Diagnostic Prerequisites And Treatment Of Hodgkin’s Lymphoma
Treatment Of Hodgkin Lymphoma

Clinical staging
This is based on the extent of the disease at the time of presentation. Classified in 1971, during the Ann Arbor conference.
Stage I: Lymph node involvement in one anatomical lymph node region (I) or in a single extra-lymphatic organ (IE).
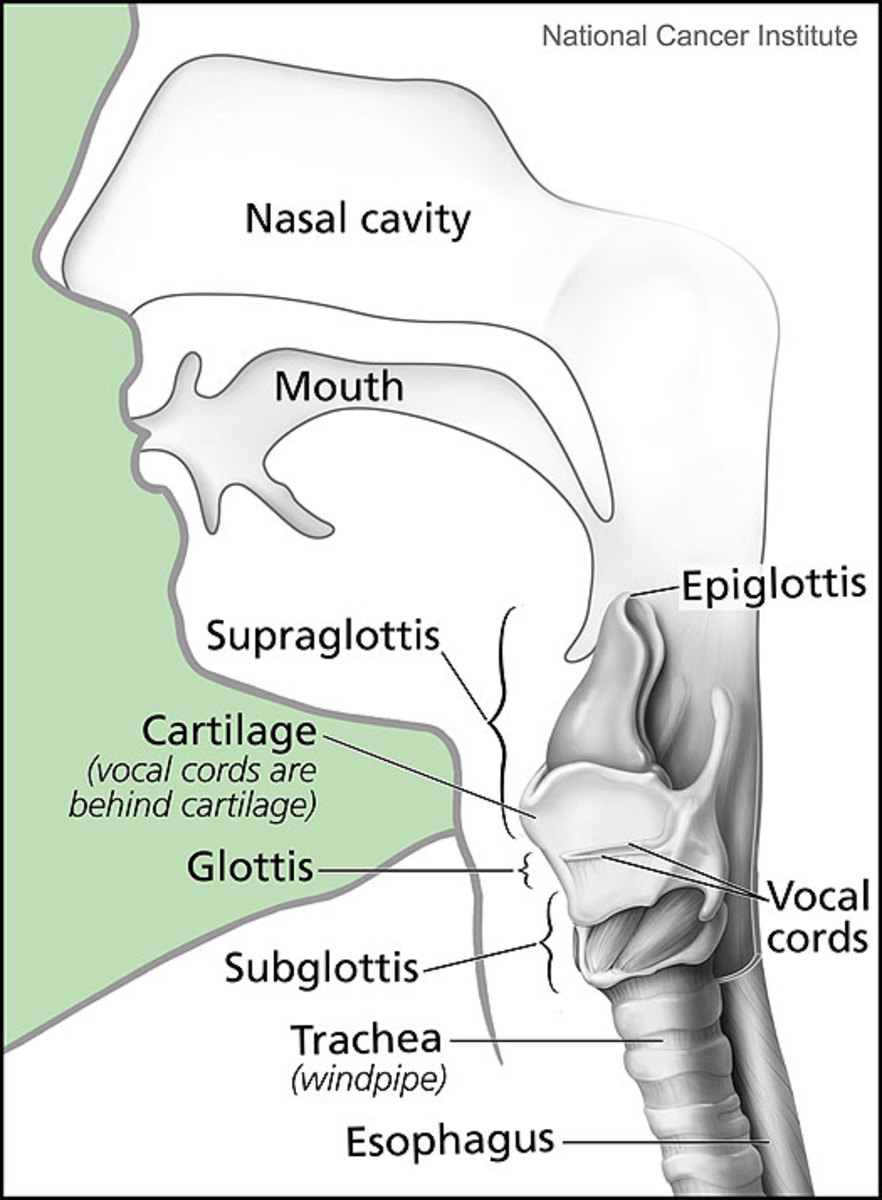
Stage II: Involvement of two or more lymph node regions, confined to the same side of the diaphragm (II) or localized involvement of an extralymphatic organ and one or more lymph node regions on the same side of the diaphragm (IIE).
