Chronic Obstructive Pulmonary Disease and Its Ever Growing Complications
Chronic Obstructive Pulmonary Disease And Its Ever Growing Complications
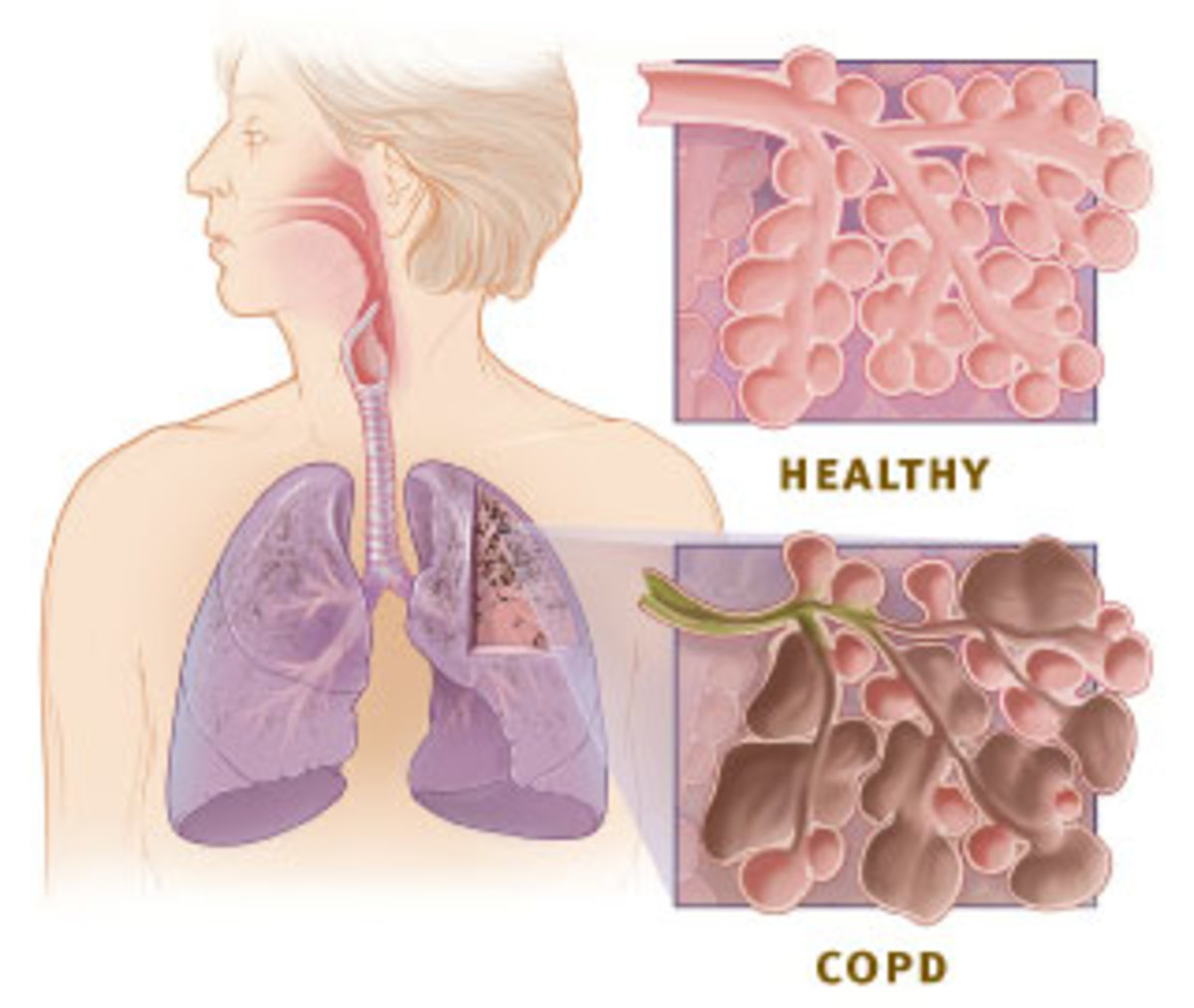
Chronic obstructive pulmonary disease (COPD) is a type of obstructive lung disease characterized by long-term breathing problems and poor airflow. The main symptoms include shortness of breath and cough with sputum production. COPD is a progressive disease, meaning it typically worsens over time.
