Diagnosing and Treating Gestational Diabetes

By Joan Whetzel
Finding out you are pregnant is a happy event for those who are trying to have a baby. You don’t want anything to spoil that happiness. Yet, not all pregnancies go off without a hitch. Sometimes they are complicated with certain conditions, like gestational diabetes; a condition that usually makes it’s appearance about 24 weeks into the pregnancy. It’s important to make sure that women are tested regularly throughout the pregnancy. And if the condition is diagnosed, then the mom’s need to follow a diet and medication regime that keeps both her and the baby healthy.
What Is Gestational Diabetes?
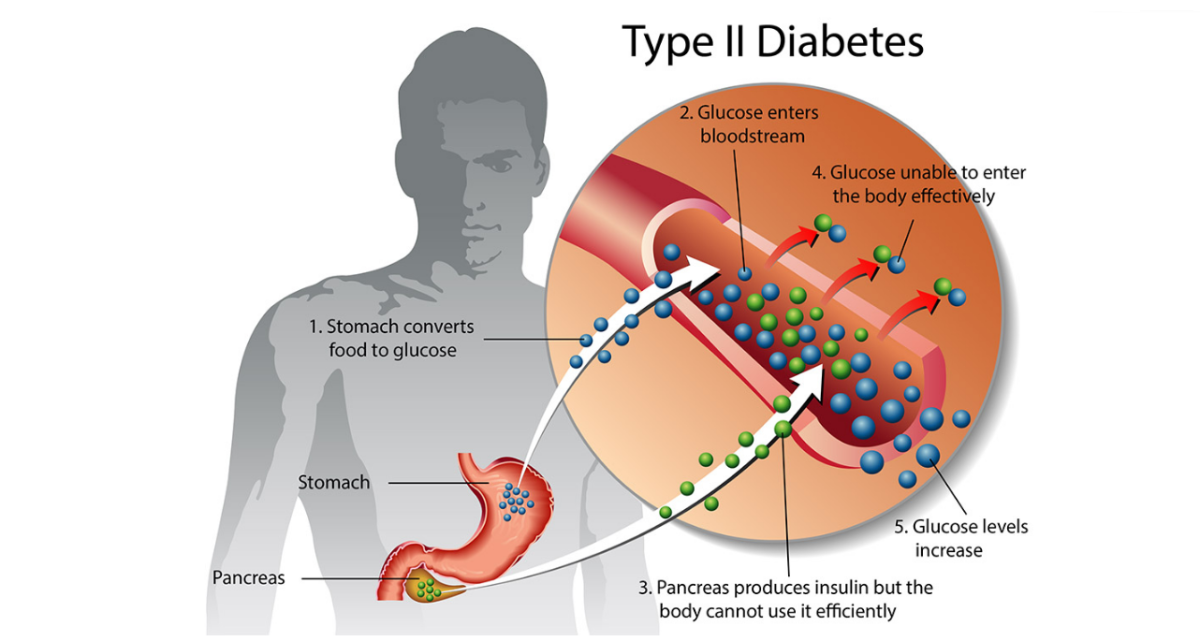
Gestational diabetes occurs when blood sugar levels rise during pregnancy. It is estimated to occur in about 18% of all pregnancies. There is no known cause for the occurrence of gestational diabetes, only some working theories. One of the prevailing theories is insulin resistance, believed to be a condition where hormone’s from the placenta block the insulin in the mother’s body. In this case the mother may need to take insulin injections 1 to 3 times a day, along with diet and exercise to help control the blood sugar levels.
Controlling Gestational Diabetes
Because gestational diabetes occurs later in the pregnancy, after the development stage, it doesn’t cause the types of birth defects seen with many other conditions. Left untreated, or poorly controlled, gestational diabetes can still harm the baby and the mother though.
