Psychoeducation: Depression and Major Depression
Depression and Major Depression
by Terri Mackinnon
Many people will be surprised when they find out that I have suffered major depression for most of my life. Although there are many types of depression, they are usually distinguished between depression and major depression.
By the time I had reached my early twenties I had suffered at least three episodes of depression. Over the next thirty years I had multiple breakdowns and was diagnosed with SAD (Seasonal Affective Disorder).I had been treated for it with medications and most of the time it seemed successful at least until the next occurance.
Each episode seemed to get longer and more difficult to deal with. In 2003 it lasted for a three month period and I found that it strange that it had started in the summer, questioning the SAD theory that I had been given.
In the summer of 2006 the depression returned again this time the episode was not going to go away and again was during the summer months. I started seeking answers to what was going on. How could I have SAD when I seemed to start these occurances during the sunny days. The medical professionals decided to go back into my file and re-examine there diagnosis. They realized that I actually had been suffereing major depression bi-polar disease and we began a treatment program.
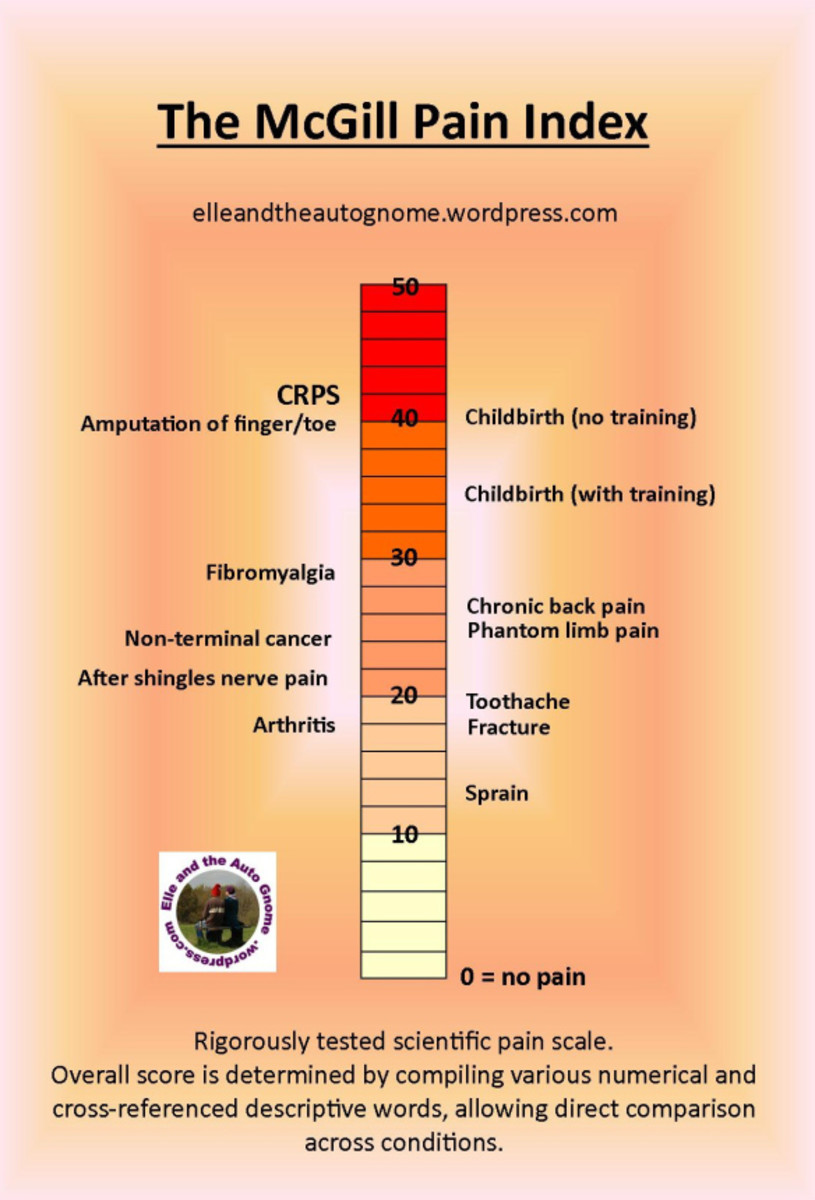
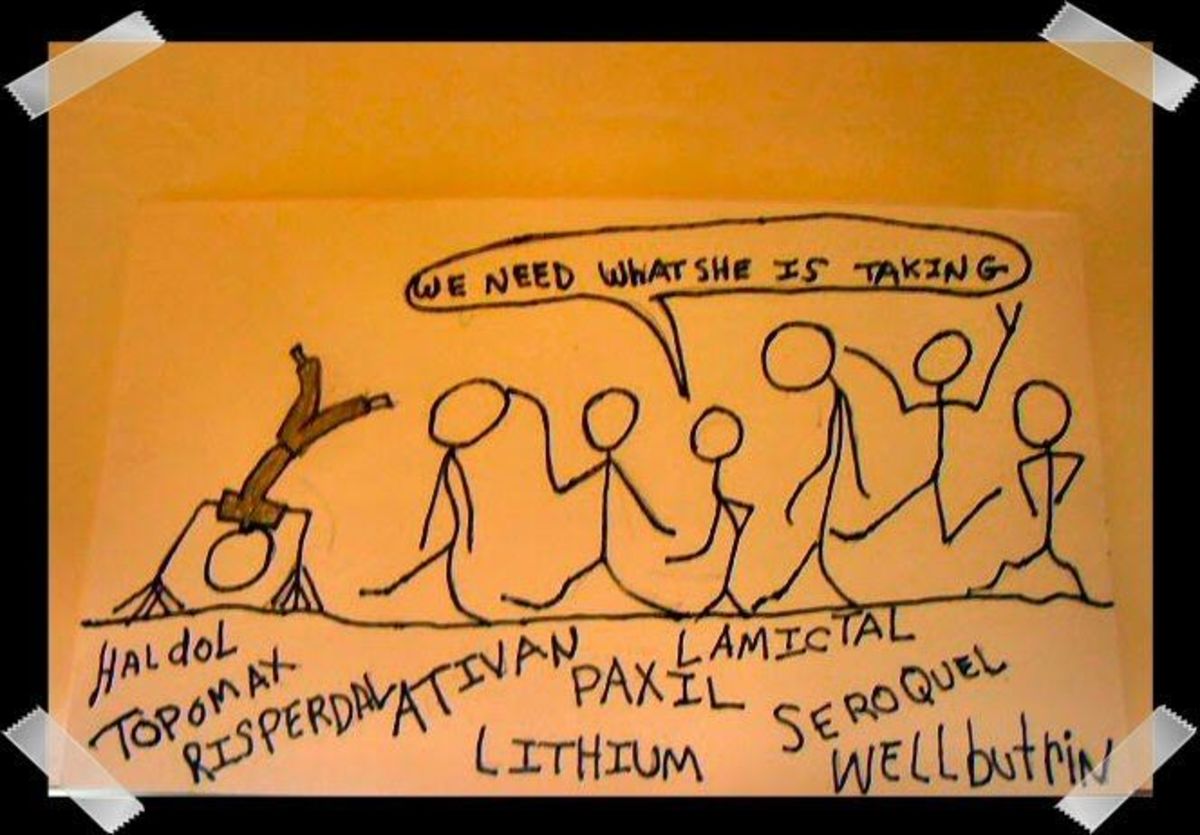
I only wish that I had questioned three years earlier the diagnosis that I was given it may have saved me the past two and a half years that I have had to undergo an emotional rollercoaster. We tried multiple medications and each one took months to find out if they were going to work or have to start again with the process.
