Dupuytren’s Contracture - Home Management and Exercises - Part 1

Introduction
Dupuytren’s Contracture is also known as Morbus Dupuytren or Dupuytren’s Disease. It is characterised by the contracture of the palmar fascia of the ring and little fingers which bends the fingers towards the palm,and cannot be fully extended. The other fingers are less commonly affected and the thumb very rarely. In the advanced cases the middle finger is also affected. But usually the index finger and thumb are not affected. The ring finger is most frequently affected and later the ring finger. But sometimes the ring finger suffers first and then the little finger. This condition is named after Baron Guillaume Dupuyrten, a surgeon, who described the pathology of this condition. He suggested a surgery to correct this abnormality in 1831. The patient always complain of pain, aching or itching sensation. Usually the discomfort is felt along the contracture.
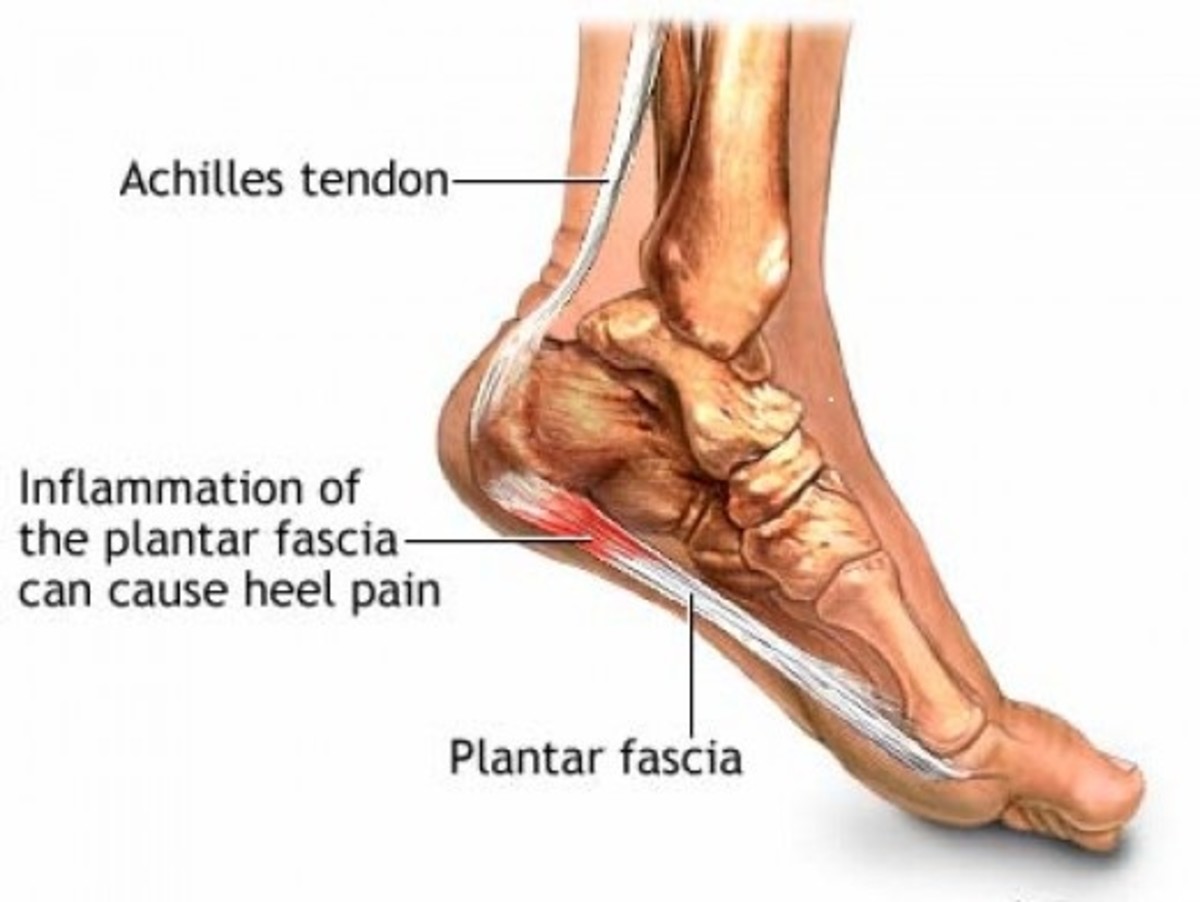
What is Palmar Fascia?
It is a layer of tissue that lies under the skin of the palm. It forms a protective covering to the small muscles,tendons,blood vessels, nerves etc. of the hand. It also gives strength to the grip. As a result in the advanced cases of Dupuytren’s Contracture the grip will be weak and the patient find it difficult to hold the objects.
What happens to Palmar Fascia?
Palmar Fascia becomes abnormally thick due to changes that occur in the collagen fibres (an Albuminoid substance in bundles).Normally the palmar fascia consists of collagen type 1 fibres, but in patients who suffer from Dupuytren’s Contracture the collagen type 1 fibres change to collagen type 2 fibres. The collagen type 2 fibres are thickePr than the collagen type 1 fibres. Hence the contracture slowly sets in.
What happens in Dupuytren’s Contracture?
The pathological changes are confined to the palmar fascia and the tissues superficial to it. As a result of chronic inflammatory reactions the palmar fascia becomes thickened and nodular. Later on there is perivascular proliferations which leads to fibrosis and contracture of the affected slips of the palmar fascia leading to the respective fingers. These contracted bands of palmar fascia to the respective fingers draw fingers into the palm of the hand. The fingers curl and hence adversely affect the hand function. The over lying skin also get contracted. In the later stages the skin gets adhered to the already contracted palmar fascia. The finger is first drawn down at the metacarpo phalangeal joint and then at the first and the second inter phalangeal joint so that finally the fingers are flexed and bend into the palm. Subsequently the joint capsules around the metacarpo phalangeal and inter phalangeal joints and the tendons will also contract leading to limitation of passive and active range of motion of the joints. In advanced cases arthritic changes also occur in the joints.
incidence
-
Sex- More common in men than in women.
