Chronic Gastritis Caused By Helicobacter Pylori Effect: The Story Of Liam Zopper From Sydney, Australia
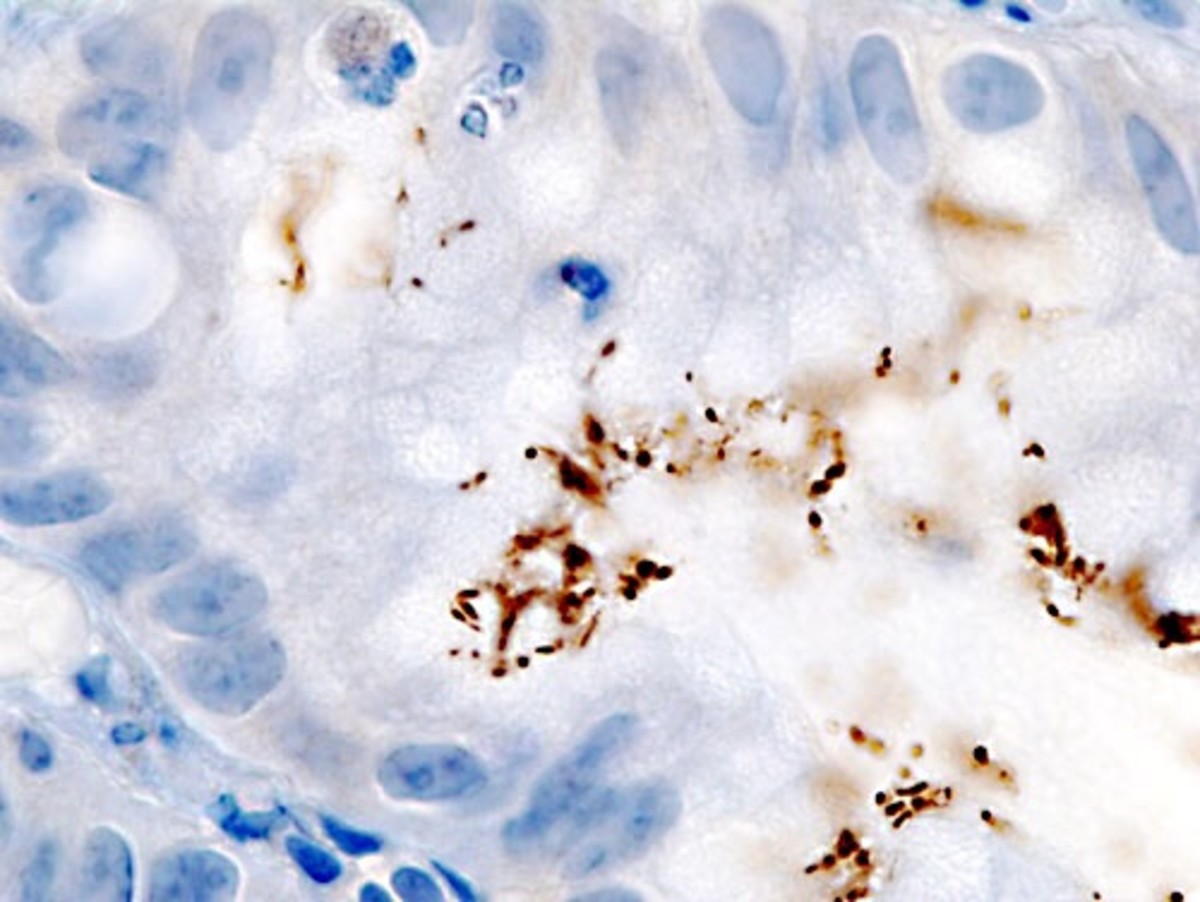
Erosion of the Muscosa lining in Gastritis

Pain Syndrome
The Story of Liam Zopper
Liam Zopper lives in sydney, Australia. On a Tuesday, after work, he felt sharp pain just below his chest, on the region where the abdomen begins. With time he began nauseating and quickly left for the Hospital. A series of diagnostic examinations was carried out, including a breathe test and then the doctors told him, he has Chronic gastritis due to a stomach infection.