When I was struggling to find answers I found some of the following information regarding depression. I hope this will make others understand how difficult this disease truly is either to live with or have someone in your family suffering with it.
"Major depressive disorder, also known as major depression, unipolar depression, clinical depression, or simply depression, is a mental disorder characterized by a pervasive low mood and loss of interest or pleasure in usual activities. The diagnosis is made if a person has suffered one or more major depressive episodes. Diagnosis is based on the patient's self-reported experiences and observed behavior. There is no laboratory test for major depression, although physicians often test for physical conditions that may cause similar symptoms before arriving at a diagnosis. The course varies widely, from a one-off occurrence to a lifelong disorder with recurrent episodes." As per the Wikipidia.
But how does that possibly affect us and what kind of symptoms should we be looking at?
According to many psychiatric professionals any change or increase in any of the following should be reported to your physician.
- ü DELAY IN FALLING ASLEEP AND RESTLESS SLEEPING
- ü WAKING UP TO EARLY
- ü SLEEPING TOO MUCH
- ü FEELING SAD
- ü FEELING OVERPOWERED
- ü DECREASED OR INCREASED APPETITE
- ü SUDDEN LOSS/GAIN OF WEIGHT
- ü CONCENTRATION/DECISION MAKING
- ü DECREASED SELF ESTEEM
- ü THOUGHTS OF DEATH OR SUICIDE
- ü LACK OF INTEREST
- ü ENERGY LEVEL
- ü FEELING RESTLESS
- ü FEELING LIKE MOVING OR SPEAKING IS MUCH SLOWER
Depression can make you feel hopeless and helpless. But by taking the first step -deciding to get treatment-can make all the difference
Medical care is the ONLY Answer! Seek a professional for there assistance.
