Definition of Ocular Hypertension

About the Author
Melissa Flagg is an ophthalmic technician and has been examining patients on a daily basis for over 20 years.
She has had rigorous training under the supervision of an ophthalmologist and specialized in the cornea, cataracts, and retina as well as how systemic disease affects the eye. She has been certified by JCAHPO as a Certified Ophthalmic Assistant.
Many people confuse glaucoma with ocular hypertension. However, the two conditions are actually quite different. Although the pressure of the eye is elevated in both conditions, glaucoma actually damages the vision, whereas ocular hypertension does not.
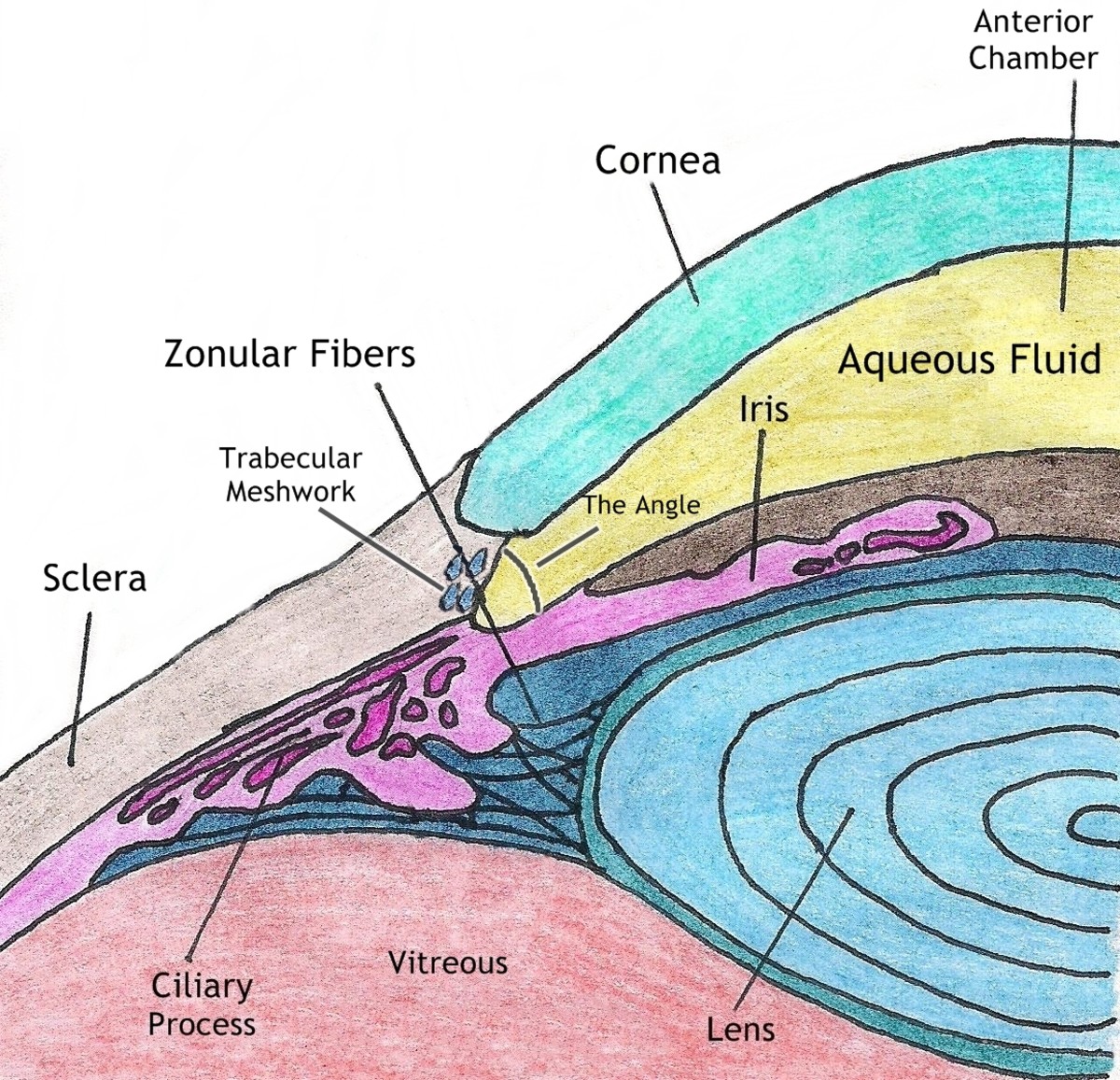
Intraocular pressure, or the pressure inside the eyeball, gives the eye its rigidity and shape. It is the result of the aqueous fluid found in the anterior chamber of the eye, which is constantly produced by the ciliary process located behind the iris. The aqueous drains through a system of ducts called the trabecular meshwork.