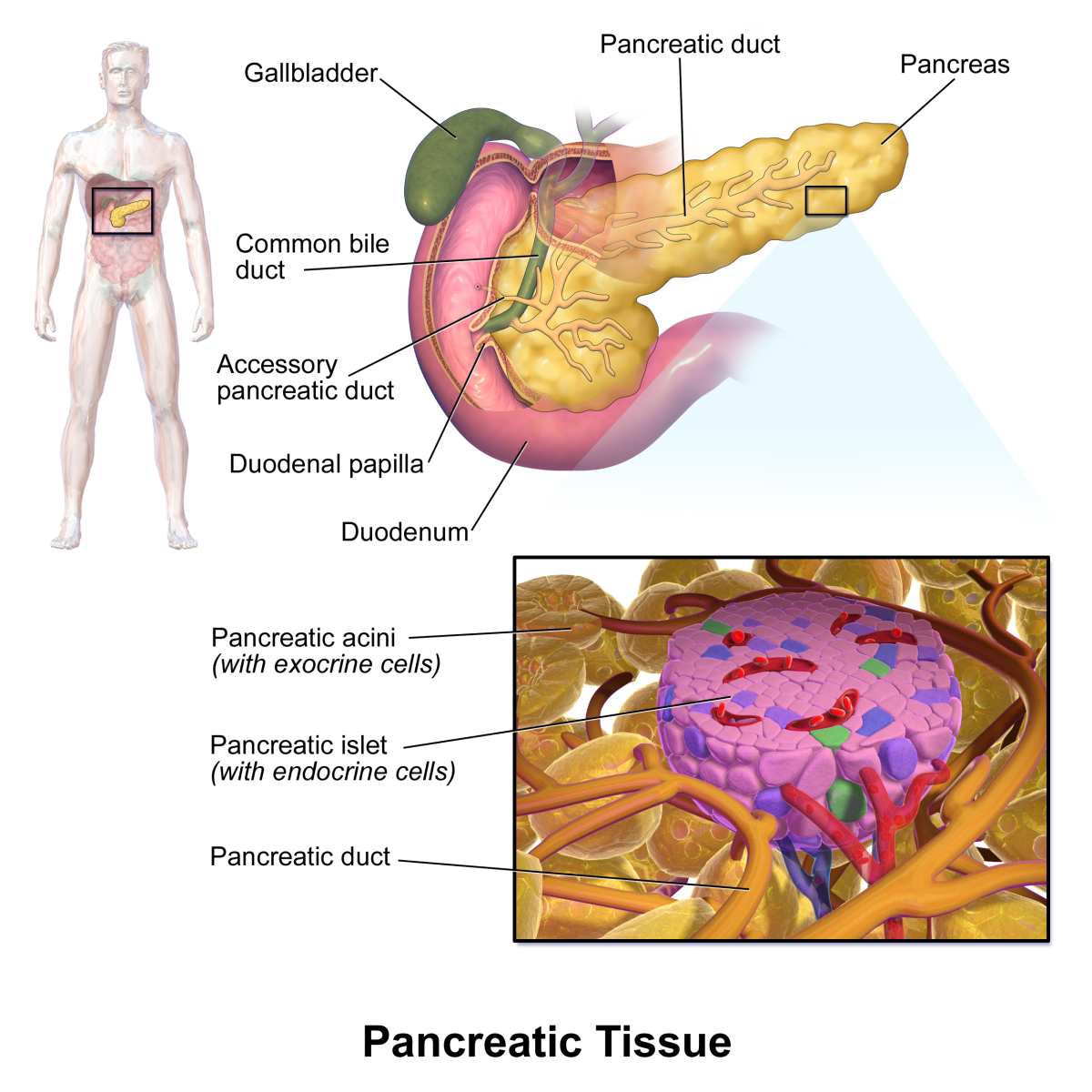
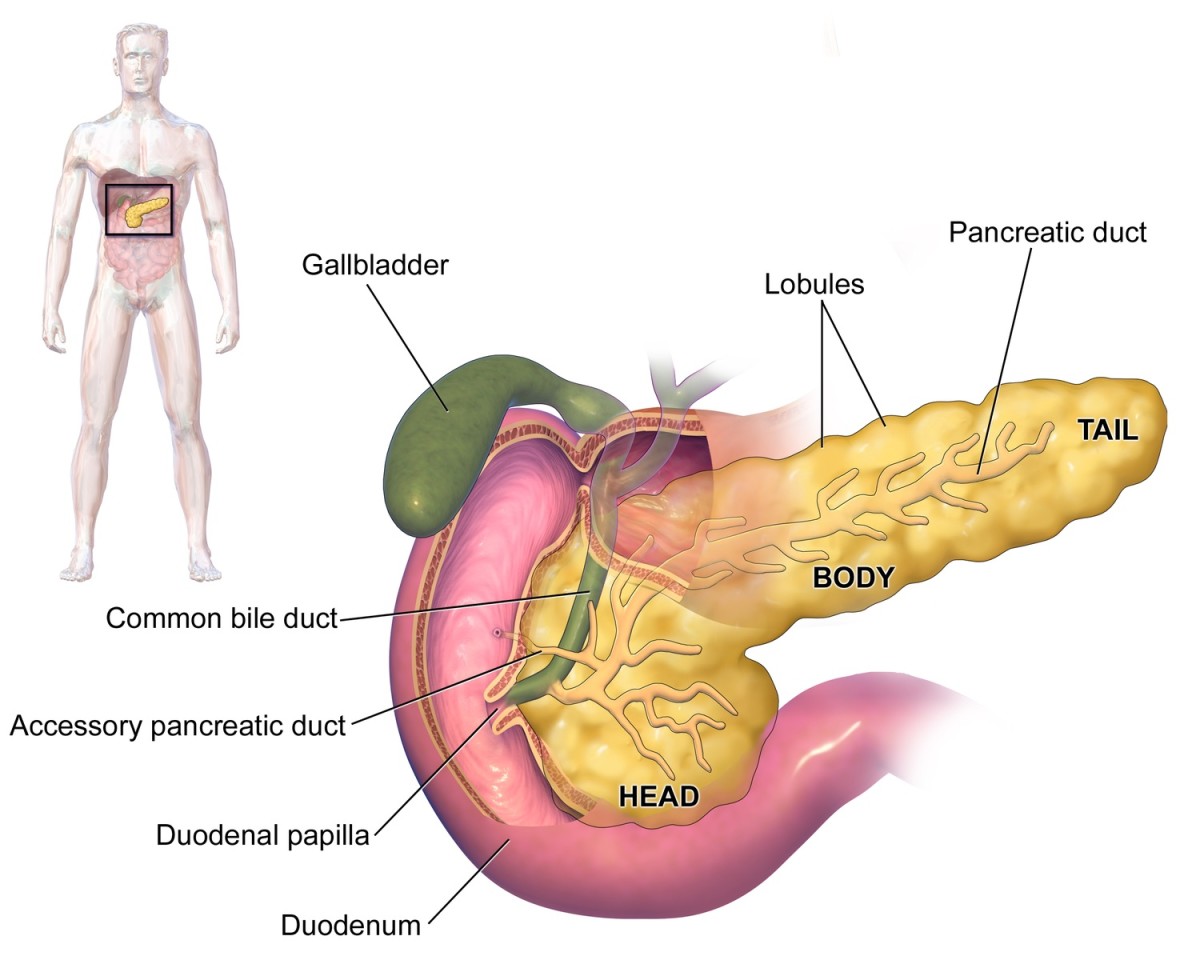
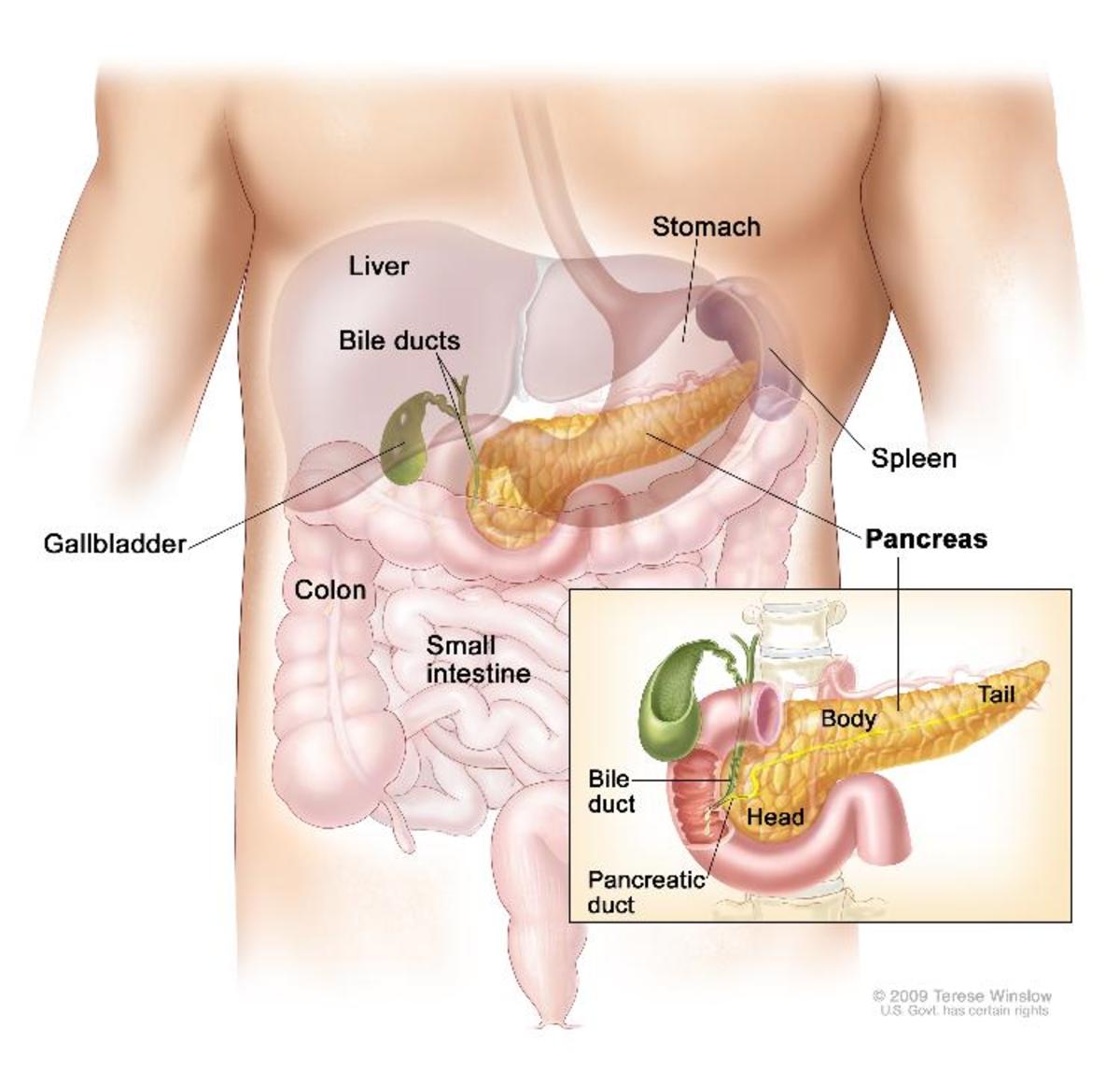
The mother’s pancreas goes into overdrive trying to produce enough insulin to take care of the blood glucose to no avail. The extra insulin does not cross the placental barrier, but the higher glucose levels will pass through to the baby, causing the baby’s pancreas to produce extra insulin. So now the baby’s getting way more energy than it needs from all that glucose, and begins storing it as fat. The baby soon grows so large that it may be difficult to impossible to deliver vaginally. So some women may require a c-section or have labor induced early.
Another complication is that, any baby that has been producing extra insulin in-utero will likely be born with low blood sugar. This is a serious health risk for all babies born to mom’s with gestational diabetes. The babies need to be monitored, and the blood sugar’s managed, until their system stabilizes. Babies born with the excessive insulin are at risk for childhood obesity and type 2 diabetes as adults. As for the risk to the moms’, it’s a good news/bad news thing. The good news is that gestational diabetes almost always clears up within a week or two of delivery. The bad news is that women who have had gestational diabetes are at much greater risk of developing type 2 diabetes later, especially if they are overweight.
