- HubPages»
- Health»
- Women's Health»
- Pregnancy
Epidural during Labor: Epidural Complications and Controversies

What is an Epidural?
Religion, politics and labor epidurals...three topics that are guaranteed to start heated debates when the subjects come up.
While many women get epidurals for labor, there are some very vocal individuals and groups who seem to equate epidurals with attempted murder of their offspring.
Epidurals cause changes to the body, no doubt. There are even some potential issues with labor, delivery, the newborn, breastfeeding.... but those who distort or exaggerate the risks are doing a disservice to those who could be helped by an epidural.
HOW MANY WOMEN GET EPIDURALS?
Epidural analgesia (pain relief) is used frequently during labor and delivery, with over 50 percent of women receiving this type of labor pain relief in the United States. There is much variability in the epidural rate around the country due to a variety of factors, with some states reporting an epidural (or combined spinal/epidrual) rate of nearly 80 percent.
An epidural is placed into the small epidural space outside of sac that surrounds the spinal cord and spinal fluid.Usually, a catheter-- but not a needle-- as is sometimes feared, is left in place in the epidural space so that medicine can be given continuously or can be increased or decreased as needed.

Personal Note from the Author
Let me start by saying here and now, I am an anesthesiologist. I have placed thousands of epidurals. BUT, but, I have never talked anybody into one, I have never withheld information or refused to answer questions before or after the procedure. I am not part of some giant conspiracy to push epidurals or force interventions on women. I'm not selling anything. That said, I will not approve comment below that amount to a personal attack because of my profession. Thank you.
And yes, I have been directly or indirectly accused of these things without provocation when these very vocal and aggressive detractors find out I'm an anesthesiologist.
Epidural Controversies
There are many controversies related to epidural anesthesia during labor and delivery. The most common ones will be discussed here.
The choice to have an epidural is a personal one. Every woman who faces this decision deserves to be able to make it as an 'informed consumer'. This isn't necessarily easy as there is A LOT of misinformation and outright fallacy at the fingertips of every mom-to-be.
There are also some good, reliable sources of information. The problem is that it's hard to know which is which sometimes.
Epidural Catheter and Needle
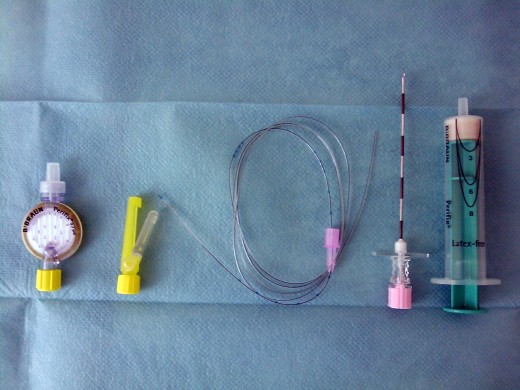
Epidural Catheter in Place

Epidural Risks
There are naturally, some risks of epidural anesthesia. After all, a needle is used to inject medication that, then, changes the workings of your body. It would be unrealistic to expect there to NOT be risk. However, understanding the risks and complications and their real likelihood is the best way to make an informed decision about receiving an epidural in labor.
Risks are undesired effects that may or may not happen, may or may not cause harm and may or may not be avoidable. These are just examples and are not meant to represent a comprehensive list of all risks that could have or ever have occurred.
- Any time a needle is used for a procedure, the risks of bleeding and infection exist. These occur rarely (1 in 200,000 cases), but can have devastating consequences, such as paralysis.
- An epidural, unlike a spinal, does not involve entering the space that contains the CSF. If the dura (covering over the spinal cord and fluid) is punctured unintentionally, a spinal headache can occur. The risk is less than 1 percent.
- There is a small risk of nerve injury or prolonged pain related to nerve irritation. The reasons for this are not entirely clear. This is actually also pretty rare. Many times that an epidural is blamed for nerve injury or back pain, special nerve/muscle studies will show that it is related to injury during labor and delivery rather than from the epidural.
There are some risks to the baby, as well, but how significant these are, is where a lot of the controversy arises concerning labor epidurals.
