Behavioral Health Care: Assessment, Treatment and Health Insurance Coverage
What is Behavioral Health Care?
Behavioral Health Care includes treatment for mental health and substance use disorders. Most health insurance companies provide benefits for behavioral health. Some health plans have generous behavioral health benefits and some plans have limited or no benefits for behavioral health. Most people are not familiar with behavioral health care or with their behavioral health coverage.

Initial Contact with a Provider
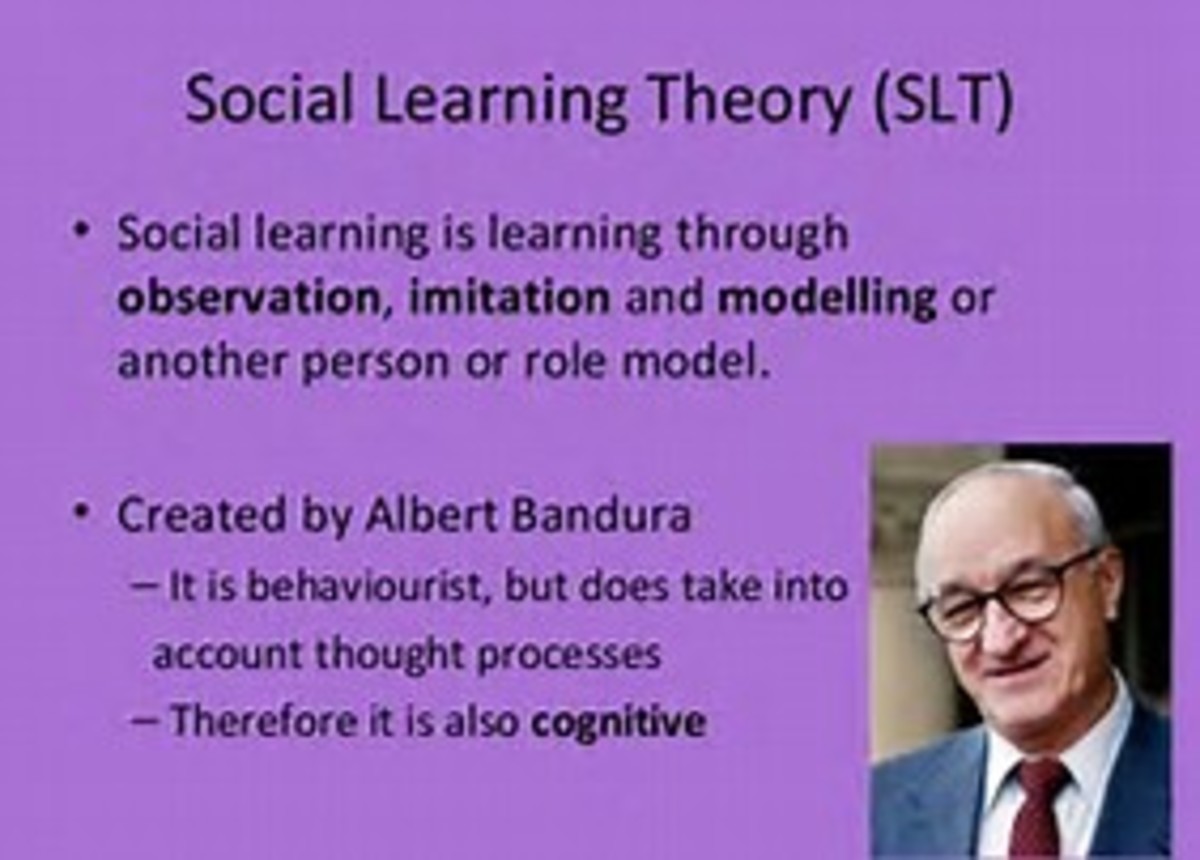
Usually, a person initiates contact with a behavioral health care provider in an outpatient setting. They call for an appointment and meet with a therapist in the office. For some, the first contact with a behavioral health care provider is in the Emergency Room or in the hospital while they are getting care for a medical condition. If a behavioral health condition contributes to or complicates a medical condition, a consultation may be requested with a behavioral health professional. Whether the initial contact occurs in an outpatient setting, in the emergency room or in the hospital, an initial behavioral health assessment is completed.
