Management of Diabetes Mellitus (dm)

Clinical Features of Diabetes
signs and symptoms
Signs of diabetes include pronounced and progressive weight loss, frequent urination, and increased thirst known as Polydipsia. Diabetic individuals usually have intense hunger. In type I diabetes, the symptoms are noted after a very short period of time unlike type II where the symptoms can be obscure and mild. Other symptoms like blurred vision and skin rashes can also occur.
Some individuals with highly responsive systems can have pronounced symptoms like Diabetic Ketoacidosis which is a metabolic disorder leading to production of ketones into the blood system. These individuals usually have the acetone smell and breaths with other symptoms like nausea, vomiting, abdominal pain and altered states of consciousness.
Classification of Dm
Type I Diabetes Mellitus
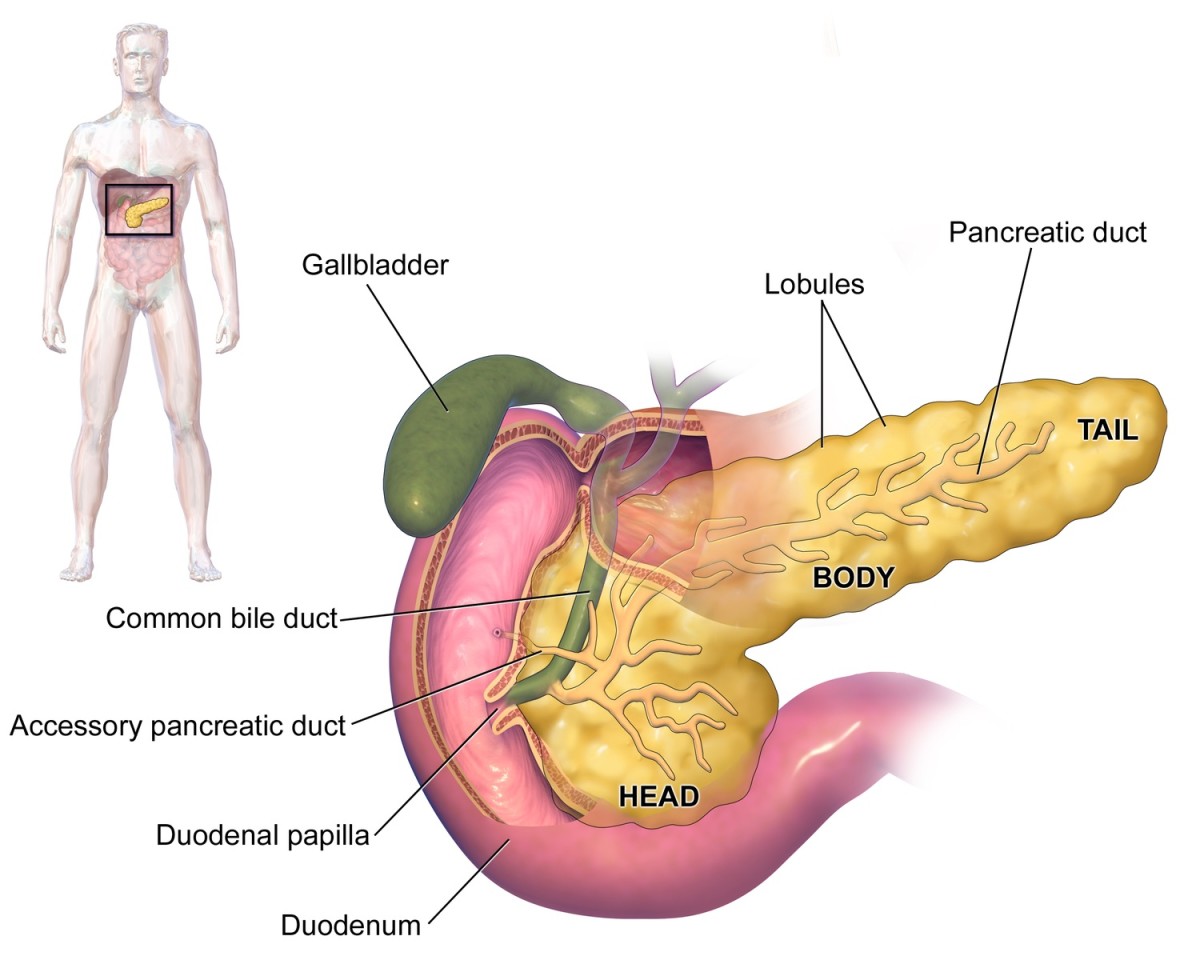
This condition results from a metabolic failure. The condition is seen when the pancreas fails to produce hormone insulin.