Pitfalls in Interpreting Data about Labor Epidurals
As always, it is best to evaluate data from outcome studies, analyses, meta-analyses and so on yourself. If you are not a scientist in the field of the study, you need to at least ask if the study is valid enough from which to draw conclusions. Because each person cannot possibly do this, peer review and standards are in place to help with this daunting task. Unfortunately, some people have chosen to try to draw conclusions that just aren't valid. Sometimes, this is done intentionally to promote a particular point of view. Sometimes, it is done out of scientific or medical ignorance (again, intentional or not) when the scientific process is not understood. There are many pitfalls to interpreting data from studies. Epidural-related topics are no exception. Here are some examples of reasons why drawing conclusions, even when they seem to be supported by data isn't always accurate.
Some data is older. Higher concentrations of more potent local anesthetics may have been in use during the time the older studies were done. Currently, very low concentration local anesthetics are used in most epidural preparations. Therefore, some older data (which opponents of epidurals love to quote) are no longer valid.
There is a "chicken or the egg" effect with epidural anesthesia. It is unclear when interpreting outcomes of women who get epidurals if there is a "cause and effect" relationship or just an association. An example would be the small-framed woman who requests an early epidural because of excessive pain. She ends up getting a c-section for 'cephalopelvic disproportion'. A study that evaluates the percentage of women getting a c-section after epidural would include her. However, it may be that she was destined for a c-section anyway because the baby won't fit through her birth canal. She had excess pain for the same reason and was, therefore, more likely to request the epidural. There are many, many of these variables that are hard to tease out or control for in a scientific study.
There are many other confounding variables, also.
- Some obstetricians are more likely to move onto C-section than others who are more comfortable with 'watchful waiting'.
- There are many possible combinations of drugs that can be used in the epidural solution. The addition of different medicines to the local anesthetic can change the effect of the epidural.
- Combined spinal-epidurals may be counted as 'epidurals' in many cases and may have different effects.
- Some studies compare epidurals to intravenous pain medication and some compare them to no intervention.
- First-time mothers may have different risk factors than women who have previously given birth.
- Older mothers are more likely to end up with C-section than younger mothers. This is one of many, many factors that are usually not controlled for, especially in older studies.
The list goes on and on and on and the above is a VERY small sampling of issues that complicate the picture and make it difficult to understand a particular study's conclusions. Unfortunately, these variables are hard for the professional to sort out. When the non-medical professional tries to interpret the data, it is even more difficult. This also makes it easier for the caregiver with an agenda to misrepresent the data (knowingly or not so) to push their beliefs on women in their care.
EPIDURAL CONTROVERSIES - SUMMARY
Controversy
| True or False or ?
| Explanation
|
|---|---|---|
Epidurals prolong labor
| TRUE
| Women who get epidurals spend longer in the second stage of labor. This has not been correlated with higher c-section rates or poor outcomes for the babies, however
|
Epidurals lead to c-sections
| FALSE
| Women who use epidurals for pain relief do not have higher c-section rates than mothers using other types of pain relief (intravenous, for example)
|
Epidurals make vacuum or forceps delivery more likely
| TRUE
| It is generally accepted that there may be a higher rate of instrument-assisted delivery in women with epidurals. Further studies need to be done with the lower concentration anesthetics currently in use. Also, there are still some unanswered questions about confounding factors.
|
Epidurals make it harder to breastfeed
| UNCERTAIN, MAY BE TRUE
| While this may be true in some circumstances, further studies are needed. Mothers who get epidurals may report more difficulty with breastfeeding. There may be an ingrown selection bias, as women who are opposed to epidurals may already be more committed to breastfeeding. Other variables may also be at play.
|
Epidurals interfere with my baby's breathing
| FALSE
| Babies born to moms who get epidurals don't fare any worse than other babies.
|
Epidural and Fever
| see discussion below in text
|
While there is definitely some individual variability, these are the currently accepted scientific positions based on the best available peer-reviewed studies and meta-analyses. Personal opinions and anecdotal 'evidence' will certainly stray from the
Epidural and Prolongation of Labor
Most of the current data suggests that epidural analgesia does prolong the second stage of labor, by about 5 percent. This prolonged labor does not translate to an increase in cesarean section rates. In other words, women with epidurals spend 30 to 60 minutes longer in labor, but are more comfortable (by most studies) and do not have increased cesarean rates.