With glaucoma, either the eye produces too much aqueous, or the trabecular meshwork doesn’t allow enough aqueous to drain through to maintain a normal pressure in the eye.
Patients with ocular hypertension could also be called glaucoma suspects. They do not have any visual field loss or damage to the optic nerve, but because of the elevated pressure in their eyes, the ophthalmologist is concerned they may eventually develop glaucoma.
Corneal Thickness and The Ocular Hypertension Study
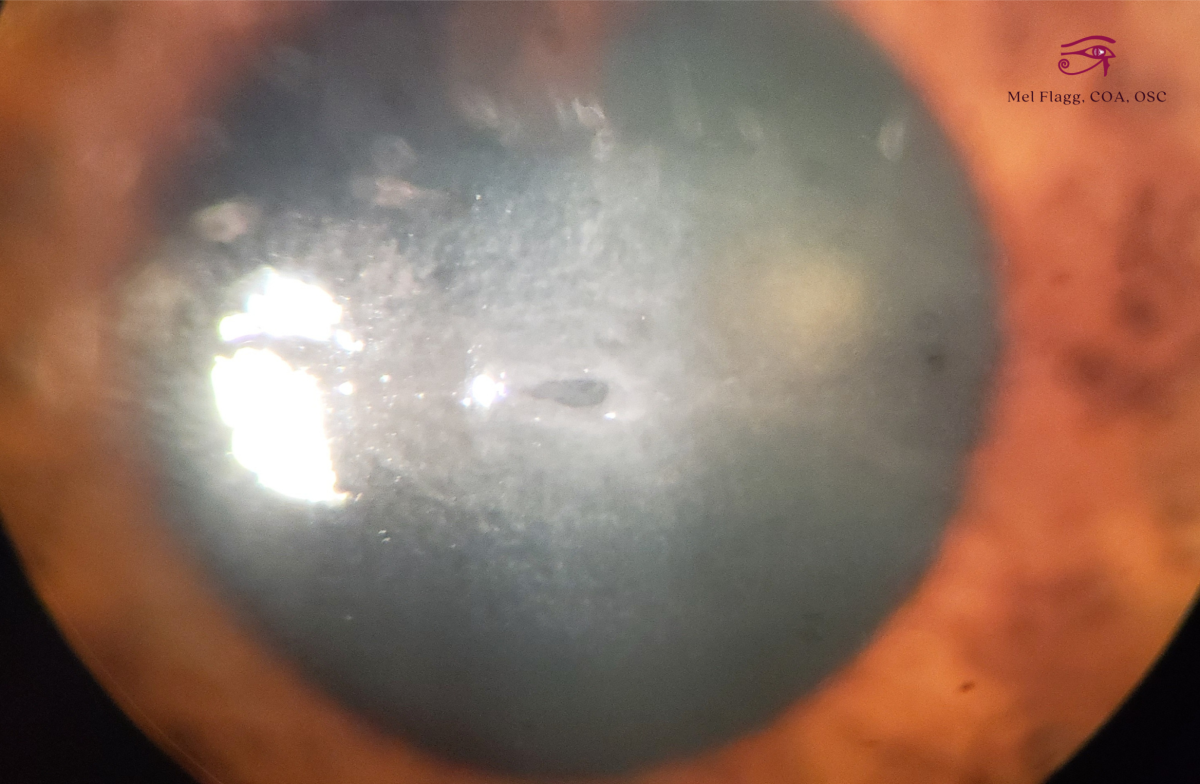
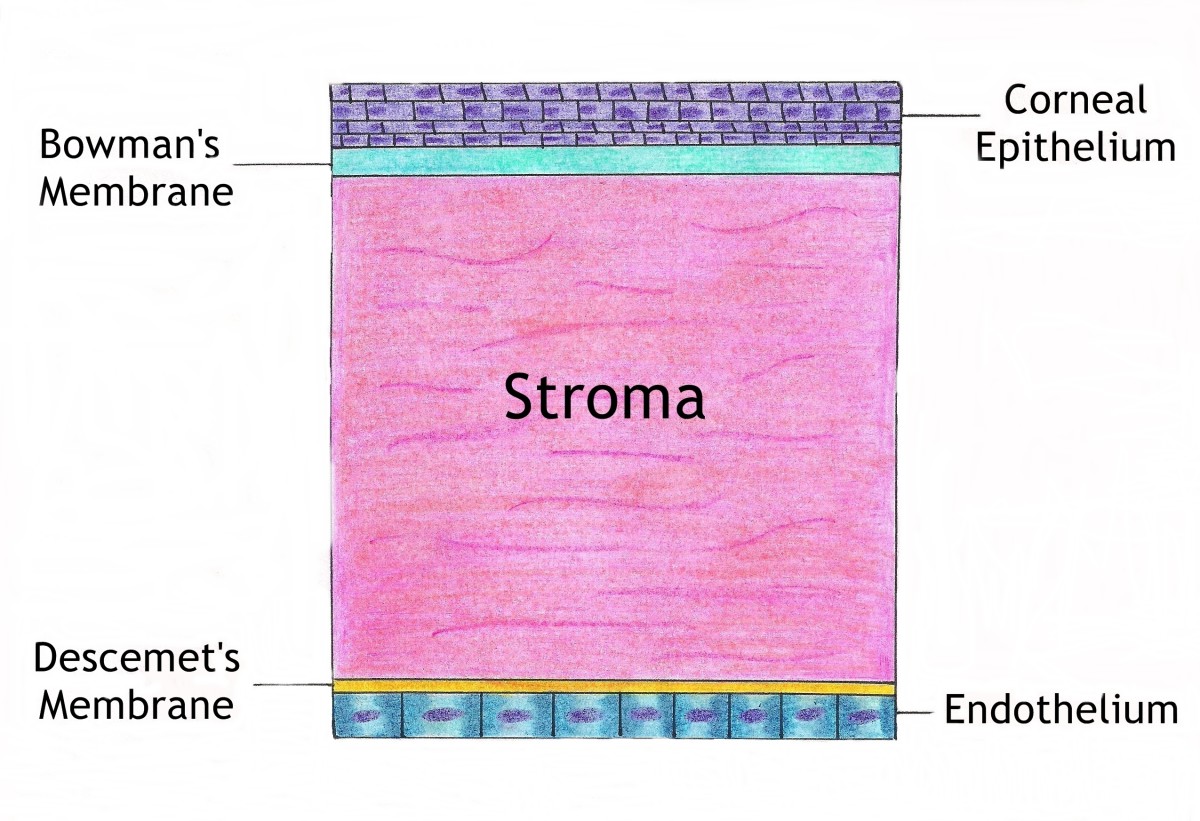
The cornea is essentially the window through which we see. It gives us 70 percent of our focusing power, and it is comprised of five layers:
- The Epithelium - the first layer of the cornea and the most likely to be injured.
- Bowman’s Membrane - the function of this second layer of the cornea is unclear. It is acellular and is made up of primarily collagen fibrils.
