Amoebiasis: Extra-intestinal Lesions, Diagnosis And Its Correlation With Meningoencephalitis
How To Diagnose Amoebic Liver abscess

Extra-Intestinal Lesions Of Amoebiasis
Amoebic Liver abscess: Invasive amoebae reach the liver through the portal blood stream from the colon which is the primary seat of infection. In the liver, they multiply and cause colliquative necrosis of liver cells to produce abscess. Unlike pyogenic abscess, the wall of the amoebic abscess is made up of necrotic and compressed liver tissue and it is devoid of granulation tissue. Active amoebae are found near the expanding margins. The pus is made up of necrotic tissue which shows amorphous material and erythrocytes. It is sterile on culture. In most cases, the color of the pus is reddish brown (anchovy sauce-like). Amoebae are seen only rarely in the pus aspirated from the center of the abscess, they are more often demonstrable in the pus aspirated from near the walls on subsequent occasions. The site of the abscess is usually the right lobe. It is usually single and may attain very large size. The abscess may enlarge progressively and spread by contiguity to the chest wall, colon, diaphragm, pleura and pericardial cavities. Amoebic abscess does not impair hepatic function significantly. Jaundice is generally mild or absent, but pressure over a major hepatic duct can give rise to obstructive jaundice. On aspirating the pus, the liver tissue comes into apposition and complete healing occurs without structural damagte or fibrosis.
During acute amoebic dysentery, the liver may enlarge as a result of diffuse inflammation caused by the products of inflammation of the colonic tissue and bacteria reaching the liver in the blood stream. The hepatic lesion clears up with cure of the dysentery. This lesion should not be mistaken for liver abscess.
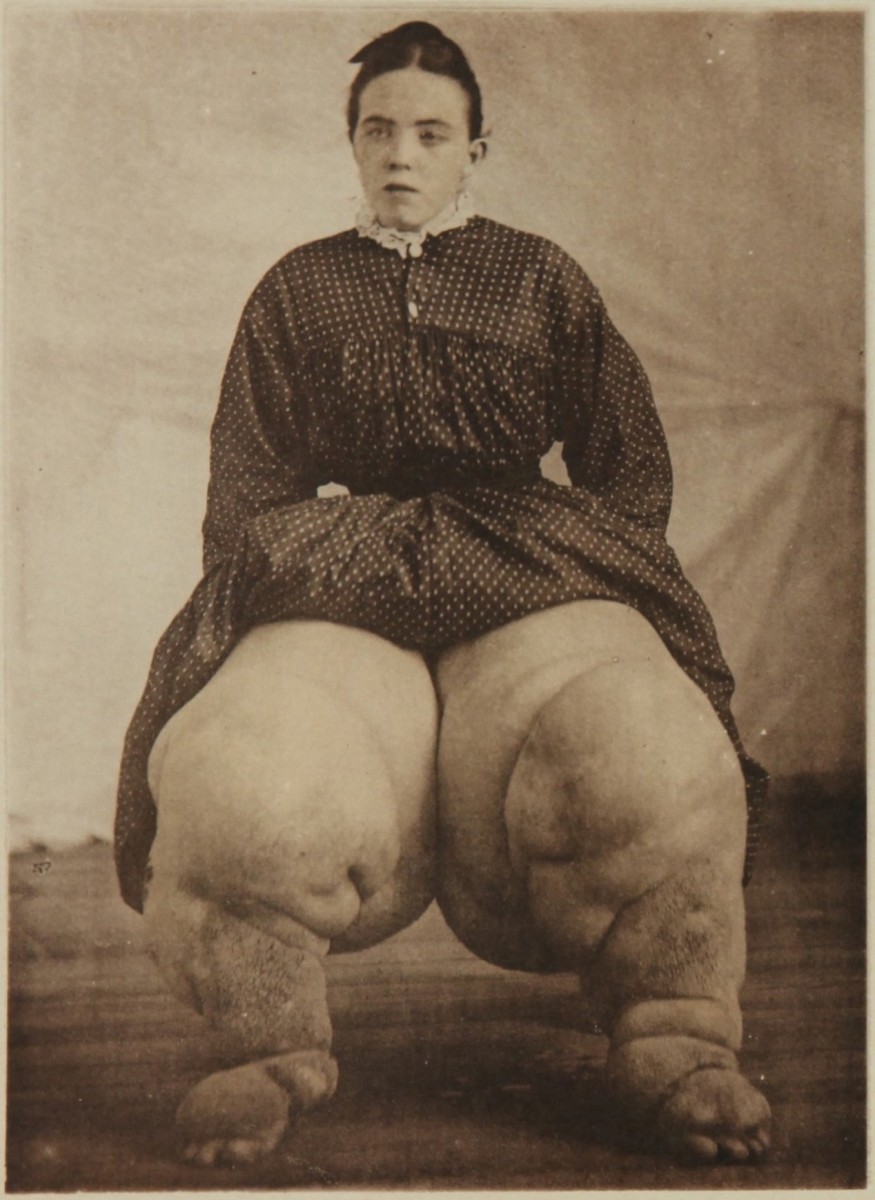
Other foci for embolic lesions include the lungs, brain, spleen and other tissues. Direct invasion of the skin by active vegetable amoebae leads to extensive spreading necrotic ulceration (or) cutaneous amoebiasis.
How To Diagnose Amoebiasis

