African Trypanosomiasis: Clinical Presentations, Diagnosis, Treatment And Prevention
Clinical Presentation Of African Trypanosomiasis

Clinical Manifestations Of Sleeping Sickness
The incubation period varies from one to three weeks. Though, the symptoms of T. gambiense and T. rhodesiense infection are broadly similar, the Rhodesian type is usually more severe and runs a more acute course with a higher mortality.
The initial lesion is the formation of a nodule at the site of the bite (trypanosomal chancre). Trypanosomes are seen in this lesion. Irregular fever and parasitemia occur within 1 to 2 weeks. Cervical femoral and axillary groups of lymph nodes enlarge. Lymph nodes are more pronounced in the posterior triangle of the neck in T. gambiense infection. Enlargement of these groups of lymph nodes is called “Winterbottom’s signs”. The spleen is often enlarged. Anemia develops in due course due to slow inanition and hemolysis. Fever, lymphadenitis, anemia and debility continue for several months. The CNS involvement is late in the Gambian type while symptoms of the CNS involvement develop within a few months in the Rhodesian type. The whole course runs over 2 to 3 years, but the course is shorter in the Rhodesian type and death may occur in 6 to 9 months.
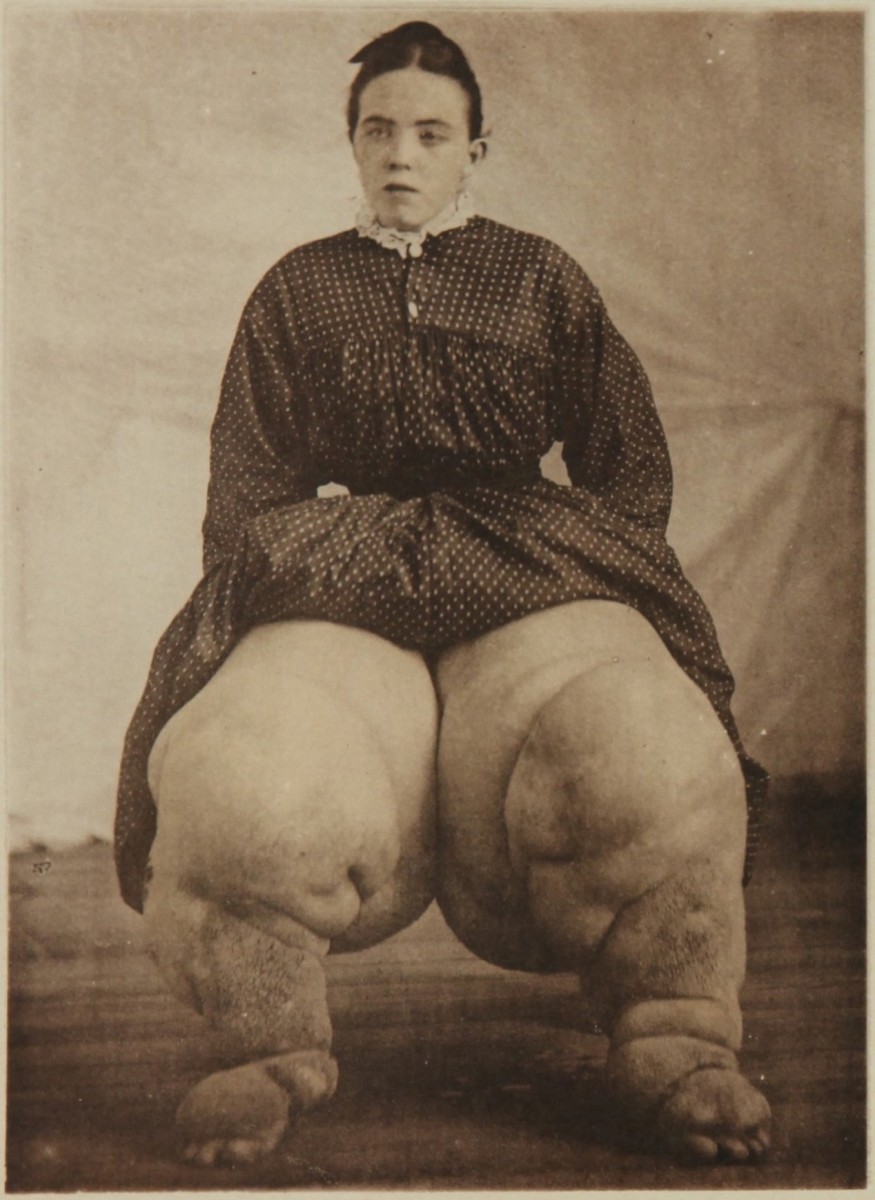
Several unusual manifestations may develop. These include circinate erythematous skin rashes, localized edema over the face, eyelids and neck, tibial tenderness (Kerandel’s sign) neuralgic pains, formication, myocarditis, pericardial effusion and jaundice. The sleeping sickness stage sets in when the parasites enter the CNS. The debility and languor increase, the gait becomes slow, shuffling and swaying, the speech becomes slurred and tremors of the tongue and lips develop. The patient may become demented. Mask-like vacant expressions, drooping of eyelids, tendency to fall asleep during day time and restlessness at night are all seen in endemic areas. The patient becomes severely emaciated and serious complications like Pneumonia, dysentery, hyperpyrexia, convulsions and coma may supervene and prove fatal. Though untreated cases of sleeping sickness and generally fatal, the Gambian type may recover spontaneously at times.
How To Diagnose Sleeping Sickness

Infectious Diseases
Diagnosis & Treatment Of Sleeping Sickness
Diagnosis Of Sleeping Sickness