- The Stroma – the third and thickest layer of the cornea. This layer gives the cornea its shape and stability and is the main culprit in ocular hypertension. The stroma does not regenerate, and because of this, it is the target of LASIK surgery.
- Descemet’s Membrane – this fourth layer is very elastic because it is made up of type III collagen. If cut, this layer will retract. It has no regenerative properties.
- The Endothelium – the last layer of the cornea maintains corneal deturgescence (relative dehydration that maintains corneal clarity) and is comprised of about 500,000 cells.
Layers of the Cornea
In 2002, the result of a study known as the Ocular Hypertension Study (OHTS) was released. This study was a huge breakthrough because it revealed that the thickness of an individual’s cornea could alter their intraocular pressure (IOP). This information led to a rise in a procedure known as pachymetry, which measures the thickness of the cornea.
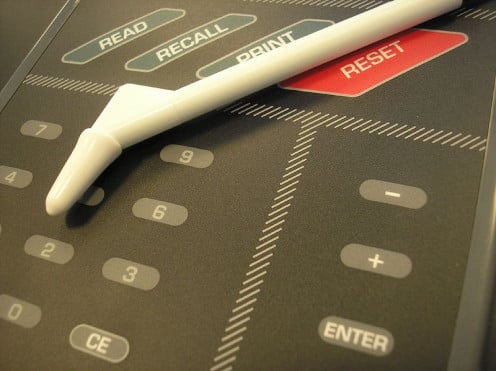
To perform pachymetry, the doctor or technician uses a device called a pachymeter, which uses either ultrasonic or optical methods to measure the corneal thickness.
The Pachymeter
For most people, corneal thickness is approximately 540nm or about half a millimeter. However, patients who are extremely nearsighted may have a corneal thickness of 590nm or more.
In patients who have had refractive surgery, the corneal measurements are typically very thin. For example, a patient who has had LASIK may have had a corneal thickness of 545 prior to surgery, but after the procedure, their corneal thickness may be 445nm.
Corneal thickness can alter IOP readings in one of two ways:
- A thin cornea could result in a lower IOP, which could hide the fact that the patient actually has glaucoma.
- A thick cornea could result in a higher IOP, which could cause a patient to be treated for a disease they don’t have.