It is believed that there are many reasons that people suffer debilitating depression. Feelings of depression are caused by a chemical change that affects how the brain functions.
The brain is made up of billions of nerve cells called neurons. These neurons send and receive messages from the rest of your body, using brain chemicals called neurotransmitters.
These brain chemicals-in varying amounts-are responsible for our emotional state. Depression happens when these chemical messages aren't delivered correctly between brain cells which lead to disrupting communication.
The good news is that there are many forms of treatment that can help you cope with depression, including medications that can strengthen weak signals by raising the levels of certain neurotransmitters, or by improving the neurons' ability to process signals. This ensures that the brain's vital messages are received.
Who Gets Depression?
Although depression can make you feel alone many people will suffer some form of depression in their lifetime. While depression can affect anyone, its effect may vary depending on your age and gender.
Women are almost twice as likely to become depressed as men. The higher risk may be due partly to hormonal changes brought on by puberty, menstruation, menopause, and pregnancy. The most common time of onset is between the ages of 30 and 40, with a later peak between 50 and 60. The condition appears to be more common in women.
Men. Although their risk for depression is lower, men are more likely to go undiagnosed and less likely to speak up and get help. They may show the typical symptoms of depression, but are more likely to be angry and hostile or to mask their condition with alcohol or drug abuse. Suicide is an especially serious risk for men with depression, who are four times more likely than women to kill themselves.
Elderly. Older people may lose loved ones and have to adjust to living alone. They may become physically ill and unable to be as active as they once were. These changes can all contribute to depression. Loved ones may attribute the signs of depression to the normal results of aging, and many older people are reluctant to talk about their symptoms. As a result, older people may not receive treatment for their depression.
Children. Age does not discriminate when it comes to depression. The family structure has changed causing additional stresses to family. Children are affected by the social pressures that they now feel. Bullying, abuse by others, pressures to succeed all add to the reasons that many children are affected. Symptoms should be looked for by the parent. Suicide is rising amongst this age group due to depression.
DEPRESSION DOES NOT DISCRIMINATE
IT'S NOT A RARE DISEASE
I found some great information regarding the Definition of Manic-depression also known as Major Depression.
Manic-depression: Alternating moods of abnormal highs (mania) and lows (depression) is called bipolar disease because of the swings between these opposing poles in mood. Bi-Polar is a type of depressive disease that is not nearly as prevalent as other forms of depressive disorders.
Sometimes the mood switches are dramatic and rapid, but most often they are gradual. Mania often affects thinking, judgment, and social behavior in ways that cause serious problems and embarrassment. For example, unwise business or financial decisions may be made when an individual is in a manic phase. Bipolar disorder is often a chronic recurring condition.
A mild to moderate level of mania is called hypomania. Hypomania may feel good to the person who experiences it and may even be associated with good functioning and enhanced productivity. Thus even when family and friends learn to recognize the mood swings as possible bipolar disorder, the person may deny that anything is wrong. Without proper treatment, however, hypomania can become severe mania in some people or can switch into depression
.
Most people with bipolar disorder -- even those with the most severe forms -- can achieve substantial stabilization of their mood swings and related symptoms with proper treatment. Because bipolar disorder is a recurrent illness, long-term preventive treatment is strongly recommended and almost always indicated. A strategy that combines medication and psychosocial treatment is optimal for managing the disorder over time. Medications known as "mood stabilizers" usually are prescribed to help control bipolar disorder.
There are several different types of mood stabilizers are available such as Lithium, valproate, carbamazepine, lamotrigine, gabapentin and topiramate.
As an addition to medication, psychosocial treatments -- including certain forms of psychotherapy (or "talk" therapy) -- are helpful in providing support, education, and guidance to people with bipolar disorder and their families. Studies have shown that psychosocial interventions can lead to increased mood stability, fewer hospitalizations, and improved functioning in several areas. Psychosocial interventions commonly used for bipolar disorder are cognitive behavioral therapy, psycho education, family therapy, and a newer technique, interpersonal and social rhythm therapy.
Treatment DOES Work! Seek help from a professional and start getting your life back or help your family member get the help that they deserve. They really do want to feel better.... Trust me. Depression hurts everyone!