People living in industrial area, mainly asbestos, coal mines area are more prone to COPD; the main problem is they are not able to breathe fresh air. The air around the mines and asbestos industry is filled with very minute pollutants making it impossible to make a safe living in those areas. Mainly children are affected.
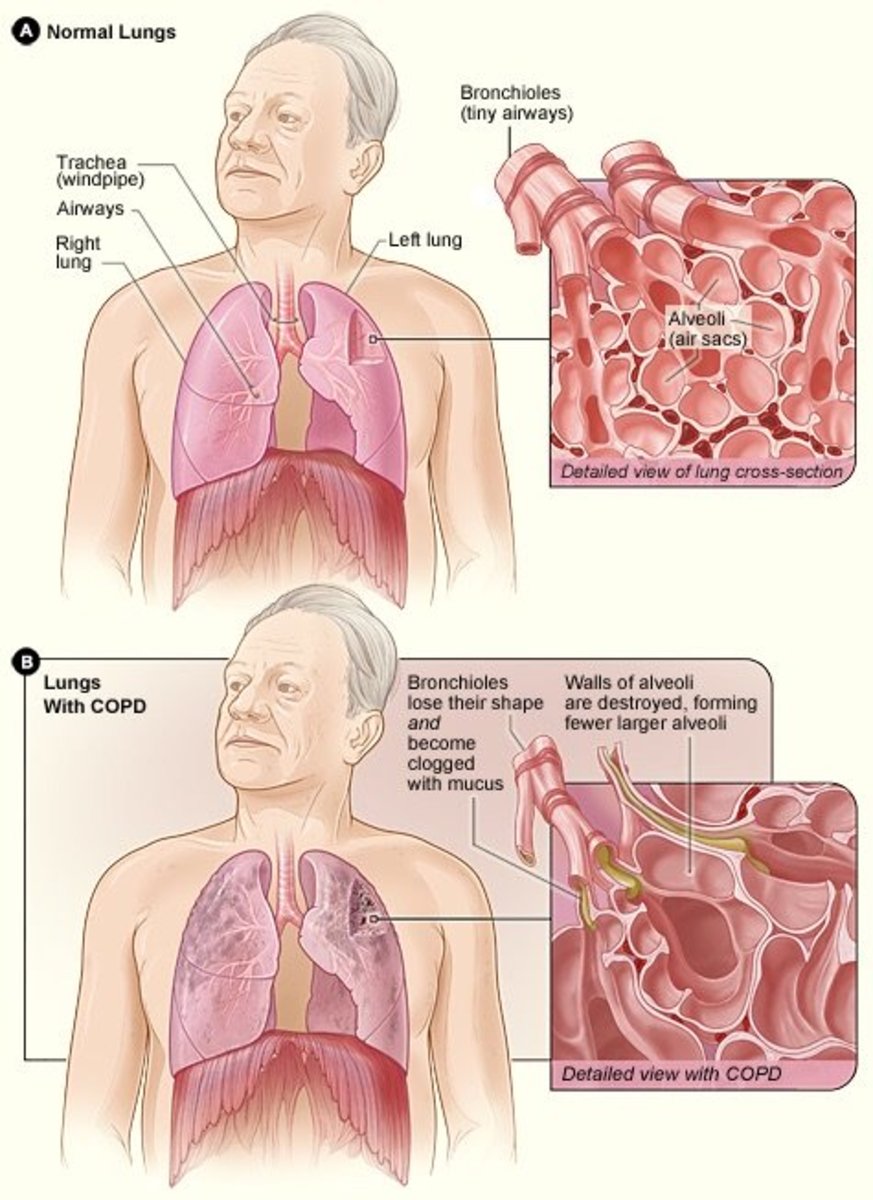
Technically, there are two conditions with COPD, chronic bronchitis, and emphysema. Sometimes, people consider asthma as part of COPD, but we are going to keep it separate for itself. The main ones that we usually classically associate with is chronic bronchitis. It could be seen by mucus production, productive cough that is one of those hallmark signs of chronic bronchitis. Usually it cannot be diagnosed based on clinical diagnosis, as to how much sputum the patient is producing, how often, how long that kind of stuff. The other condition is emphysema, (a condition in which the air sacs of the lungs are damaged and enlarged, causing breathlessness). Emphysema is usually described as being structural changes. The biggest risk factor associated with COPD, causing 90 to 95% of COPD cases is smoking. Smoking is the number one cause of COPD. All other ones are less common, but still important to mention is going to be environmental exposure, certain things where people are exposed to a lot of dust, silica, and another one is just air pollutants from exhaust from different types of things within the atmosphere. Another big one is actually going to be a genetic condition, and this is going to be called alpha-1 antitrypsin deficiency. This is the least common, but it can happen, it is an autosomal dominant disorder, one of the things with this one is that usually you have to have a family history of COPD, some underlying unknown reason why there is liver disease, and also they usually have to be less than about 45 to 50 years old in order to take into consideration alpha-1 antitrypsin deficiency.
