Chronic Neuropathic Pain

A Little About Me
I am a physicians assistant and currently work in occupational medicine. I have worked in occupational medicine and orthopedics for the last 13 years. In my practice, I treat patients with complex neurological and orthopedic conditions. One of the more severe forms of chronic neuropathic pain is Complex Regional Pain Syndrome (CRPS), which can cause significant emotional and physical disability. In my experience, the patients that I treat know very little about why they have pain and what to expect in the course of their treatment. I am writing this article to help patients who are suffering from chronic neuropathic pain and/or complex regional pain syndrome.
The Diagnosis of Complex Regional Pain Syndrome (CRPS)
Complex Regional Pain Syndrome (CRPS) is formerly known as Reflex Sympathetic Dystrophy (RSD). CRPS can be defined as a chronic pain condition that results in extreme pain and abnormal/heightened sensitivity. This condition often presents initially in one extremity, such as the left leg or the right arm, but can also spread to other extremities as the disease progresses. At this time, there is not one specific known cause for this condition. It usually develops as a result of a conglomeration of several different factors. In my experience, patients who have had a traumatic injury to an extremity and then have surgery or injections to that extremity may go on to develop this condition. However, it doesn't happen in all cases.
In CRPS, it is theorized that damage to the peripheral and/or central nervous system causes the nervous system to malfunction. In general terms, the purpose of a healthy nervous system in an extremity is to allow us to feel something touching our skin and to move our muscles. The nervous system is supposed to alert us to painful sensations, such as a cut, burn, extreme cold, etc., so that we know to take our extremity away from that object. The intention is that when we are alerted to this painful sensation, we move ourselves away from whatever is causing it to prevent significant damage to the extremity. In CRPS, the nervous system starts alerting painful sensations to otherwise benign objects. Instead of feeling a light, soft touch on the skin, patients with CRPS can feel excruciating pain as if they were touching something that was doing significant damage to the extremity. This is called allodynia. Allodynia is defined as pain due to a stimulus that does not usually provoke pain. This symptom is frequently present in patients who have CRPS and can be very debilitating.
Another hallmark (or classic) symptom is hyperalgesia. Hyperalgesia is defined as increased pain from a stimulus that usually provokes pain. Patients with hyperalgesia will have exaggerated amounts of pain with seemingly minor injuries. This symptom can also be very debilitating.
Patients with CRPS can also have changes in skin temperature, skin color, skin texture, sweating, hair patterns (either the absence of hair or excessive growth of hair), nail growth, and swelling. The skin can appear shiny, red or can appear thin, blue, and pale. This is primarily related to abnormalities in the circulation caused by damages to the nerves that control blood flow and temperature in that extremity.
