The Link Between Chronic Pain and Depression
Is There a Relationship Between Depression and Pain?
Through the Eyes of a Nurse
Every hospital nurse has seen it at one time or another. The scene of a patient complaining of pain and requesting pain medication, only to be found asleep when you enter the room. Or maybe you have a patient who doesn’t complain of pain and in fact doesn’t talk much at all, has a flat effect or is even tearful and has difficulty with movement but doesn’t express any requests or explanation for their appearance. As a nurse, being all about assessment of the patient and situation, you would probably ask yourself, “Is this patient really in pain or is it depression that is making him feel and act this way?” Would you go a little further to consider that it could be both depression and pain at the same time?

Defining Depression
According to Walker and Avant (2005), to define a concept all available uses of the concept are used to define its’ meaning. Then consider the purpose of your analysis to determine the uses that will be necessary for inclusion to your concept analysis (p.67). The definitions of depression and pain from Encarta Online Dictionary and Encyclopedia were used in addition to an extensive literature review. Literature included for review for this paper are retrieved from the following websites and sources: Mayo Clinic, WebMD, Clinical Psychiatry News, Pain Management Nursing, Harvard Health Publications, Spine-Health.com, The Johns Hopkins Arthritis Center, Rockhawk.com, Taber’s Cyclopedic Medical Dictionary, Concernedcounseling.com, Psychosomaticmedicine.org, Painaction.com and The Cleveland Clinic.
Depression is defined by Encarta Online Encyclopedia as a feeling of deep unshakable sadness and decreased interest in most former activities. Everyone experiences these feelings from time to time. When these feelings last longer than a few days or weeks is known as clinical depression and is the form that will be discussed in this paper. It is the most prevalent mental condition and effect 8% of adult in the United States at one time or another. Symptoms of depression include change in eating habits, sleeping habits, social withdrawal, complaints of physical ailments, lethargy, irritability and decreased interest in former activities. Taber’s defines depression as a mood disorder characterized by loss of interest or pleasure in living and exhibits symptoms of sadness, hopelessness or tearfulness, loss of energy, irritability, inability to concentrate, decrease in daily activities, change in appetite or body weight, change in sleep habits, persistent feelings of guilt, a sense of worthlessness and recurrent thoughts of death or suicide.