More curiosity from Mr. Liam made him discover this infection is caused by an organism called Helicobacter Pylori. So, what is Gastritis? Will Mr. Liam be okay? Is he in a critical situation?
Epigastric Pain in Gastritis

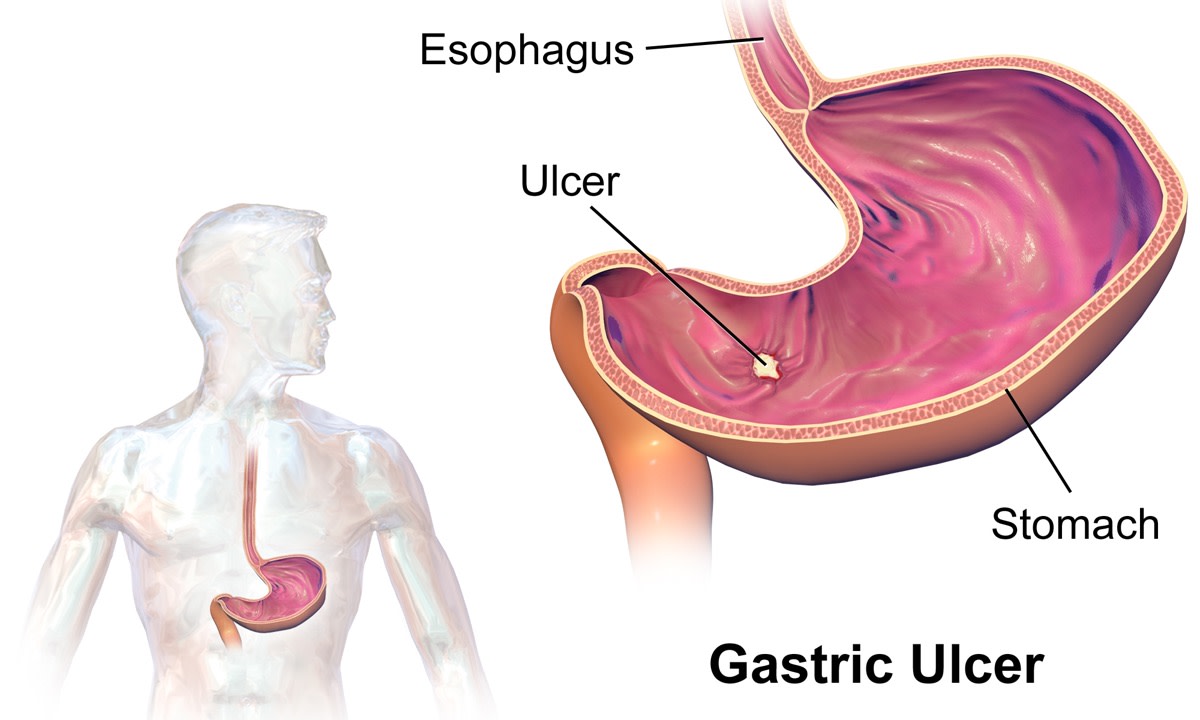
What is Gastritis?
Gastritis is the change in the normal state of the stomach mucosa wall (the internal walls of the stomach). Usually, this change is an inflammation. Gastritis is best diagnosed histologically through endoscopy and some of what we see on the stomach wall are Mucosal congestion, Oedema, acute hemorrhagic erosive lesions and sometimes substantial reduction in mucosal blood flow.
Gastritis could happen during a short period of time and hence Acute, but it could also occur in a long duration and hence Chronic (> 6 months). There are three main sub types of Gastritis and they are:
- Gastritis due to autoimmune processes- In this case, the body defense mechanism which supposed to fight any foreign body turns against itself and begin to target some body organs as foreign, thereby fighting them. In Gastritis, these defense cells attack the parietal cells of the stomach which are responsible for secretion.
- Gastritis due to Bacterial infection (Helicobacter pylori).
- Gastritis due to chemicals and drugs.