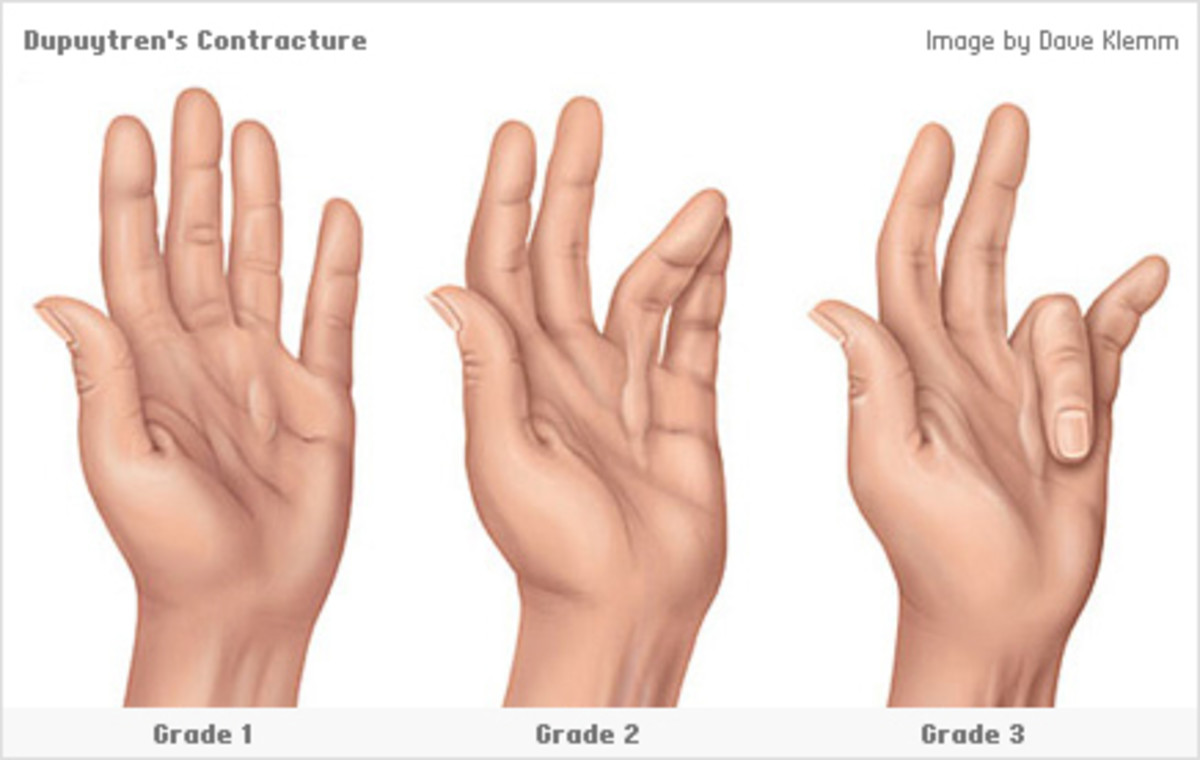
Other potential symptoms include abnormal muscle movements, which can range from very stiff, fixed abnormal postures (called dystonia) to tremors or jerking in the extremity. There can be difficulty controlling the muscle movements in that extremity due to damages to the nerves that control the muscles and this can lead to problems with coordination and paralysis.
Diagnostic Criteria
The diagnosis of Complex Regional Pain Syndrome (CRPS) can be difficult to make. There is not currently a standard diagnostic test that is used to identify for this condition or to differentiate it from other chronic pain conditions. Oftentimes, the diagnosis of CRPS is based on multiple different factors, including physical examination, subjective complaints, response to injections, bone scan, nerve testing, and mode of onset. When diagnosing this condition, it is typically necessary to rule out potential other causes for the symptoms, including Lyme disease, small fiber polyneuropathies, multiple sclerosis, other demyelinating diseases, generalized muscular disease, and clotting in veins.
Several organizations have compiled different diagnostic criteria that are required to be present in order to make the diagnosis. These include the Budapest (Harden) criteria, Veldman criteria, and criteria from the IASP (International Association for the Study of Pain). I typically rely on the Budapest (Harden) criteria to diagnose this condition, as they are the most specific. The IASP criteria were developed in 1994 and the Budapest criteria represent a revision of the original IASP criteria from 1994. There are 2 versions of the Budapest criteria, a diagnostic version that was developed to maximize sensitivity and identify true positive cases, and a research version that was developed to more equally balance specitivity and sensitivity.
The Budapest (Harden) criteria are as follows:
(1) Continuing pain disproportionate to the inciting (initial) event. This literally means that a person has pain that lasts longer than is expected for the particular injury or diagnosis.
(2) 1 symptom from each of the following four categories:
(a) Sensory: hyperesthesia/allodynia. This is the presence of increased pain when you touch the area and the presence of pain with otherwise benign stimuli.
(b) Vasomotor: temperature asymmetry or skin color changes or asymmetry. This means that the affected leg or arm has either a higher or lower temperature compared to the non-affected arm or leg and there are also color changes, such as redness, etc.
(c) Sudomotor/edema: edema or sweating changes or sweating asymmetry. This means that the affected arm or leg is swollen or sweats when the non-affected arm or leg does not.
(d) Motor/trophic: reports of decreased range of motion or motor dysfunction, such as weakness/tremor or dystonia or trophic changes: hair, nail, skin. This means that there is weakness, muscle spasm, absence of hair on the affected extremity, or changes in the skin pattern and color.