Initial Assessment
During the initial assessment, questions are asked about symptoms and problems, current and past stressors and events, family, relationships and social support systems, academic and occupational functioning, current and past psychiatric symptoms and substance use patterns, treatment history, thoughts about harming self or others, spiritual and religious beliefs, personal strengths, medical history and current medical conditions, as well as some demographic information such as name, age, address and phone number. The purpose of the assessment is to determine what, if any, mental health or substance use disorders exist and to identify treatment needs. From the initial assessment, problems are identified, a diagnosis is made and a treatment plan is developed with the goal of eliminating or decreasing the symptoms and problems identified in the initial assessment.
Mental Health Conditions
Mental health conditions include mood disorders such as depression and bipolar disorders. They include anxiety disorders such as PTSD (post traumatic stress disorder), panic disorders with or without agoraphobia (fear of open spaces where a person is confined to their home out of fear of having panic symptoms in public), OCD or obsessive compulsive disorder (where a person might feel compelled to repeat a behavior in order to avoid experiencing an intrusive thought or feelings of guilt). Mental health conditions include psychotic disorders such as schizophrenia where a person experiences hallucinations and delusions (sees and hears things other don’t see or hear and believes things that aren’t reasonable). Mental health conditions in elderly patients could include delirium or behavioral disturbances in dementia. Mental health conditions can also include adjustment difficulties, grief and loss, relationship problems, childhood behavior problems, and abuse issues.
Substance Related Conditions
Substance related conditions can include symptoms of depression, anxiety and psychosis that are substance induced, or caused by substance use. Substance related conditions can include withdrawal and intoxication symptoms. Accurate assessment of withdrawal potential and withdrawal symptoms is important. Withdrawal from alcohol and benzodiazepines (valium, xanax, klonopin, etc.) is potentially life threatening. Withdrawal from heroin and other opiates, such as oxycontin and other pain pills, is not generally life threatening but can be complicated by other medical or psychiatric conditions. Questions about the quantity and date of last use of alcohol and other drugs are asked to assess for withdrawal potential and severity. Substance related conditions include substance abuse and dependence, and a host of bio-psycho-social problems that are caused by ongoing substance abuse and dependence.
Co-occurring Conditions
Mental health conditions and substance related conditions are often still treated at separate facilities, even though it is increasingly rare that a person would have one without the other. A person with psychiatric symptoms often uses substances in a misguided attempt to “self medicate” their symptoms. A person with a substance use disorder often develops psychiatric symptoms as a consequence of their use. Some facilities do offer “dual track” programming for co-occurring substance abuse and mental health conditions so that both conditions can be treated at the same time. Often a decision is made to treat one condition first, and then follow up is recommended to treat the other condition. If the recommended follow up care is not pursued, it is highly likely that a relapse or recurrence of both conditions will occur as the course of treatment is not complete.
Level of Care
Another important component of the behavioral health assessment is the level of care determination. Behavioral health care can be provided on an outpatient basis, in the hospital as acute inpatient care, at a partial hospitalization program or day treatment program, or in an Intensive Outpatient Program. The level of care is determined by the severity of symptoms and the intensity of services provided at that level.
Outpatient Treatment
Treatment as an outpatient is typically held in the therapist’s office every week or every two weeks. In some instances, during a crisis or time of high risk, it might be necessary to see a therapist in the office two or more times a week for a few weeks until symptoms are stabilized or the crisis is resolved. Rarely would it be necessary to see a therapist this frequently for a long period of time, especially if no progress is being made in the therapy. If symptoms are severe and no progress is being made, a higher level of care should be considered. If symptoms are mild or stable, the frequency of sessions is not indicated. The frequency of visits should decrease or therapy should be terminated with that provider. Sometimes monthly maintenance visits are helpful to prevent a recurrence of symptoms, especially with a severe, recurrent depression.