In Liam's case, he suffered the second sub type and we will now take our time to evaluate this kind of gastritis.
Helicobacter Pylori
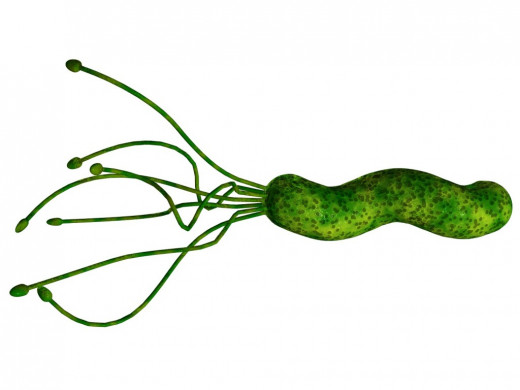
Helicobacter Pylori
Helicobacter pylori is a spiral shaped, microaerophilic, gram negative bacterium measuring approximately 3.5 microns in length and 0.5 microns in width. It is the most common chronic bacterial infection in humans of which 50% of the world's population is affected.
The stomach environment is highly acidic which is the appropriate environment for digestion and secretion of digestive enzymes. H. Pylori survive by producing the substance Urease which forms ammonia and bicarbonate that neutralize gastric acid and form a protective cloud around the organism. This makes Urease a very important substance for its survival and colonization and hence produced in abundance, making up more than 5% of the organism's total protein weight. This is of diagnostic importance as a Urease breathe test to check for the presence of Urease in the stomach confirms H. Pylori infection.
It has other characteristics, enabling its survival, like spiral shaped flagella which facilitate its passage through the mucous layer. Also, its ability to attach itself to gastric epithelial cells by means of specific receptor-mediated adhesion.
H. Pylori causes pathology by adapting to live in association with barrier; then causes cell damage and inflammatory cell infiltration which is now Gastritis.
Urea Breath Test

Clinics
The routs by which infection occurs remains unknown, but person to person transmission of H. Pylori through either fecal-oral or oral-oral exposure seems most likely.
Possible Signs and symptoms
- Abdominal pain (epigastric, especially)
- Indigestion
- Nausea
- Vomiting
- feeling of fullness
Diagnosis
- Complete Blood count
- Biochemical analysis of blood
- Stool test
- Urease Breathe test
- Endoscopy
Treatment
A triple PPI therapy is prescribed and taken twice daily.
Lansoprazole (prevacid): 30 mg Per Os, or Omeprazol (Prilosec): 20 mg Per Os
Clarithromycin (Braxin) 500 mg Per Os
Amoxicillin 1g Per Os, or Metronidazole 500 mg Per Os
Non Invasive diagnosis for helicobacter Pylori Infection
Tests
| Methods
| Main Use
| Comments
|
|---|---|---|---|
13-C Urea breath test
| hydrolysis of ingested 13-C urea by H. Pylori to produce 13-C in expired air
| Diagnosis of infection and monitoring of infection later, after eradication
| Highly sensitive and specific False-negative results after recent use of PPIs or antibiotics
|
Stool antigen test
| Immuno assay using monoclonal antibodies
| same
| Same
|
Serology
| Serum antibody detection
| Diagnosis of infection, Epidemiological studies
| Inaccuracy limits use. Antibiotics remain positive after infection cleared
|
From Essentials of Kumar & Clark's Clinical Medicine Handbook 5th Edition, page 81
Invasive Tests (endoscopic Gastric Mucosal biopsy)
Invasive tests
| Methods
| Main use
| comments
|
|---|---|---|---|
Rapid Urease (CLO) test
| Urease from H. Pylori breaks down to form Ammonia, causing a pH dependent colour change in the indicator present
| Diagnosis of infection in patients already undergoing endoscopy
| Highly sensitive and specific False-negative results after recent upper gastro-intestinal bleeding and recent use of PPIs and antibiotics
|
Histology
| Direct visualization of the organism
| Subject to sampling error and observer variability
|
Essentials of Kumar & Clark's Clinical Medicine, Handbook, 5th Edition, page 81
© 2014 Funom Theophilus Makama