Epidurals and C-Section Rates
Women with epidurals do not have a higher C-section rate than women receiving intravenous pain medication. It's possible that in some situations or labors, the epidural does contribute to further interventions culminating in C-sections. But, the assertion made by anti-epidural groups that this is usually, or always the case is not scientifically valid.
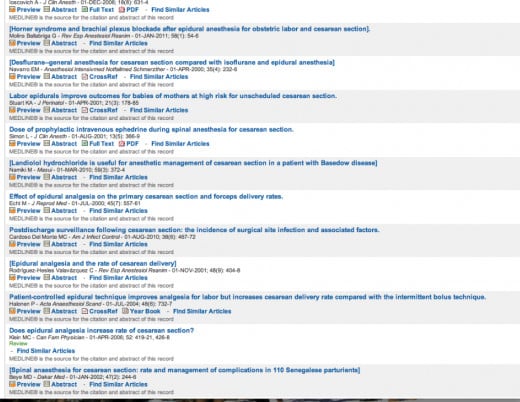
A Medline search, with the terms "epidural cesarean section rate", gives 587 results since the year 2000 in English-language, (mostly) peer-reviewed journals, showing that despite current evidence, this continues to be an area of active surveillance.
Medline Search: Epidurals and C-Sections
Epidurals and Breastfeeding
Women who receive pain relief during labor may initially (first day) have more trouble getting baby to latch on and breastfeed, especially in the first day after delivery. Some reports seem to indicate that overall success is affected. Many reports find no difference in long-term success in breastfeeding. Further, attempts at studying different preparations of medications has not shed any light on this topic so far (specifically, fentanyl, a commonly suspected narcotic medicine that is often added to epidurals, does not seem to change the stats). Institutions with lactation support seem (not clearly scientifically valid, by report) to have a much higher success rate for breastfeeding mothers, with or without epidural use.
The correlation between epidural and breastfeeding is met with some skepticism as to a cause and effect relationship. It is also possible that women who are more likely to request epidurals, also have other risk factors for difficulty with breast feeding. There are several confounding variables that may make a definitive answer hard to reach on this topic, although some groups like Lamaze have already made their conclusions.
Epidural Effect on Newborn
Infants born to mothers who had epidurals seem to have adequate and comparable oxygen levels and Apgar scores to non-epidural births. In the absence of other risk factors, epidural alone does not seem to adversely affect neonatal outcome (with the exception noted below).
Epidurals, Maternal Fever and Newborn Risk
As studies of the effects of labor epidurals have tried to separate and clarify any risk, it has been discovered that some women develop an elevated body temperature after receiving an epidural. Further, the higher the mom's body temperature during labor, the more problems her newborn may have after birth.
This is an undesired finding that is the subject of very active study. Researchers and clinicians, as well as patients, want to understand the factors that lead to fever in the laboring mother, and the adverse effects on the baby. Finding the cause is the key to prevention.
So far, using a representative study ("Intrapartum temperature elevation, epidural use, and adverse outcome in term infants; Greenwell, EA; Pediatrics: Feb 1, 2012; 129(2): e447-54) we know that around 19 percent of women will develop a body temperature of 100.4F or higher. This is much higher than the 3 percent of women without an epidural reaching the same temperature.
In women who had epidurals AND fever of greater than 101F, the risk to the baby for weakness, seizures and low Apgar scores were 2 to 6 times higher than for women without BOTH of these factors. Women who had epidurals, but maintained normal body temperature did not see an increased risk to the baby.
We don't understand why some women develop fevers and others don't. But, prevention of the temperature elevation seems to prevent problems with the babies.
Again, this is relatively new information and investigation is ongoing, but still in its early stages. But, women should be aware of this risk.