Inpatient Hospital Treatment
Acute inpatient hospital treatment is for the most severe and life threatening symptoms. A person who is suicidal, has a suicide plan, intends to carry out the plan, and has the means to carry out the plan definitely needs to be in an inpatient setting. Likewise, a 62 year old man who has been drinking a fifth of whiskey a day for the past forty years, has a heart condition, and has a history of DTs and seizures when he stops drinking will need to be inpatient for detoxification in order to safely stop drinking. On the other hand, a 23 year old male who has been smoking marijuana daily for three years does not need to be in an acute inpatient setting. Acute inpatient treatment is reserved for conditions that are life threatening or symptoms that are so severe that the person is unable to care for himself. An inpatient stay is typically very brief and the patient is discharged as soon as he or she is stable and able to stay safe.
Residential Treatment
Some health plans include benefits for residential treatment. Most do not. Residential treatment is not the same as acute inpatient hospital care. Around the clock medical care is not available in a residential treatment facility. Residential care is a sub acute level of care. In a residential setting, treatment is provided for about six hours a day. The setting is very structured and the patient lives on site and attends programming during the day. If our 23 year old marijuana user failed an Intensive Outpatient Program, he might be a good candidate for residential treatment. His insurance plan may not cover his residential treatment though.
Partial Hospitalization Programs (PHP)
Partial hospitalization is sometimes known as day treatment. It is a step down from acute inpatient. Medical care is still available but the patient is able to go home at night. Usually partial programs are six hours a day and are completed in fewer than ten days.
Intensive Outpatient Programs (IOP)
Intensive Outpatient Programs (IOPs) are typically three hours each day for three days a week, and can be in the day time or in the evening. Some Intensive Outpatient Programs are four to seven days a week. IOP can be as short as a week or two, but is usually four to six weeks, depending on progress and symptom severity. Physician and nursing care is not typically provided at this level of care, although a patient might see a physician on an outpatient basis while attending IOP.
Long Term Care
Some patients do not get better after treatment, and may require placement in a nursing home upon discharge from the hospital. Some may require longer term placement in a state hospital or mental institution. They may be released after a longer course of treatment or remain in the institution long term.
Medical Neccessity
When behavioral health care is a covered benefit in a health insurance plan, the care provided must be “medically necessary.” If it is not medically necessary, it is not covered, and insurance will not pay for it. A person might have “unlimited” inpatient days or outpatient visits for behavioral health treatment, but if the care is not medically necessary, it is not covered.
When an authorization request is made for a behavioral health service, a behavioral health professional employed by the health insurance company reviews the request. If the request is for additional hospital days but the patient is stable and no longer a danger to self or others, the request for coverage for continued stay at the inpatient level may be denied. Likewise, if a patient has been seeing an outpatient therapist three days a week for six months, is not making progress toward getting better, and refuses to take medications that are known to relieve symptoms, the request for continued authorization for care may be denied. In both instances, the medical necessity criteria for continued care were not met.
Summary
In summary, behavioral health care is health care that is directed toward mental health conditions and substance use disorders. The first visit with a behavioral health care professional typically includes an initial assessment of needs to be addressed in treatment. A treatment plan is developed from this initial assessment that includes goals of treatment. Subsequent visits will be aimed at meeting treatment goals. The provider will use methods and interventions that are known to be effective in treating the conditions identified as problematic. Part of the assessment involves determining what level of care is needed, with a preference for “least restrictive” levels of care. Health insurance benefits may or may not cover behavioral health treatment. When behavioral health is a covered benefit, the treatment must meet medical necessity criteria in order to be covered.