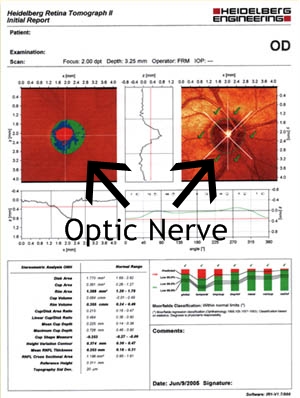
Heidelberg Retinal Tomography
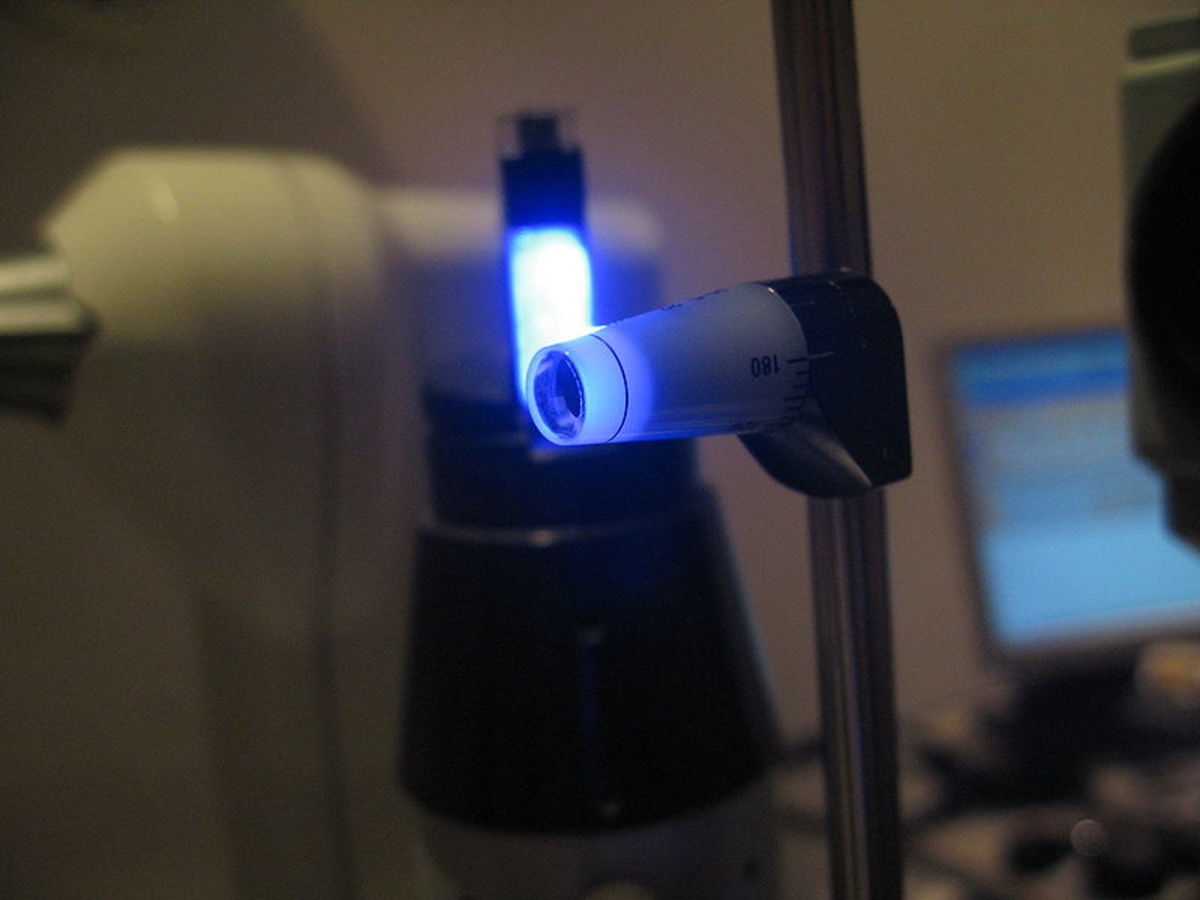
Goldman Applanation
Testing for Ocular Hypertension
The tests ordered for ocular hypertension are generally the same tests ordered for patients with glaucoma. These include:
- Pachymetry
- IOP testing
- Visual Field Analysis
- Optical Coherence Tomography (OCT)
- Heidelberg Retinal Tomography (HRT)
- Measurement of the cup-to-disc ratio
Tonometry
The most common test for glaucoma, however, is actually the pressure check, or measurement of intraocular pressure or IOP. This test is done at every exam, and sometimes patients come in just to have their IOP checked.
The procedure used to check the pressure is known as tonometry, and the device used is called a tonometer. There are several different methods of performing tonometry:
- Goldman Applanation
- Tonopen
- Non-Contact (NCT) Tonometer
- Shiotz Tonometer
The most accurate of these methods is by far the Goldman applanation method.It's also the most widely used by ophthalmologists.
The tonopen is predominantly used on patients who can’t undergo applanation because of corneal issues, such as a corneal abrasion or scratch.
The NCT tonometer, most commonly called the “air puff” test, is predominantly used by optometrists.
The Schiotz method is hardly used anymore; however, in its day, the Schiotz Tonometer was the most accurate way to check a pressure. Below is a video explaining how the Schiotz Tonometer works, and the basic principle behind testing the intraocular pressure in general.
The Schiotz Tonometer
Visual Field Testing

Optical Coherence Tomography
Visual Field Testing
Visual field analysis is a test of the patient’s peripheral, or side, vision.
The patient places their head in a machine that flashes lights in various places in the periphery of the patient’s vision. Every time the patient sees the light, they click the hand held button.
