound can image the pancreatic and bile ducts.
A Magnetic Resonance Cholangiopancreatography (MRCP) uses magnetic resonance imaging to create cross section images of the body. Using a dye, this type of test can show the gallbadder, pancreas, pancreatic ducts, and bile ducts.
An example of the results that can signal the difference between Mild Acute, and Severe Acute Pancreatitis are as follows from Medscape (Bullets are added by me)
"Evidence of organ failure
- systolic blood pressure below 90 mm Hg,
- arterial partial pressure of oxygen [Pa O2] 60 mm Hg or lower
- serum creatinine level 2 mg/dL or higher,
- GI bleeding amounting to 500 mL or more in 24 hours)
Local complications
- necrosis
- abscess
- pseudocyst"
Pseudocyst
Pancreatitis
Have you had, or know someone who has had pancreatitis?
Causes of Pancreatitis
Pancreatitis may have a known cause, including
- Alcoholism
- Gallstones
- Some metabolic disorders
- Cystic Fibrosis
- Post-ERCP - a treatment to destroy gallstones
- Abdominal trauma
- Penetrating ulcers
- Cancer of the head of the pancreas
- Certain medications
- Infections such as Mumps, Coxsackie Virus
- Abnormalities in the shape of the pancreas
- Autoimmune pancreatitis - the body fighting against the pancreas
Occasionally, there is no cause that can be found.
The most common cause of Acute Pancreatitis is a gallstone blocking the duct, and the most common cause of Chronic Pancreatitis is alcohol - usually heavy usage.
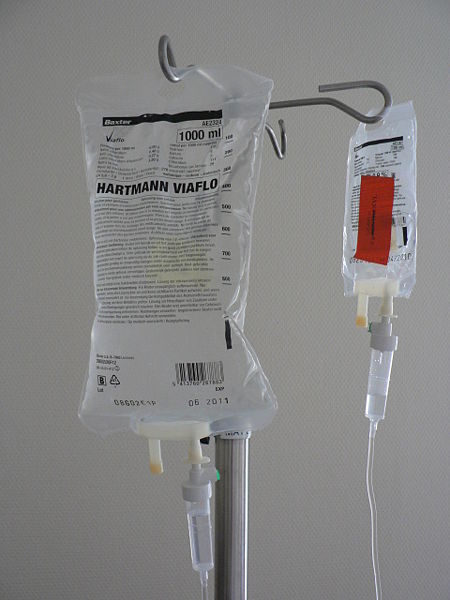
IV Fluids
Treatment for Pancreatitis
For most Acute Pancreatitis - the treatment involves Intravenous (IV) pain relief and fluids in a hospital, until the pancreas settles and resumes normal functioning. The cause of the pancreatitis attack will need to be resolved - eg cholecystectomy (gallbladder removal) or ERCP if the initial attack was caused by gallstones, giving up smoking cigarettes and drinking as both of these can cause pancreatitis.
However, approximately 25% of people with acute pancreatitis have Severe Acute Pancreatitis and may need admission to Intensive Care or High Dependancy Unit (ICU or HDU) as pancreatitis can affect the heart, lungs and kidneys. In some cases, the tissue of the pancreas may be damaged and become infected. This can be difficult to treat, and will occasionally require heavy duty antibiotics. Psuedocysts are also difficult to treat, and may involve surgery.
Antibiotics are not usually recommended as prophylaxis except when there is infected pancreatic necrosis present, but not solely for fever.
Surgical Intervention

Surgical Intervention
Occasionally, surgical intervention is necessary to treat the pancreatitis, or more commonly the cause of the pancreatitis.
Surgical interventions include but are not limited to:
- Cholecystectomy - removal of the gall bladder
- Placements of stents in the pancreatic duct
- Distal Pancreatectomy - removal of part of the pancreas
- Drainage of infected pancreatic abcesses
- Removal/Drainage of pseudocysts
- Removal of infected pancreatic necrosis
Whilst surgery may seem like the 'easiest' way to fix the problem, often this is not the case. For mild acute pancreatitis, surgery is not usually necessary. For Severe Acute Pancreatitis, they will try to treat the symptoms as they arise, and only opt for surgery when there is no other choice.
For example:
A family member with Severe Acute Pancreatitis was hospitalised for several weeks, before an attempt to drain psuedocysts formed in his abdomen was made. This was completed by the 'transgastric' route - endoscopically through the stomach, so no external excision was made. A drainage naso-gastric tube was placed, to drain the infection.
A second surgery a number of weeks later was performed to remove the psuedocysts that had not shrunk despite very strong antibiotics. This surgery was much bigger - involving an incision across his abdomen, and ICU care post op.
Prevention of Pancreatitis
To prevent pancreatitis, it is necessary to try to prevent the illnesses and conditions that can contribute to pancreatitis such as gallstones, heavy alcohol usage and smoking.
To prevent gallstones, it is a good idea to maintain a health weight, and healthy diet - such as a low fat diet with plenty of fruit and vegetables, Whole grains are also recommended as these are good for your cholesterol level, which may contribute to gallstones.
It is not necessary to completely avoid alcohol to prevent pancreatitis, but it is recommended to avoid heavy or binge drinking of alcohol. Moderate consumption of 2 (1 for women and older people) alcoholic beverages or less per day is okay. However if you have had pancreatitis, it is best to avoid alcohol completely to avoid further attacks.
Cigarette smoking has also be considered to play a role in the development of pancreatitis, so avoiding cigarette smoking, or giving up the habit, is recommended - particularly to those who have had pancreatitis.
Acute Pancreatitis
Conclusion
Acute Pancreatitis is an inflammation of a pancreas that causes upper abdominal pain, nausea and vomiting. Often caused by gallstones. it is most often a mild illness, but requires hospital intervention with fluid and pain relief until the attack subsides and the pancreas function returns to normal. However, some people may have Severe Acute Pancreatitis, which can be life-threatening as it affects the function of a number of vital organs. Severe Acute Pancreatitis requires HDU or ICU level care.
Treatments include IV fluids, pain relief, avoiding alcohol and cigarettes, and occasionally surgical intervention is required.
To prevent a repeat or initial attack it is wise to maintain a healthy diet and healthy weight, avoid (or moderate) alcohol consumption, and give up or avoid cigarettes.
Information From:
Information for this hub was collated from personal knowledge, personal experience, and these informational websites:
WebMD - What Is Pancreatitis?
Emedicine - Pancreatitis
MayoClinic - Pancreatitis
Medscape - Acute Pancreatitis
National Institute for Diabetes and Digestive and Kidney Diseases - Pancreatitis