Type II Diabetes Mellitus
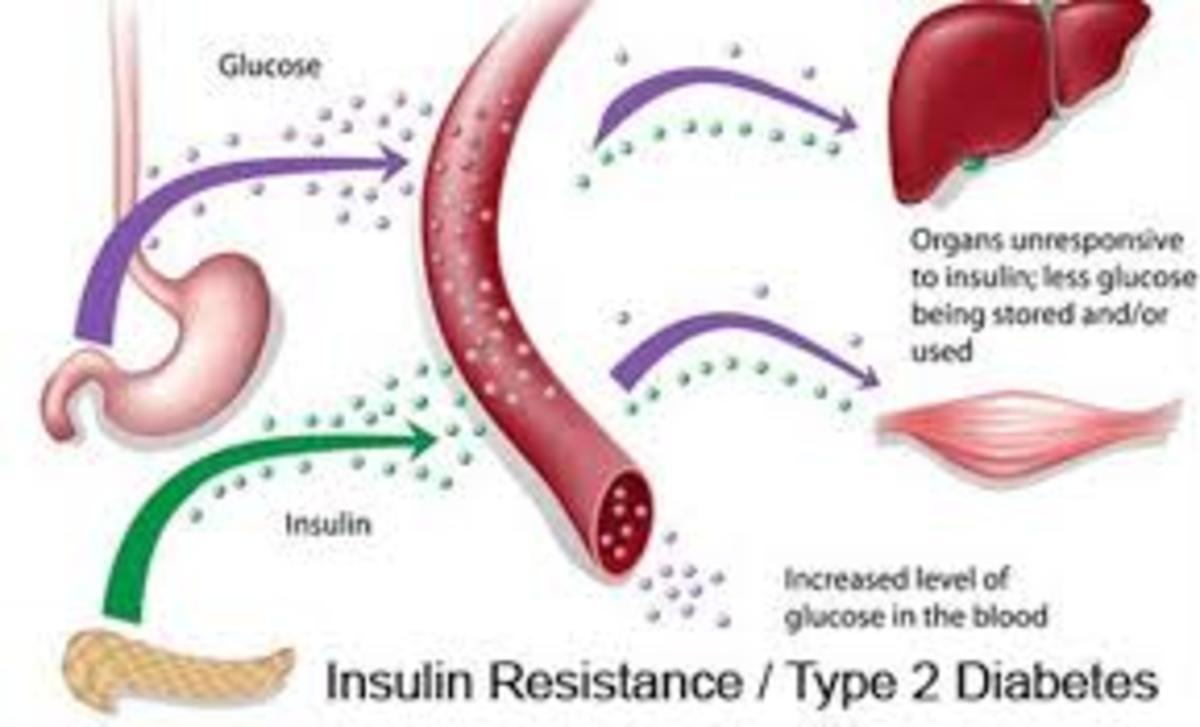
Results from the inability of the body cells to recognize and use the insulin properly. The condition is developed when the pancreatic function is normal; however, the cells that use up insulin fail to utilize the insulin hormone to control the blood sugar levels
Gestational Diabetes
Usually present in pregnant women; developed due to the effects of pregnancy.
Causes / Etiology and Risk Factors of Dm
Causes
Diabetes types are differently developed. Type I diabetes can be inherited; however, it can also be triggered by a viral infection. The virus responsible for the condition is known as the Coxsackie B4 virus. Despite the inheritance of the genetic susceptibility, diabetes mellitus type I must have an environmental triggering factor.
Type II diabetes is fairly due to genetics and lifestyle factors. Any form of defect on the hormone insulin results into a specific type of diabetes. Diabetes is dependent on insulin factors. After digestion of food has been done, incorporation of energy inform of sugar is done. Sugar is absorbed into the blood stream for energy provision purposes. In response to the high sugar levels, the pancreas releases insulin hormone into the blood stream to control the blood sugar levels to normal. In the event of low sugar levels, the pancreas produces glucagon hormone which reduces the amount of glucose in the blood stream.