(3) At least 1 sign in 2 or more of the following categories:
(a) Sensory: Evidence of hyperalgesia (to pinprick) and/or allodynia (to light touch and/or temperature sensation and/or deep somatic pressure and/or joint movement).
b) Vasomotor: Evidence of temperature asymmetry (>1°C) and/or skin color changes and/or asymmetry.
(c) Sudomotor/Edema: Evidence of edema and/or sweating changes and/or sweating asymmetry.
(d) Motor/Trophic: Evidence of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin).
(4) There is no other diagnosis that better explains the signs and symptoms.
In summary of the above, criteria, it is necessary to see at least some signs and some symptoms of sensory, vasomotor, sudomotor, and motor changes. It is also necessary that there is pain that is disproportionate to the initial event and pain that extends beyond the expected duration of healing. Finally, it is necessary to rule out other potential causes. Patients with CRPS are diagnosed after they have had these symptoms for 6 months or longer, as it is necessary for there to be a chronic component of pain that extends beyond the expected healing time. As noted above, it is this conglomeration of factors that ultimately leads to the diagnosis of CRPS.
DIagnostic Tests
When there is clinical suspicion for this diagnosis, there is a need for confirmation of the diagnosis with a more objective test in most cases. One of the most specific tests for this diagnosis is a sympathetic nerve block/injection. However, only about 1/3 of patients with CRPS will have a good response to this type of injection. A good response to the injection is diagnostic for CRPS, but the absence of a response does not rule out the presence of CRPS. In patients with CRPS, it is expected that they will have significant pain relief from the injection. However, in most cases, the pain relief is temporary and only lasts several hours to several days. As such, this is not an effective treatment for the condition. However, it is extremely efficacious as a diagnostic test.
A bone scan can also be used in the diagnosis of this condition. A bone scan is similar to an x-ray, but it uses contrast to look for uptake in certain areas of your body. In CRPS, there is a pattern of uptake that is characteristic of the condition.
For Research Purposes - please answer the following:
What treatments have you tried for CRPS?
Treatment
There are many available treatments for this condition. It typically takes multiple different treatments used at the same time to get a good control on this condition. Many patients with this diagnosis will need to be treated chronically. However, just like the diagnosis of diabetes, it is possible to effectively manage this condition long term. The following treatments are listed in the order in which they are usually recommended. The treatments listed first are usually the ones that are tried just after the diagnosis is made followed by the treatments towards the bottom of this section is pain relief is inadequate with the first line treatments.
Medications
The most commonly used medications for this condition include NSAIDs (Motrin, Naproxen, Ibuprofen, Advil); neuropathic pain medications (Lyrica, Neurontin); tricyclic/SNRI anti-depressants (amitriptyline, nortriptyline, duloxetine); NMDA receptor antagonists (ketamine, amantadine), and alpha 1 adrenoceptor blocking agents (terazosin, prazocin).
Oftentimes, a combination of the above medications is necessary to treat the condition.
Physical Therapy/Exercise
A program of physical therapy is necessary with a therapist that is specifically trained in this condition. Treatment with a therapist that is not trained in CRPS can be devastating and can actually exacerbate the condition. After a course of therapy, the therapist educates the patient in an exercise program that can be performed at home on a regular basis. Regular participation in an active exercise program can be a quite effective treatment for this condition.
Psychological Treatment
Psychological treatment is focused on improving the patient's quality of life. Psychological sessions for a patient with CRPS focus on developing coping skills to deal with the chronic pain condition. Cognitive behavioral therapy is a specific type of psychotherapy that is commonly used in the treatment of this condition. Additionally, many patients who have CRPS also have comorbid psychological diagnoses, including anxiety or depression. These can also be treated with outpatient psychotherapy.
Pain management
Generally, patients with CRPS are treated on a long-term basis with a pain management physician. This doctor can provide medications and recommend other treatment options. It is very important that a person with CRPS maintain a good therapeutic alliance with his treating physician to optimize the potential therapeutic benefit.
Spinal Cord Stimulation
A spinal cord stimulator (SCS) is a type of electrical stimulation unit that is surgically implanted into your spine and provides stimulation to the nerves. An SCS is a rather effective treatment for this condition in most cases. However, they are only considered after all reasonable non-operative treatments have failed and are considered to be a last line treatment.
© 2015 Kortney T