Infectious Diseases
Diagnosis Of Amoebiasis
Differential diagnosis: Amoebic dysentery has to be differentiated from baciliary dysentery, ulcerative colitis and tuberculous enterocolitis. Amoeboma may closely resemble carcinoma. Chronic intestinal amoebiasis may be misdiagnosed as irritable bowel syndrome, diverticulitis, neurasthenia or malabsorption state. Hepatic amoebiasis is a common cause of prolonged fever in the tropics and when liver enlargement and tenderness are not marked, it resembles enteric fevers, brucellosis or tuberculosis.
In an endemic area, enlargement and tenderness of the liver should suggest the diagnosis of amoebic liver abscess. Other conditions such as alcoholic liver disease, primary and secondary tunours of the liver, subdiaphragmatic abscess and pyogenic liver abscess have to be differentiated. In case of doubt, the diagnosis is confirmed by aspiration of pus from the abscess. Prompt response to antiamoebic drugs is a point suggesting a diagnosis of hepatic amoebiasis.
Laboratory diagnosis: Serological tests are positive in extraintestinal forms of amoebiasis, especially when the liver is affected. Of the tests, indirect hemagglutination test has been found to be most sensitive. Other tests like indirect immunofluorescence, countercurrent electrophoresis and agar gel diffusion are also useful.
How To Diagnose And Treat Primary Amoebic Meningoencephalitis

Primary Amoebic Meningoencephalitis
Some species of free-living soil amoebae of the genus Naegleria may produce primary amoebic meningo-encephalitis, which is a rapidly fatal disease. The organisms are carried in the nose and throat of asymptomatic carriers. It is seen worldwide, occurring sporadically.
Naegleria gruberi is the common pathogen. The genus Hartmanella (Syn: Acanthamoeba) can also affect man. In most of the cases, a history of swimming or bathing in contaminated water may be obtained. The organism enters through the roof of the nose and spreads up the cribriform plate or reach the subarachnoid space. The brain is edematous and covered by a blood-stained purulent exudates, especially in the basal cisterns. Amoebae are also seen invading the grey matter.
Clinical features: The incubation period is 2 to 14 days after a possible exposure. The clinical picture resembles acute meningitis. The CSF is under tension and it is turbid or blood stained Microscopy shows erythro ytes, numerous polymorphs and motile amoebae containing ingested erythrocytes which may be mistaken for macrophages. The species of amoeba can be identified by suitable staining. Amoebic meningoencephalitis is associated with high mortality occurring within 2 to 5 days. Present treatment is not fully satisfactory.
Treatment: Amphotericin B given intravenously in a dose of 0.25 mg/Kg daily for 8 days is partially effective against Naegleria. The drug can also be given intrathecally in a dose of 0.5mg diluted in 5ml of CSF, thrice a week.
Acanthamoebae: (Hartmanella) are free-living amoebae seen in soil and water. Thse become pathogenic to immunocompromised hosts. They gain entry through the nasal mucosa, abrasions on the skin or eyes. Pathogenicity is similar to that of Naegleria.
© 2014 Funom Theophilus Makama