One other point to make sure is that COPD is not always clear-cut. It is not always the sense that one only has chronic bronchitis, or he or she only has emphysema. One of the big things that we need to understand is these things often coexist. That is an important point to remember.
Chronic bronchitis is usually associated with mucus build up. We have the mucosal lining, which is the epithelial tissue, may be some lamina propria (The lamina propria is a thin layer of loose (areolar) connective tissue, which lies beneath the epithelium, and together with the epithelium and basement membrane constitutes the mucosa). Outside of that we have submucosa, which is kind of a loose connective tissue, and there are submucosal glands. They are naturally producing mucus to humidify the airways to trap certain types of pathogens, and help to be able to keep the airway moist, and humidified. In situations with chronic bronchitis the problem is that the mucus production increases significantly, and it is the result of usually these irritants, smoking, dust exposure, and what happens is this mucus plugging causes the narrowing of the airway. One could obviously see that because obstructive disorder is the narrowing of the airway. One of the big things here one has to remember is there is going to be hypertrophy and hyperplasia of these mucous glands, and it is because of airways coming into contact with all these irritants, the smoke, dust, silica, pollutants, and it is causing agitation of the mucosa, and the way that our actual body deals with that is we stimulate these mucous glands to produce more mucus to coat that area. So because of that one of the classic things that we will see here is hypertrophy and it is just an increase in size of the mucous glands, they are going to get bigger. The second thing is that you are going to make more of them, so that is called hyperplasia, and these are the classic signs for these mucous glands. Because we also have other cells that are important for the mucus production, there are a couple of them scattered around the airway. We have these special cells, and they are called goblet cells, (goblet cells are simple columnar goblet shaped like epithelial cells that secrete gel-forming mucins, like mucin MUC5AC). Goblet cells are also responsible for producing that mucus, and it is more of alkaline mucus, which helps to be able to coat the airway, it helps to moisten the air, humidify the air, helps to be able to filter out any pathogens. Because of this these different risk factors there is going to be hypertrophy, hyperplasia of the mucous glands, as well as for the goblet cells.
The next thing that happens is unfortunately, smoking especially, there is so much irritation in this area that it can actually cause destruction of the cilia. So there could be ciliary shortening, and they are also going to have less motility. So, because of that there is accumulation in the airways, and this mucus is going to be really hard to get out. Because of that the patient is going to have ciliary dysfunction. This is due to the cilia getting shorter, become less motile and not able to beat that mucus, because that is one of the function of the cilia, they help to beat mucus up that the patient can spit it out or swallow, but because there is so much mucus and the cilia are not properly working what is going to happen is that mucus is just going to sit there in the airways, and plug up the airways and cause obstruction to the airways narrowing of the airways that is the problem with this one. The airways are responsible for bringing oxygen into the actual alveoli. O2 is supposed to make it down into the alveoli, but because of this mucus plug very little of oxygen is going to make it down. A lot of it will not make it, and may have to divert to other areas where there are more patent airways. So, one of the big things here is there is not going to be a lot of oxygen. The opposite is that we want to breathe carbon dioxide. So because of that what is going to happen now, the carbon dioxide that we are trying to breathe out is going to get stuck, or trapped, so one of the big things with this that you notice with chronic bronchitis is that we cannot get as much air in oxygen wise, and we cannot get a lot of the air out, but more specifically getting air out that is the big thing. One of the big big things that we are going to see in patients who have this chronic bronchitis is they have what is called air trapping. In general, they get a little bit smaller, so if the patient has already this mucus plug, they are narrowing the airway, and when one tries to exhale the airway gets even smaller, getting that little bit of air out would be too difficult. A lot of that air sits down in these airways, and a lot of it builds up, especially CO2. So the patient gets very little oxygen in, and very little CO2 out, and this causes that classic air trapping.