The Pain Phenomenon
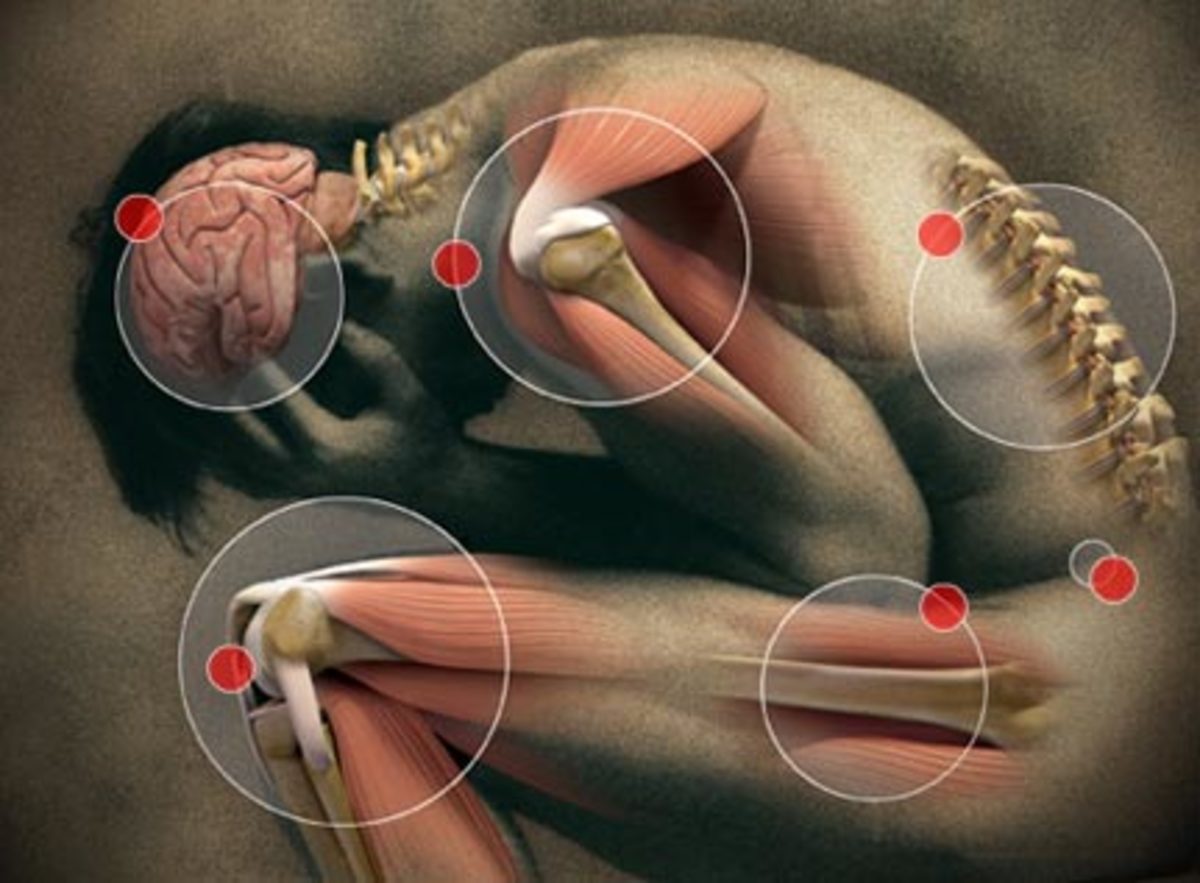
In comparison, there is another phenomenon that is experienced by everyone at one time or another: pain. Encarta states that pain is an unpleasant experience that may be received by sensory or emotional means caused by real or perceived threat to personal injury or harm. Taber’s states that pain, in addition to the above definition, includes not just the perception of uncomfortable stimuli but the response to that perception. Pain can be present in nearly any organ system with different characteristics in each system. Taber’s goes on to say that there are several factors that can influence the pain experience. Some of these factors include but are not limited to; the nature of illness or injury, physical and emotional well-being of the patient, how acute or chronic the symptoms are, the social or cultural status of the patient, memory and personality among others
Symptoms Common between Depression & Chronic Pain
Both conditions can exhibit similar traits such as lack of energy, change in sleep habits, appetite and mood. Knowing these facts presents even more questions such as, “Could one condition bring about the other?” “Does depression cause pain or does pain cause depression?” “Could both conditions occur at the same time?” and “Are the two concepts related or totally unrelated?” As nurses, it is vital that we explore the true meanings of depression and pain, the relationship between the two concepts and how they affect our patients. By gaining a clear perspective into these phenomenon, healthcare providers can then better assist their patients in effectively recognizing depression as well as unrealized effect of pain when dealing with depression and pain. In this article I will attempt to explain possible connections of depression and pain as the two concepts are explored in more depth. Kolcaba’s Theory of Comfort will be used to analyze this concept exploration.

The Research
The next step to concept analysis after defining the concept is to define its attributes. This step is the main goal of concept analysis and determines the characteristics that are most common of the concept and provide a broad view into its meaning. Defining attributes are not absolute or indisputable and may change as concept understanding improves. They may also change as the concept changes or as the concept is used in a different context (Walker & Avant, 2005, p. 68). Articles, research studies and websites were used for research to discover the most common attributes of both phenomenon of depression and pain.
