Attention Deficit Hyperactivity Disorder (ADHD) – An Emerging Threat to Normal Child Development

Exploring ADHD
In today’s age of technological advancement, lifestyle modifications with their own benefits and risks make the population of the 21st century prone to a number of psychosomatic disorders. Attention Deficit Hyperactivity Disorder (ADHD) is one of those mental ailments that somehow obstruct the normal physiological development of a child until the onset of maturity. In clinical terms, ADHD is defined as a childhood neurodevelopmental disorder adversely influencing a patient’s competitive ability and mental development leading to reduced cognition beginning from childhood until adolescence.
Well-recognized impulsive patterns of hyperactivity, sustained inattention, behavioral imbalances, restlessness, distraction, hyperkinesis, brain dysfunction, lack of concentration, daydreaming, confusion, cognitive conflicts, and forgetfulness are observed in clinically confirmed cases of ADHD.
The children affected with the onset of ADHD often display symptoms of constant mobility, excessive talking, discomfort, lack of patience, interruptive conduct, indiscipline, and difficulty in performing school assignments. The patients with ADHD lack attention and exhibit delays in accurately grasping and processing information, react abruptly, do not respond to directions, remain irresponsible with a tendency to lose things, miss details and switch between the activities. Most of such children experience performance issues at school and fail to acquire good grades leading to poor academic records.
Although the disease predominantly influences children, its effects extend until adulthood resulting in social problems and functional difficulties among the impacted individuals.
The children affected with ADHD face challenges with their working memory and remembering things. They remain disorganized and tend to lose focus on their activities. They lack time management skills and have difficulty acclimatizing with other children of the same age groups.
ADHD patients are devoid of contemplation, self-insight, and thoughtfulness. They often have difficulty in talking, reading, comprehension, and regulating their emotions. They lack willpower, motivation, alertness and frequently experience daydreaming. Such patients are predominated with reduced intellect and problem-solving abilities, feel defeated by the challenges of life, and lack vision and clarity in their future goals and achievements. The affected children fail to write words in an organized manner and are unable to coherently respond to situations and rapidly assemble ideas and actions following their circumstances. These children tend to deflect from normal work capacity and display uneven patterns of productivity and accuracy in their work with a high degree of variation. At times, they are active and perfectly perform their tasks; however, many times they get erratic, lazy, and unwilling to accomplish their assignments. The victims of ADHD experience symptoms prior to the age of 13 years, with the onset of hyperactive and impulsive behavior. The symptoms, if sustained may adopt a chronic course, continue until the beginning of adolescence, and manifest in adulthood.
Problems in Adulthood
5 – 10 % of the children suffering from ADHD may acquire manic depression or bipolar disorder leading to serious mental manifestations. However, 10 – 20 % of patients suffer from a personality disorder, delinquency, and substance abuse. Adults with ADHD remain under-educated and under-employed relative to their intellectual ability, intelligence, education, and family backgrounds. They continue to exhibit hyperactivity, interpersonal problems, and instability at the workplace.
ADHD patients are more prone to post-marital conflicts, divorce, and poor social relationships. They are not able to drive well, especially in traffic-prone areas, and are likely to encounter road traffic accidents due to their negligent driving.
Etiology and Prevalence
ADHD patients display deformity in executive functions that adversely influence their self-regulation, cognitive flexibility, sequencing of behavior, response inhibition, planning and working memory. Genetic factors to an extent believed to be the predisposing factors of occurrence of this disease. Apart from the genetic factors, pregnancy complications, smoking and alcoholism during pregnancy, premature birth, postnatal defects, disorganized lifestyle, chronic stress, and exposure to lead and neurotoxicants like pesticides, nicotine, solvents, and heavy metals are the causative factors enhancing the onset of ADHD.