Stage III: Involvement of lymph nodes above and below the diaphragm (III) which may also be accompanied by splenomegaly (IIIs).
Stage IV: Extensive disease involving nodes on either sides of the diaphragm and involvement of extralymphatic tissues such as bone marrow, live, etc.
Each stage is further classified as B or A, depending upon the presence or absence of constitutional symptoms. The important constitutional symptoms are:
- Fever above 380C and night sweats and
- Loss of 10% of body weight within six months
In group B, the prognosis is worse compared to group A both from the point of remission and duration of survival.
Diagnosing Hodgkin Lymphoma

Staging Procedures And Investigations
Staging procedures
Since the choice of initial therapy depends on the stage, full investigation should be undertaken in all cases before deciding the therapeutic schedule. It has been established beyond doubt that proper staging and institution of appropriate therapy initially are most important in bringing about a favourable outcome.
Investigation of a case of lymphoma
- Full clinical examination
- Radiology of the chest to reveal mediastinal nodes and pulmonary involvement
- Complete hematological investigations
- Bone marrow trephine biopsy
- Live function tests and liver biopsy if liver is enlarged
- Isotopic liver scan to detect lymphomatous involvement
- Lymphangiography to detect disease in abdominal nodes and for follow up. The dye persists in the lymph nodes for over one year and therefore the response of these lymph nodes to treatment can also be followed up.
- CT scan of abdomen and chest to detect enlarged masses.
- IVP to detect glandular masses around the kidney.
- Inferior venacavogram to detect abdominal nodes.
- Ultrasonography to detect masses of glands in the abdomen
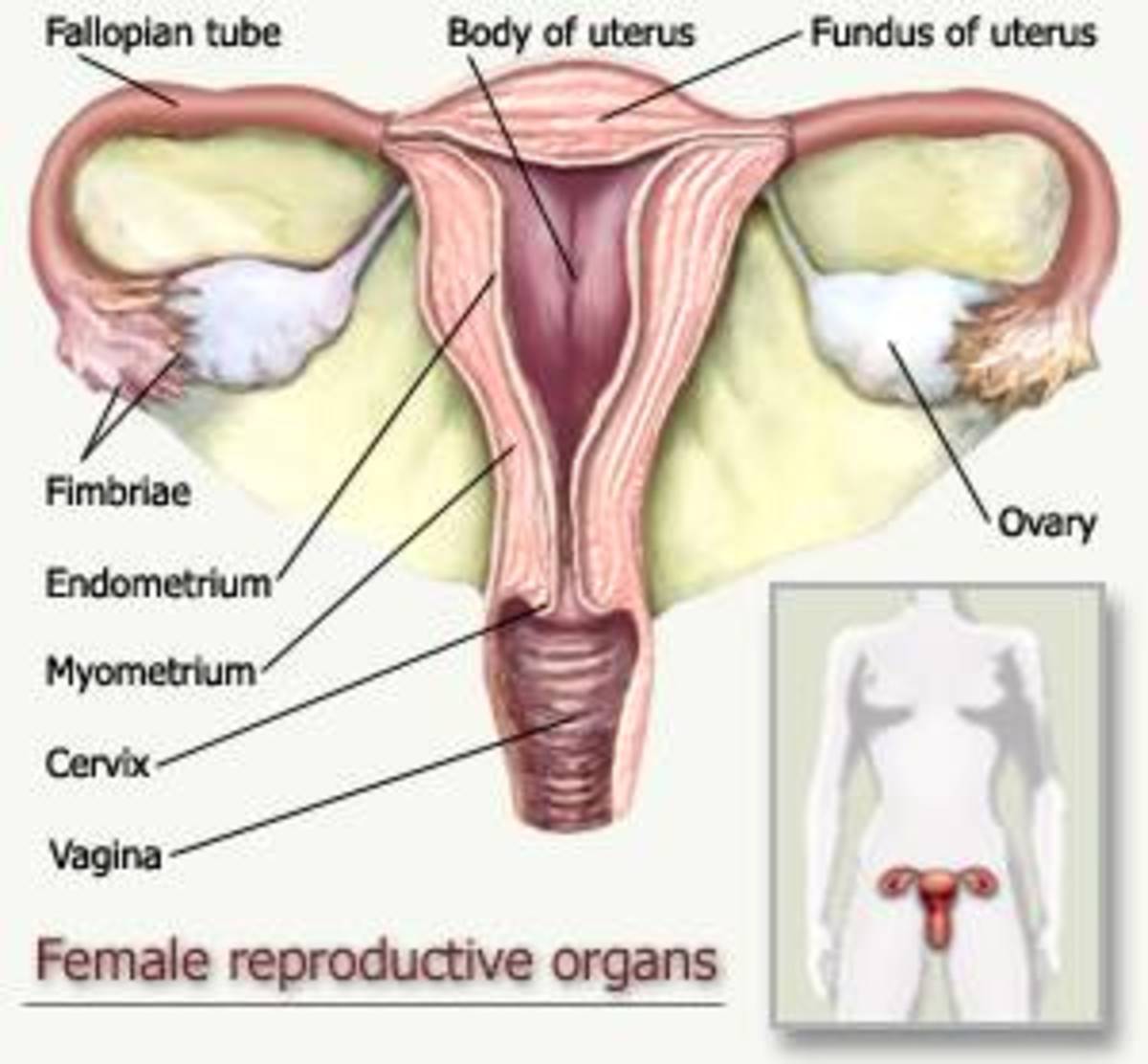
- If by all these methods, the disease is staged as II or I, laparatomy and splenectomy are indicated. A normal sized spleen may still be the seat of lymphomatous involvement and only by histological examination can involvement of the spleen be excluded. In addition to splenectomy, a staging laparotomy includes lymph node biopsy from the