The result is a map of the patient’s retina that tells the doctor where peripheral vision has been lost. This is an invaluable way to not only diagnose, but also monitor glaucoma.
Heidelberg Retinal Tomography and Optical Coherence Tomography
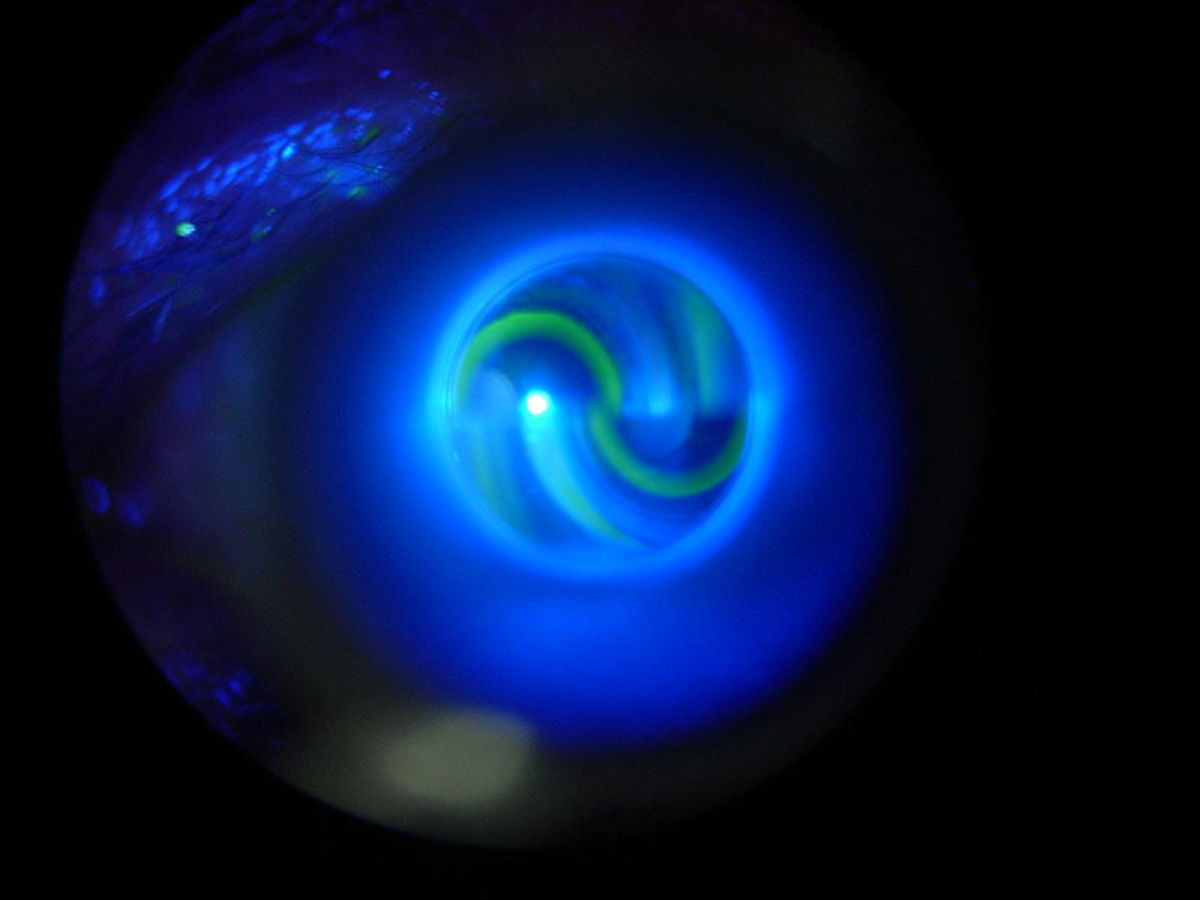
Heidelberg Retinal Tomography (HRT) scans the optic nerve and renders a 3D representation of it, which allows the ophthalmologist to see exactly what the optic nerve looks like.