After review of the literature several characteristics about the concept of depression have been made known. These characteristics include sadness for most of the day, nearly everyday, change in appetite, change in sleep, change in weight, agitation, restlessness, fatigue, feeling of worthlessness, inability to concentrate and possible thoughts of suicide or death (painaction.com, 2008). Depression is one of the most common health problems healthcare providers face and is four times more likely to be present in people with chronic pain than the general population (spine-health.com, 2004).
Pain also presents itself in varies different ways as evidences by the review of literature available. I previously noted in my concept analysis of pain that, although pain may be present in many different disease processes, it usually is facilitated through a similar pathway it each case. No characteristics of pain are certain for any particular condition or disease or for any individual. A specific pathway is usually responsible for several different symptoms and patient can have more than one route for producing pain sensations which may even change over time. This pathway is a result of impulses that travel along pathways of the nervous system where sensation is processed. Based on the previous definitions and the research of information I have found, I believe that the significant factors of the pain concept are universality of experience, physiological mechanisms, subjectiveness and individuality of experience, provocation of anxiety, experience that involves internal and external aspects as well as the instinctive withdrawal from painful stimulus (whether perceived or actual). According to my research and personal experience, I would define the concept of pain as a universal yet individual experience. It is an occurrence of discomfort based on actual or perceived threat of harm to one’s physical, mental or emotional well-being. The perception and description of pain is extremely personal and individual due to the fact that the discomfort felt by one person cannot be shared with another person.
In a literature review of possible connections between the phenomenon’s of depression and pain interesting insight was revealed. According to the American Psychosomatic Society pain perception is high in individuals that suffer from depression than the general population. The society performed a search of to find studies that compared psychophysical responses to painful stimuli in those with depression versus people who did not suffer from the condition. Six independent studies were found and all provided results showing that depressed persons had a higher pain perception threshold than non-depressed persons (psychosomaticmedicine.org).
In an article for Pain Management Nursing France, Krishnan and Trainor wrote of a study they conducted in an attempt to shed light on the relationship between chronic pain and depression. In this study they looked at the prevalence of depression and chronic pain in first-degree relatives of 100 patients with chronic pain. It was noted that those with close relative with depression had a higher incidence of depression themselves. This result suggests the possibility that major depression observed in chronic pain patients might be the effect of a genetic predisposition to depression for these people. HealthyPlace Chronic Pain Community published an article stating that depression can worsen back pain and conversely, back pain can lead to major depression. The article goes on to say that depression and chronic pain are the two most common health concerns that healthcare providers face but only a small number of research studies have been done to reveal the connection between the two phenomenon in the general population. The research that has been done shows that depression is nearly four times greater in individuals with chronic pain than those without chronic pain. Findings also suggest that the rate of depression is increased in relation to increases in pain severity. In 2007 Spine-health.com confirmed these findings with their own study that indicated that 61% of people with chronic back pain also suffered from depression. More recent studies are beginning to probe into the possibility that depression and anxiety may play a role in the onset of back pain (concernedcounseling.com). There were 252 chronic pain patients responded to a questionnaire presented by University of Iowa researchers. Out of that group of patients, two-thirds were diagnosed with depression of which 68% admitted that the depression came first. In additions to these findings, 34% of the patients that had not been diagnosed with depression scored an 8 or higher on the Beck Depression scale (clinicalpsychiatrynews.com).
The John Hopkins Arthritis Center published research finding that physical symptoms are common in persons suffering from depression. Moderate to severely depressed patients were more likely to express complaints of headaches, chest pain and chronic muscle pain. The center also conducted a study of first-degree relatives of depressed patients to find that those with chronic pain had more first-degree relatives with depression and depressive disorders. Due to these results it was determined that depression in not considered to be a co-morbidity of pain. In fact, depression has been found to interact with chronic pain, increasing mortality and morbidity (Hopkins-arthritis.org).