The patient has low oxygen coming in because of the mucus plug. The mucus build up causes air trapping. On top of that less oxygen is going to be making it into the airway because of the mucus plug, but more significantly, the patient is going to have more CO2 building up, because it exchanges here. Because of the mucus plug occluding the airway, especially during expiration, because as we expire the airways get a little bit smaller, it is going to cause so much CO2 to build up. There are two things, the CO2 is going to start building up in the blood and less oxygen is going to make it down into the airway and profuse into the tissue. This is a V/Q mismatch. This can lead to hypoxemia and another one which is really bad here is hypercapnia. Hypoxemia is the low partial pressure of oxygen, and hypercapnia is the high partial pressure of CO2. This is one of the big common finding we are going to see in patients with chronic bronchitis.
Another thing that we have to think about with chronic bronchitis is it puts people at risk of developing lung infections, especially because of the mucus plugging. There are two bacteria that are commonly seen in patients who have COPD that can actually cause this increased risk of pneumonia, one is called haemophilus influenza, and the other one is called Moraxella catarrhalis. These are the ones that are going to increase the risk of pneumonia, and usually this could be strep pneumonia, or lobar pneumonia. With emphysema, this is mainly a structural issue, and then for chronic bronchitis this is a mucus issue.
The liver releases a specific protein into the blood and this protein is called alpha-1 antitrypsin. It is an antiprotease. Because of that its job is to inhibit the action of elastase. So, if you have your liver producing this in constant amounts what it is going to do is it is going to breakdown this actual elastase and prevent it from being able to cause this damage to the elastic tissue. The inhibition of elastase is going to overcome and the patient is going to have a lot of elastase and they are going to start producing damage.
Bernoulli principle says that when you get air coming out of the lungs it leaves in a high velocity manner. At this juncture the airway inside there should be a low pressure, so because of that high velocity means low pressure in the airway. The elastic fibers do create an outward force and this outward force is going to help to be able to keep the actual airways open even despite the fact that air is moving at a high velocity, and causing a low pressure in the airways. Because of emphysema the person loses the elastic tissue here in the actual small airways, because of that whenever he exhales they are not able to keep the airway open, it collapses. When it collapses air is trapped, and it is not able to go out from the lungs, and because of that overtime, that air starts actually causing kind of dilation and expansion. Because of that the CO2 that you are trying to exhale is going to start building up because it is going to be so narrow. During inhalation you are able to bring air in with emphysema, but it is just not as much. Hypoxemia and hypercapnia are way more common in chronic bronchitis. Hypoxemia and hypercapnia for emphysema is usually a later event. A lot of problems with COPD lies with expiration, because again when we expire those airways get a little bit more narrow especially if there is mucus blocking it, or if you lose the elastic tissue. There is going to be a little bit of oxygen not as much getting into the airway, it can lead to hypoxemia, as well as hypercapnia, and this is usually going to develop later stages. After someone who has had chronic emphysema for a long period of time they are going to develop hypoxemia and hypercapnia to a point where actually it is severe and it can lead to a very very dangerous complication like right side heart failure.
There are three types of emphysema that we generally see, centriacinar emphysema. If these dilated pockets of airways develop in the distal airways it can form another type and that is called panacinar emphysema, and the one that is really bad, which we really are going to watch out for is when it affects the distal alveoli, and the distal alveoli usually are forming near the actual pleural tissue. Because of that this is the one that you got to be careful of because it can actually form little blebs that can rupture and form spontaneous pneumothorax.
There is a big complication that can develop with emphysema and chronic bronchitis and it was related to the hypoxemia and hypercapnia, which are way more common in chronic bronchitis, it can happen in emphysema, but it is usually in the late stages. Because the patient has so much vasoconstriction this is causing the blood pressure to rise so high in the pulmonary arteries. This hypoxemic overtime can lead to pulmonary hypertension. If the pressure in the pulmonary arteries is high, then the right ventricle is going to have to increase its workload. It is going to have to pump and pump against high pressure so they can push the same stroke volume out. Because of that it is going to put so much workload on the right side of the heart that eventually can lead to what is called right ventricular hypertrophy, but then unfortunately, overtime failure, and this what we refer to as cor pulmonale. It is a complication that can develop because of chronic obstructive pulmonary disease.