History of residence in an endemic area, irregular fever, enlargement of cervical lymph nodes and hepatosplenomegaly should point to this diagnosis. Trypanosomes can be demonstrated in peripheral blood, lymph gland aspirate or the CSF. When the parasites are scanty concentration methods using centrifugation are more helpful. The CSF findings give evidence of neurological involvement. Serological tests like the indirect fluorescent antibody test and the enzyme linked immune-sorbent assay (ELISA) are helpful in diagnosis.
Treatment
The early cases: Suramin, which is a derivative of urea, is effective when the infection is limited to the blood and lymph nodes. Suramin treatment is indicated in cases which do not show neurological involvement and CSF abnormalities. The course consists of 5 doses of suramin 20 mg/Kg given intravenously as a 10% solution on days 1, 3, 7, 14 and 21. Toxic effects include sudden fatal anaphylactic reactions and renal tubular damage manifesting as proteinuria. When proteinuria occurs, the drug should be temporarily stopped. Since suramin does not enter the central nervous system, it is ineffective in the late cases.
Late Cases: Neurological involvement is treated with melarsoprol (Mel B). It is a trivalent arsenical condensed with BAL. Melarsoprol glycol. It is given intravenously at a slow rate in a dose of 3.6 mg/Kg limited to a maximum of 200 mg (3.5 to 5ml) given on alternate days. In severe cases, the course may have to be repeated after 3 weeks. Melarsoprol is very effective in curing even advanced T. rhodensiense infections. Untoward side effects include local necrosis, anaphylactic reactions and encephalopathy.
A water soluble derivative of Mel B (Trimelarsan [Mel W] Melarsonyl) can be given intramuscularly or subcutaneously and it is useful to treat children.
Effect of treatment: Nearly all clinical signs and CSF abnormalities return to normal with early treatment and remain so even after two years. Even advanced cases are curable by modern therapy. The patients should be observed for two years with repeated CSF examination to detect relapse early.
Prevention: It is achieved by anti-tsetse measures such as the use of a tsetse repellant cream (Di-Meepol), avoidance of reservoir hosts and chemoprophylaxis. A single dose of suramin (25 mg?Kg) or of pentamidine (4 mg/Kg) gives protection for up to 6 months.
© 2014 Funom Theophilus Makama