Any damage sustained from abnormal pressure in the eye becomes very apparent with an HRT, and the changes that occur over time can more accurately be monitored.
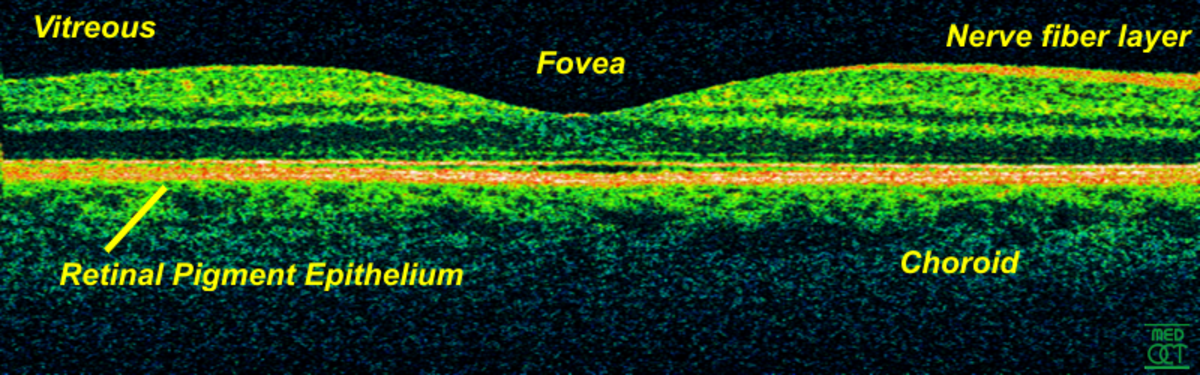
The same is true with Optical Coherence Tomography (OCT); however, with OCT the image is not 3D. The OCT image provided (see photo) allows the doctor to see all the different layers of the retina, or in the case of glaucoma, the optic nerve.
The Cup-to-Disc Ratio
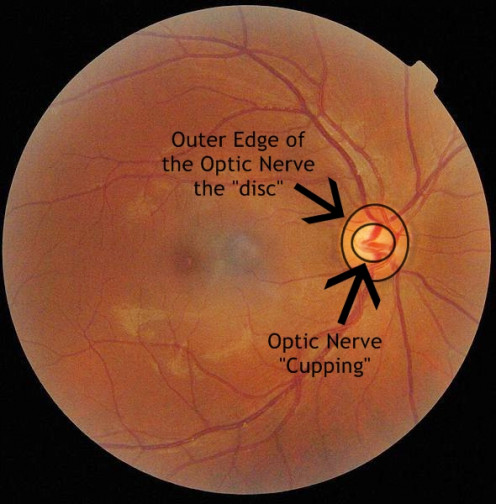
Measurement of the cup-to-disc ratio is done at every dilated exam, and sometimes when a patient simply comes in for a pressure test. It is a visual measurement of the damage caused to the optic nerve from glaucoma. When the pressure in the eye rises, it forces the optic nerve to “cup.” This creates a bowl-like appearance to the optic nerve, which results in the loss of peripheral vision.
To understand the “cup-to-disc” think of the optic nerve as a doughnut, the center hole would be the cupping created by the increased pressure, and the doughnut would be the rim of the optic nerve. The size of the doughnut hole grows as the pressure in the eye rises, which leads to permanent vision loss. The photo below may help you visualize the cup-to-disc ratio.
The Cup-to-Disc Ratio
Treatment for Ocular Hypertension
There really isn’t any treatment for ocular hypertension, unless it advances to glaucoma. If this happens, there are a number of medications as well as surgical options for treatment. The most important thing to remember about ocular hypertension is keep your appointments with your eye doctor. This condition needs to be monitored.
Every six months (sometimes every three months) is the normal frequency of office visits for most patients. This is so that should the ocular hypertension advance to glaucoma it can be caught right away, minimizing the damage that can be done.
© Copyright 2012 - 2015 by Melissa "Daughter of Maat" Flagg ALL RIGHTS RESERVED