Harvard Medical School conducted studies that show a relationship the effects pain and depression have on each other. It was found that the presence of pain increases recovery time from depression and depression decreases the effectiveness of pain treatment therapy. In many rehabilitation centers the two conditions are treated simultaneously, usually with the methods. These methods include meditations, hypnosis and progressive muscle relaxation. Physicians prescribe medications such as aspirin, acetaminophen, nonsterodial anti-inflammatory drugs, opiates and psychiatric drugs. Exercise is used by physical therapists to increase mobility, which can promote onset of new pain or exacerbate chronic pain. The results of the Harvard University study show influences from psychology, neurology and hormones that connect depression and pain (health.harvard.edu).
The Cleveland Clinic published research that indicates that depression can be worsened by pain as pain can also be worsened by depression. A comparison was made of individuals who have no depression to those with a major case of the condition. Those with major depression have more than double the likelihood of chronically painful physical conditions. The article continues by stating that antidepressants can be used to treat chemical imbalances that cause depression and may also help decrease the intensity of pain that is felt physically (clevelandclinic.org).
The Connection
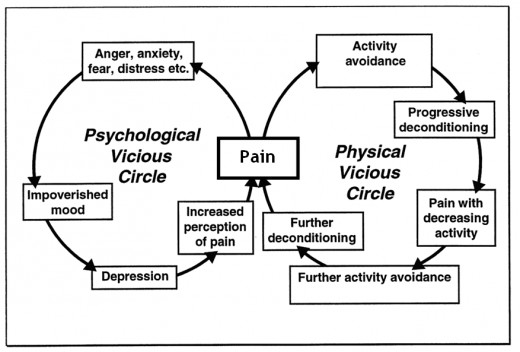
As I continued the review of available literature on depression and pain, the connection between the two has become evident. Now that a connection of the two concepts has been established researchers must know determine whether depression is the cause for chronic pain or is chronic pain the cause of depression. According to rockhawk.com there is evidence to support that both may be true. This site published the results of an analysis of information gathered by the World Health Organization which said that 22% of primary care patients presented with persistent pain lasting 6 months or longer along with a disability due to the pain in which they received medical treatment. Patients with persistent pain also experienced anxiety or symptoms of depression 4 times as much as those without persistent pain (clevelandclinic.org). Research results printed in a Mayo Clinic article reveals that depression and pain work along similar circuitry through the limbic area of the brain, which is the center for emotion (mayoclinic.com). Further information regarding this link is found in an article by Salynn Boyles of WebMD of a study conducted on the characteristics of this common pathway. According to Boyles the neurotransmitters serotonin and norepinephrine that have significant effects on depression are the same ones that promote pain. The article also indicates that because determinating which condition was the cause of the other may be impossible the cycle is viewed as a “depression-pain syndrome”. Therefore, ways of coping with both conditions simultaneously should be sought (webmd.com)
Theory
THEORETICAL CONTEXT
Among the different theories that have been discussed throughout this semester the one I have chosen as the basis for research into the possible relationship between depression and pain is Kolcaba’s Theory of Comfort. This model was chosen due to the fact that it addresses the aspects of life that are basic to all humans including the need of relief, ease and the action of moving beyond stress causing healthcare situations (Kolcaba, 1994, cited in McEwen & Wills, 2007). Depression and pain are both experiences that evoke a strong need for relief. Depression has characteristics such as change in sleep and eating habits, lethargy and according to recent research, somatic pain in various parts of the body. Changes in sleep and lethargy can promote decreased mobility, which in turn can cause pain or increase present somatic pain. Pain that is chronic and not relieved can disrupt activities of daily living therefore causing depression to develop and the need for relief in order for comfort to be restored. Recent studies also reveal that depression and pain work along the same pathways in the brain, which could explain why many characteristics of each concept are very similar. Kolcaba explains that comfort is presented in three different types.