-
Age- Usually in the middle or old age.
-
Ancestry- More common in Western countries.
-
Hereditary- Often runs in families.
Causes
-
Metabolic Disorders.
-
Injury to the tissues of the palm is an exciting cause.
-
Commonly found in those people who have an occupation which demands continuous use of hand.
-
Smoking- Smoking is associated with an increased risk of Dupuytren’s Contracture. This may be because smoking causes microscopic changes within the blood vessels of the hand adversely affecting the blood supply to the structures within the hand.
-
Alcoholism- Alcoholism also has a negative influence on the Dupuytren’s Contracture.
-
Diabetes.
-
Epilepsy Therapy with Phenytoin.
-
Liver Diseases.
-
Gout.
-
Rheumatism.
Symptoms
-
Presents with a flexion deformity at the metacarpo phalangeal joint of involved finger or fingers.
-
In the earlier stage, there is a hard nodule in the deep palmar fascia at the level of the metacarpo phalangeal joint.
-
In the later stage, shortened fibrotic bands of palmar fascia stand out as cords in the palm and can be palpated over the palmar aspect of the affected fingers and the flexion deformity becomes fixed. These bands may get extended upto the 2nd phalanges.
-
The skin gets adhered to the fibrotic bands and hence thrown into wrinkles.
-
The flexion deformity is more at the metacarpo phalangeal joint.
-
The may have a feeling of pain or irritation in the palmar aspect of the hand, especially along the contracted bands.
-
In most of the cases, there may be no pain unless the flexed fingers are forcibly extended.
Diagnosis
-
Compare with the other hand. Sometimes the condition may be bilateral.
-
Usually ring and little fingers are affected.
-
In the early stages, a palpable nodule may be present at the level of the metacarpo phalangeal joint.
-
In the later stages, flexion deformity of the affected fingers.
-
In the later stages, shortened fibrotic bands of the palmar fascia stand out as cords in the palm and can be palpated over the palmar aspect of the affected fingers.
-
Skin gets attached to the fibrotic bands and hence the skin may thrown into wrinkles.
-
Table top test- The patient places his hand on the table in such a way that the palmar aspect of the hand is in contact with the surface of the table. If the palmar aspect of the hand lies flat on the surface of the table, then the test is negative. If the palmar aspect of the hand does not lie flat on the surface of the table leaving a space between the palm of the hand and the surface of the table, the test is positive. In such cases treatment is indicated.
-
In the advanced cases,the individual is incapacitated from carrying out certain specific activities. Since the thumb and the index fingers are not usually affected, many do not experience much inconvenience or disability to carry out fine movements like writing in the early days. But once the condition progresses,it gets worsened to such an extend that the patient won't be able to open the fingers fully or to grasp large objects or to get the hand into narrow places.
-
Xray- may show arthritic changes in the metacarpo phalangeal joints and inter phalangeal joints.
Treatment
If the condition progresses slowly and has little impact on ones ability to carry out normal activities of day to day life, he may not need any treatment.But one must be very cautious and watchful to see whether the condition progresses further. Physiotherapy or surgical intervention is needed before the condition worsens.
Minor Invasive Techniques
Surgery is done on fingers that are severely affected and not in the early stages. Post operatively gain is more at the metacarpo phalangeal joint level than at the inter phalangeal joint level.
The surgical treatment involves removing or releasing the contracted fibrous bands which are responsible for flexing and pulling the fingers in towards the palm. This can be done by various surgical procedures. The choice of technique of surgical procedure depends on the severity of the symptoms. Moreover the choice of technique of surgical procedure varies from surgeon to surgeon.
-
Needle aponeurotomy- It is a minor invasive technique.In this technique a needle is inserted through the skin to ‘puncture’ and ‘break’ the contracted fibrous cords of the palmar fascia that is responsible for flexing in the finger or fingers. The contracted fibrous cord is sectioned at as many levels as possible along its length, depending upon the location and severity of the condition.Once the procedure is over, the punctured cord may be stretched with caution and the finger is pulled straight. After the treatment a small dressing is applied for 24 hours. After 24 hours the patient can use the hand normally. The disadvantage is that the procedure may damage the tendons or the nerves. Recurrence is possible.
Advantages-
a. No incision.
b. Can be done in several fingers at a time.
c. Immobilisation only for 24 hours.
d. Post operatively, physiotherapy not needed. -
Enzyme Injection- Injecting an enzyme into the tight contracted fibrous cord. This enzyme softens and weakens the cord. Now the softened and weakened cord may be manipulated and stretched out by straightening the fingers. The disadvantage is that the procedure may damage the tendons or the nerves and painful. Recurrence is possible. Advantages same as in the case of ‘Needling.’
Surgical Intervention
In early stages Subcutaneous Fasciotomy is beneficial. But in the later stages surgical excision of the involved fascia is the only reliable treatment. In severe cases the surgeon removes all the affected tissues including the adhered skin. If the skin is not removed completely, the deceased tissue may get adhered to the skin. Hence chances of recurrence is increased. There after skin graft is done.
Disadvantages-
a. Invasive technique.
b. Longest recovery period.
c. Longer periods of immobilisation.
d. Post operatively, longer periods of intensive physiotherapy.