Avoiding the Complications of Diabetes – Diabetic Neuropathy
One of the most prevalent and frequent complications of diabetes globally is the onset of diabetic neuropathy. The probability of developing diabetic neuropathy intensifies with the advancement of age and duration of diabetes.
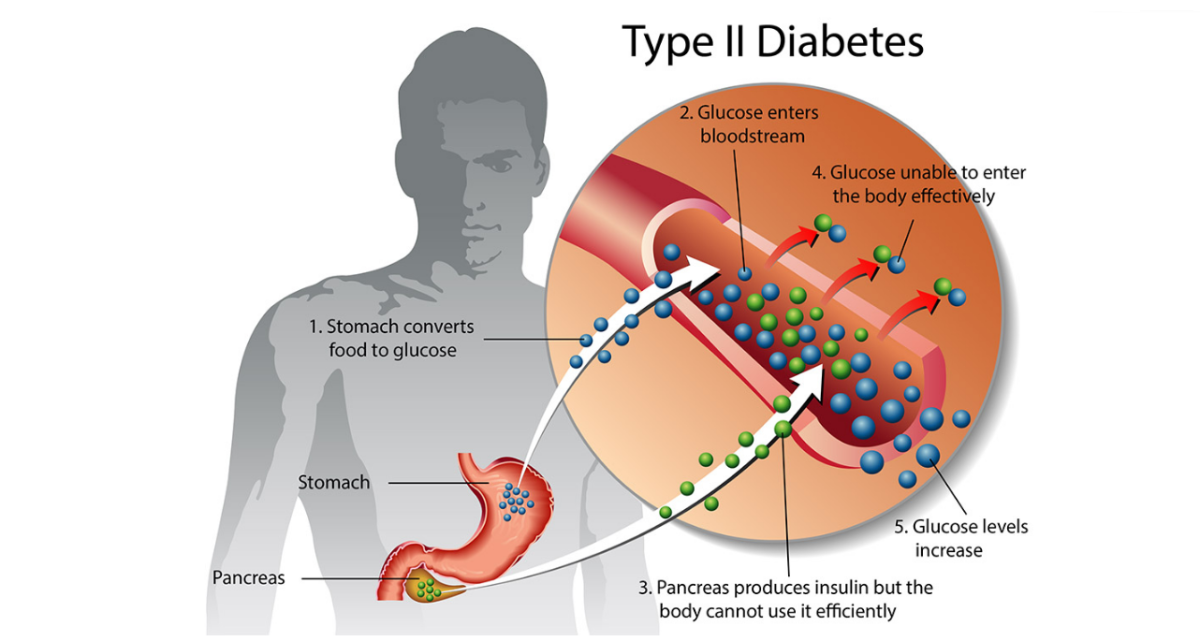
Unusually high blood glucose levels are usually the causative factors which cause the inception of nerve impairment. Diabetic neuropathy still remains a medical condition that has no cure, but there are various treatment options and alternatives accessible, which can assist in pain and symptom management. Diabetic neuropathy can be prevented or its development can be precluded if the blood sugar is kept under strict control.

Indications of diabetic neuropathy
Diabetic neuropathy can be categorized into four types of neuropathies, which have their own set of symptoms. The categories of diabetic neuropathy are:
Peripheral neuropathy
This is one of the most prevalent types of diabetic neuropathy, and the peripheral nerves, which are located in the hands and feet, become impaired. Some of the symptoms which are manifested when peripheral neuropathy strikes are:
- Loss of sensation, tingling and burning sensation in the hands and feet
- Jabbing, shooting and sensations that simulate electrical shocks
- Extreme sensitivity to stimuli
- Decreased perception of pain and temperature
- Weak muscles
- Trouble walking at a normal pace and with steady gait
- Unable to notice foot problems like ulcers, sores and infections
Autonomic neuropathy
The autonomic nervous system is accountable for managing the involuntary functions like the heart rate, bladder function, sweating, and gastrointestinal function. Diabetes can adversely influence the nerves that are situated in these areas, and so the symptoms which become discernible are:
- Bladder problems like urinary incontinence
- Constipation, diarrhea
- Profuse or decreased sweating
- Digestive problems
- Heart rate and blood pressure are not regulated normally
- Sexual disorders like vaginal dryness in women and erectile dysfunction in men
Proximal neuropathy
This is also termed as diabetic amyotrophy or femoral neuropathy, and this category of nerve damage affects the thighs, buttocks, legs and hips. Mostly older people who are battling with type 2 diabetes are commonly affected by this type of neuropathy, and the symptoms are usually noticeable only on one side of the body. This neuropathy is distinguished by:
- Intense shooting pain
- Wasting of the muscles
- Abdominal swelling
- Unexplainable weight loss
Mononeuropathy
In this type of neuropathy, a single nerve or a group of nerves located in the face, torso or leg is affected. It is also known as focal neuropathy and usually affects older individuals suddenly. Although excruciating pain is the hallmark symptom of mononeuropathy, the pain is not continuous and symptoms begin to show improvement with time. Some of the perceptible symptoms are:
- Double vision
- Pain experienced in the shin, foot and front of the thigh
- Paralysis on one facial side
- Pain in the chest or abdomen
How is diabetic neuropathy diagnosed?
The healthcare provider will take a complete medical history, carry out a physical and neurological exam and will ask the patient to describe the symptoms in detail. Some of the other tests which are carried out to establish the exact cause of neuropathy are:
Filament test: a monofilament which is in the shape of a soft, nylon fiber is kept on the feet. If the patient is unable to detect it on the feet, it means that nerve damage has been sustained.
Nerve conduction studies and EMG: these tests are often conducted in conjunction with one another to test the speed and intensity of the electrical impulses that are relayed by the nerves.
An annual foot exam is also recommended for diabetic patients so that any incidence of infection, sores or abnormalities can be detected and treated early before causing major complications.
How to treat diabetic neuropathy?
Some of the commonly prescribed medications for assisting in symptom and pain management are:
- Anti-seizure medications
- Antidepressant
- Lidocaine patch
- Capsaicin cream
- Opoids
Diabetic patients are advised to keep a persistent check on their blood glucose levels to slow down the progression of diabetic neuropathy and to reverse the symptoms. A research suggested that strict control of blood glucose levels could reduce the risk of developing diabetic neuropathy by 60%. Developing healthy habits like visiting the specialist regularly, taking the medications, opting for healthier food options, exercising regularly and smoking cessation is advisable for diabetic neuropathy patients for better management of their condition. Foot care should be the top priority of diabetic neuropathy patients because loss of sensation can cause many wounds to go undetected, which can cause severe infections and ultimately lead to lower limb amputation.