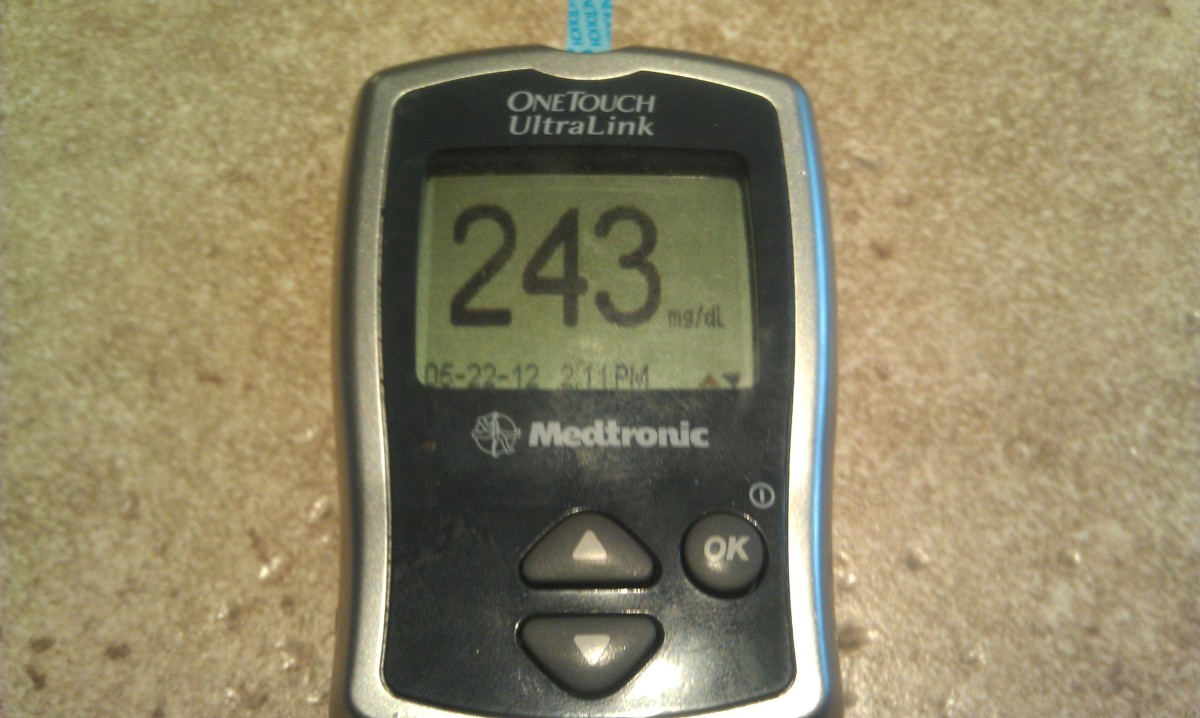
Insulin is responsible for the build up reactions in the body; however, diabetes can reduce the amount of insulin that the pancreas produces. Lack of insulin leads to break down of the cells leading to pronounced weight loss. When a person develops diabetes, the blood glucose becomes elevated beyond 10mmol/L. This facilitates the reabsorption of water into the renal tubules leading to increased urination and thirst. Moreover, much glucose is passed in the urine making the body cells deficient of glucose and energy.
Risk factors
Risk factors of diabetes type I include genetic factors and the environmental triggers. Substances that are known for damaging the pancreatic cells can possibly lead to diabetes. Additionally, certain viral infections can lead to diabetic conditions. Individuals should take precautions especially when there is history of diabetes in families
Diet is a major contributing risk factor. Early exposure of infants to cow milk and cereals at ages below four months has been proven to cause type I DM. Other dietary influences include diets with low vitamin D. Diabetes type I is also common in whites than other races.
Type II diabetes is associated with many risk factors. Fat (increased weight) is associated with insulin resistance. Obesity and inactivity reduces the reception to insulin by the cells thus leading to type II DM. Other factors like old age, race (blacks- African-Americans, Asians, Hispanics and Indians) are highly affected. Family history of diabetes is also an important factor in type II DM. Gestational Diabetes is associated with old age (women over 25 years), family history or previous personal history of diabetes. Increased weight and race (Blacks, Hispanics, American Indian and the Asians) also contribute largely to gestational Diabetes mellitus.
Management of Diabetes
DM is a condition that has no cure but can be properly managed. The management aims at keeping the blood sugar levels to normal. Management can be done through dieting, medication and exercise. Lifestyle modification is an important factor in controlling the condition. Exercise reduces the weight to reasonable levels which ultimately increases the functionality of the body cells. Dietary modification will also ensure reasonable amount of sugar in the blood stream.
Medication involves using a wide range of regimen to lower or raise the blood glucose to normal levels. Metformin regimen is usually used as the medication of choice. Insulin therapy is widely used as well. Insulin is usuallyinjected intravenously to increase its efficacy. However, patient education on prevention is important in managing diabetes mellitus. Patients should absolutely avoid risk factors and dangers in DM.