Comfort Types
Type
| Definition
|
|---|---|
Relief
| state of being after a need is met
|
Ease
| calm, content state of being
|
Transcendence
| state when person rises above situation of stress
|
Areas of Context for Comfort Types
Type
| Definition
|
|---|---|
Physical
| sensation experienced in the body
|
Psychospiritual
| inner awareness of self
|
Environment
| external surroundings
|
Social
| interpersonal, family and social relationships
|
Impression
When viewing these different types of comfort and the context in which they can be experienced along with the characteristics of depression and pain, the connection between the concepts of depression and pain become more evident. According to Kolcaba, the role of the nurse in the comfort care of a patient involves the deliberate evaluation of the needs for comfort, plan and implementation of measures to provide that comfort and reevaluation of comfort level after measures have been accomplished. Assessments may be subjective, objective, intuitive or a combination of all three (Kolcaba, 2001, cited in Tomey & Alligood, 2006).
Conclusion
CONCLUSION
The primary goal of a healthcare provider is to assess comfort levels and factors that affect comfort, then develop, implement and reevaluate a plan of treatment to provide optimum comfort. In order to make an accurate assessment, the healthcare provider must realize that comfort or lack of is experienced physically, mentally and emotionally. Acknowledging this fact makes it clear that depression and pain are both very real threats to the comfort of an individual. The fact that many characteristics are similar to both concepts and both are believed to follow the same chemical pathways in the brain, many of the same methods used to promote relief and ease for one concept would be beneficial to the other as well. Educating patients regarding the relationship between depression and pain would increase awareness and understanding for suggested treatments that could ease suffering with both conditions. Kolcaba’s Theory of Comfort contains a framework that is exceptional for explaining the relationship between depression and pain.
A Common Phenomenon
Leave Feedback
Use the buttons below (thumbs up/down section) to leave feedback on what you thought about this article. Thanks for reading!
References
References
Boyles, S. (2004). Study Links Depression and Pain. Retrieved March 4, 2008 from http://www.webmd.com/depression/news/20040826/study-links-depression-pain?print=true
Clark, M.,M.D., M.P.H. (n.d.). Managing Chronic Pain, Depression and Antidepressants: Issues & Relationships. Retrieved March 31, 2008 from http://www.hopkins-arthritis.org/patient-corner/disease-management/depression.html
Deardorff, W.W. PhD, ABPP. (2004). Clinical Depression and Back Pain.
Dickens, C. PhD., McGowan, L. PhD, Dale, S. M.B.B.S., (2003). Impact of Depression on Experimental Pain Perception: A Systematic Review of the Literature with Meta-Analysis. Retrieved March 4, 2008 from http://www.psychosomaticmedicine.org/cgi/content/full/65/3/369
France, R.D., Krishnan, K.R., Trainor, M. (1986). Chronic pain and depression. III. Family history study of depression and alcoholism in chronic low back pain patients. Pain 1986; 24:185-90.
Harvard Health Publications (2004). Depression and pain.
HealthyPlace (2007). Low Back Pain, Chronic Pain and Depression. Retrieved March 31, 2008
MacReady, N. (2002). Depression May Bed Casusal Factor in the Development Of Chronic Pain. Clinical Psychiatric News 30:10, p. 68. Retrieved March 3, 2008 from http://www.clinicalpsychiatricnews.com/article/S0270-6644(02)7011…terms2=&terms2=&terms2=&terms3=&terms3=&terms3=&terms3=&terms3=
Mayo Clinic (2006). Pain and depression: Are they linked? Retrieved March 4, 2008 from http://www.mayoclinic.com/print/pain-an-depression/AN01449/METHOD=print
McEwen, M. & Wills, E.M. (2007). Theoretical Basis for Nursing (2nd ed.)
Medscape (2002). Chronic Pain and Depression. Retrieved March 4, 2008 from http://www.rockhawk.com/chronic_pain_and_depression.htm
Tomey, A. M., & Alligood, M. R., (2006). Nursing Theorists and Their Work (6th ed.). St. Louis, MO: Mosby
© 2012 Shawn Holmes