Symptoms and Testing for Gestational Diabetes
Here’s the kicker. Women with gestational diabetes won’t know they have it because they don’t exhibit symptoms. That’s why monitoring their blood work and urine tests, and performing a glucose screening around 24 to 28 weeks is so important.
Risks of Having Gestational Diabetes
The American Diabetes Association lists the risks for gestational diabetes as follows.
- 1. Your are overweight.
- 2. You have had gestational diabetes in a pregnancy prior to this one.
- 3. You are spilling sugar in your urine.
- 4. You have a family history of diabetes.
Signs that may cause your midwife or doctor to watch you more closely for signs of gestational diabetes include:
- You have given birth to one or babies weighing 8.75 pounds or more.
- You’ve had a stillbirth for no apparent reason
- You have delivered a baby with a birth defect.
- You have high blood pressure.
- You are over the age of 35 years.
- You have excessive weight gain during your pregnancy, especially in the first trimester.
Treatment for Gestational Diabetes
Treatment for gestational diabetes is geared toward controlling mom’s blood sugar levels, keeping them at levels that considered normal for a non-pregnant state. That means moderate exercise to help make use of the glucose, a calorie controlled diet of nutritious foods (meats, dairy, fruits and veggies, starchy foods, and some fat), and in most cases, insulin injections 1 to 3 times a day. Mom also should be checking her blood sugars several times a day to make sure her levels are staying within normal limits. Normal limits are:
- Around 80 to 95 mg/dl before meals.
- 120 mg/dl 1 to 2 hours after meals, but not more than 14 mg/dl.
Keep a journal of blood sugar levels, when they were taken, insulin injections, and meals. Take the journal with you to all doctor’s appointments as well as your glucose meter. The meters they make these days can be plugged into a computer so that the doctor can watch your progress. Check the American Diabetic Association website for diet plans. If this doesn’t help you, have your doctor or midwife recommend a nutritionist to help you set up a diet plan for you.
Your doctor or midwife may also want to monitor your pregnancy more closely. Yes, that means more visits, but it’s worth it to make sure you deliver a healthy baby.
Resources
American Diabetes Association. Gestational Diabetes.
http://www.diabetes.org/diabetes-basics/gestational/
Baby Center. Gestational Diabetes.
http://www.babycenter.com/0_gestational-diabetes_2058.bc?page=1
Mayo Clinic. Gestational Diabetes.
http://www.mayoclinic.com/health/gestational-diabetes/DS00316
Web MD. Gestational Diabetes.