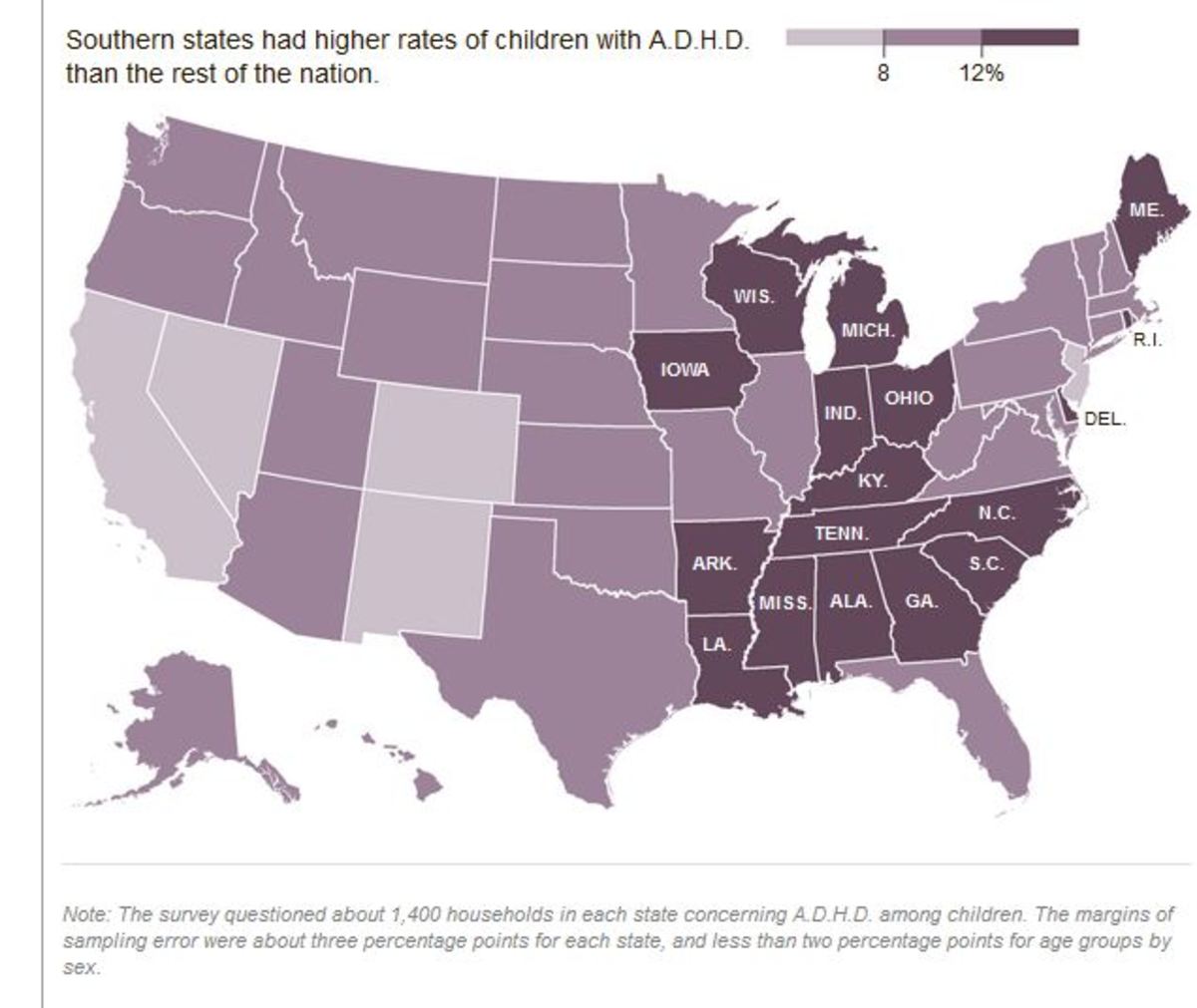
This disease is not confined to geographical boundaries, and almost every country has reported cases of ADHD at some point in time. ADHD is expected to dominate in people with a family history of depression or other behavioral disorders like Tourette syndrome and oppositional defiant disorder.
Diagnosing and Managing ADHD
The first step in challenging this behavioral disorder is confirming diagnosis through a detailed assessment of the affected children. Clinical neuroimaging studies including EEG, SPECT, PET, and MRI are helpful in tracking functional alterations and reduced blood flow (in front striatal circuitry and the cerebellar vermis of the human brain) as significant contributing factors in the occurrence of ADHD.
The patients must not be humiliated for their non-performance in school, and thorough monitoring of the symptoms is required for exploring the severity of illness in the diseased individuals. Special training needs of disabled children require attention and accomplishment for effective management of this behavioral problem. The schoolteachers and parents need to render special counseling sessions with the help of psychotherapists to the affected children for controlling disease progression. Indeed, good parenting skills are highly required to antagonize a child’s disruptive behavior by instilling enthusiasm and courage with consistent positive feedbacks, praises, and rewards.
Medicinal Treatment
Traditionally prescribed drugs like Ritalin, Methylin, Dextroamphetamine, Dexedrine, Metadate, and Concerta impart psychoactive effects on the diseased children, with possible adverse impacts on memory and behavior. Integrative medicine presents combination therapy with herbs for acquiring increased cognition and neuroprotection among the affected population. Botanicals like St. John’s Wort, Melatonin supplements, Chamomile (Manzanea), Lemon Balm (Melissa officianalis), Valerian (Valeriana officianalis), Kava Kava, Ginkgo biloba, Ginseng, Biota, Schizandra and Pycnogenol offer promising remedies in curing ADHD. These botanicals enhance the body’s neurotransmitters, rectify sleep patterns, induce antispasmodic and sedative effects, and render anti-stress, anxiolytic, muscle relaxant, and analgesic responses resulting in increased blood flow, improved cognition, memory, and reduction in oxidative neuronal damage by rectifying defective dopamine transport mechanism in the diseased individuals.
Clinical studies reveal the neurotoxic effects of food additives like bleaching agents, emulsifiers, preservatives, artificial flavorings, and colorings on the human population. Similarly, allergens including eggs, soy, wheat, corn, peanuts, white vinegar, almonds, tomatoes, chicory, plums, fish, and raspberries may selectively irritate or render toxic effects on the nervous system of ADHD victims. Therefore, such ingredients are not recommended in the diet for sustaining health and facilitating recovery in the affected patients.
Indeed, the importance of nutrients like iron, zinc, magnesium, vitamin B6, megavitamins, and essential fatty acids lies in enhancing mental arousal, attentiveness, social responsiveness, behavior, attention span, IQ, and challenging severe manifestations of ADHD in children and adults of variable age groups.
Other Therapies
Regular exercise, meditation, spirituality, hypnotherapy, guided imagery, Neurotherapy (by EEG biofeedback), behavior management, massage therapy, osteopathic manipulative therapy, multisensory communication, positive reinforcement, practicing patience, and consuming a balanced diet facilitate in antagonizing behavioral imbalances, depression, impulsiveness and hyperactivity in patients of ADHD.
A blend of alternative therapy, traditional treatment approaches, and behavior management potentially alters the progression of ADHD by establishing psychological well-being and stabilizing physiological processes resulting in highly effective and self-sufficient mind-body coordination in ailing patients.