portal, para-aortic and iliac nodes and repositioning of ovaries in young females for preotecting against irradiation. Splenectomy also improves the tolerance of the subject to combination chemotherapy. For children under 13, splenectomy carries the risk of fatal pneumococcal sepsis and hence this is not advocated. For stages III and IV, laparotomy and splenectomy are not indicated, since the disease is already widespread.
Symptoms Of Lymphoma

Treatment
Stages I and II: Radiotherapy with a total dose of 4000 to 4500 rads given in 4 weeks is the method of choice. A total dose not below 4000 rads is curative in 90% of cases. Improved high voltage radiotherapy techniques allow safe irradiation of al lymph nodes above or below the diaphragm by upper mantle or inverted Y fields.
Stages III and IV: Cyclical chemotherapy is used. The most popular combination is MOPP and this consists of:
Dose
| Days
| |
|---|---|---|
Mustin hydrochloride
| 6 mg/m2 intravenous
| 1 and 8
|
Oncovin (Vincristine)
| 1.5 mg/m2 intravenous
| 1 and 8
|
Procabazine (Natulan-Roche)
| 100 mg/m2 oral
| 1 to 14
|
Prednisolone
| 40 mg/m2 oral
| 1 to 14
|
The 14-day treatment is followed by 14 day rest and the cycle is repeated. Usually, 6 courses of drugs are given. There are many other effective regimens which use different drug combinations.
Prognosis
Below 20 years (%)
| 21 to 40 years (%)
| Above 40 years (%)
| |
|---|---|---|---|
Stages IA and IIA
| 94
| 93
| 78
|
Stages IB and IIB
| 93
| 83
| 45
|
Stages III to IVA and B
| 80
| 61
| 22
|
Approximate five-year survival rates reported from the West
Lymphoma Treatment

Histologically, lymphocyte predominant types show the best prognosis. Circumscribed lesions have a better prognosis than diffuse lesions. Results in African series are not so encouraging as these figures suggest.
Relapses are managed by the same or alternate schedules of chemotherapy. In resistant cases, two regimen can be combined.
Long term risks
Only 1% of patients treated for HL develop acute myeloid leukemia which is resistant to thereapy. The risk of second malignancies is higher in treated HL patients than in the general population.
© 2014 Funom Theophilus Makama