Acute Rheumatic Fever: The Health Relevance Of Its Differential Diagnosis, Treatment And Prophylaxis
Differentiating Rheumatic Fever From Other Diseases
Differential Diagnosis
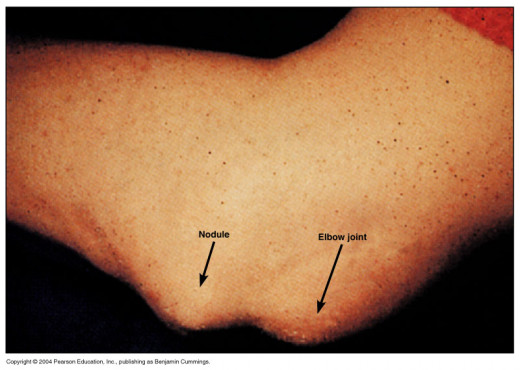
Infective endocarditis may present with fever and heart lesions. Presence of clubbing, hepatosplenomegaly, absence of arthritis and development of embolic complications help to distinguish this condition. Henoch- Schonlein purpura may resemble rheumatic fever when purpura is insignificant. Acute leukemia may present with arthralgia and arthritis and produce difficulty in diagnosis before the blood picture becomes diagnostic. Presence of severe pallor, bleeding tendencies, non-migratory arthritis, hepatosplenomegaly and fundal hemorrhages should alert the physician about the possibility of leukemia. Spetic arthritis is usually monoarticular and the source of primary infection may be evident. Gonococcal arthritis, Reiter’s syndrome, systemic lupus erythematosus, polyarteritis nodosa, allergic arthritis and serum sickness have to be excluded in atypical cases.
Treating Rheumatic Fever

Treatment
Treatment may be divided into: management of the acute state; eradication of the streptococcal infection and prevention of recurrences (secondary prevention).
Acute Phase: Strict bed rest should be instituted since it is absolutely essential to limit carditis and reduce the incidence of chronic heart disease. It is to be continued till ESR comes down to normal.
Anti- inflammatory agents: The drug of choice is aspirin which has a dramatic effect. The antirheumatic dose of aspirin is 90 to 100 mg/Kg/day, given in four divided doses after food. Since in this high dose the drug may produce gastric irritation, antacids such as aluminium hydroxide or magnesium trisilicate may be given simultaneously. The dose of aspirin is reduced when fever subsides and it should be continued in a small dose for 10 days after disappearance of all the symptoms. Adverse side effects of aspirin include nausea, dizziness, tinnitus, deafness, vomiting, hyperventilation, hemorrhagic tendency and psychosis.
Alternatively, corticosteroids may be given. Corticosteroids and salicylates are equally effective in the management of rheumatic fever. Corticosteroids are preferable in those with carditis, since it controls the cardiac lesion, whereas aspirin may not. The common preparation is prednisolone in a dose of 40 to 50 mg daily given orally. Withdrawal of steroids may result in exacerbation and hence it should be tapered off under the cover of aspirin.
Streptococcal infection is controlled by giving procaine peniciliin intramuscularly in a dose of 500,000/day for 7 to 10 days.
Treatment of chorea: Salicylates and steroids have no effect on chorea. The patient is put to bed in a quiet room. Involuntary movements can be controlled by diazepam, chlorpromazine, or phenobarbitone, given in the usual doses, Haloperidol is very effective in controlling the chorea if given in a dose of 0.25 mg 6 hourly.
Prophylaxis Of Rheumatic Fever

Secondary Prophylaxis
Since rheumatic recurrence is invariably precipitated by streptococcal reinfection, benzathine penicillin 1.2 mega units is given once every three weeks to prevent streptococcal re-infection and rheumatic recurrence. As an alternative, oral penicillin, 200,000 units twice dails may be given. Penicillin- sensitive individuals may be treated with sulphadimidine 0.5 g/day. It is desirable to continue rheumatic prophylaxis, life long but the chance of recurrence comes down with increasing age and the passage of time after the acute attack. It is mandatory to continue penicillin prophylaxis at least till the age of 25 years or for 5 years after the initial attack. Whichever is later.
Primary prevention has been achieved very effectively in most of the developed countries by early diagnosis and prompt treatment of streptococcal infections.
© 2014 Funom Theophilus Makama