Exercise Guide for Diabetics

Planning for an exercise as part of the treatment regimen for diabetes mellitus is a good idea. This is beneficial for the whole body, not just for diabetic care. Exercise is well known to enhance blood circulation, thus, promoting wellness. The major effects of exercise in the body includes the enhancement of heart functioning, fluid and electrolytes balance, and aids in the detoxification of the blood. All in all, exercise promotes good health and prevention of future health problems.
With the case of diabetes mellitus, having regular exercise is recommended a part of the treatment regimen, but, needs extra caution because of the existing health problem. It is then advised to consult a specialized physician (diabetologist) in planning for an exercise regimen to incorporate in the diabetic plan of care.
The following are some of the basic principles in planning for an exercise that suits your case, as a diabetic.

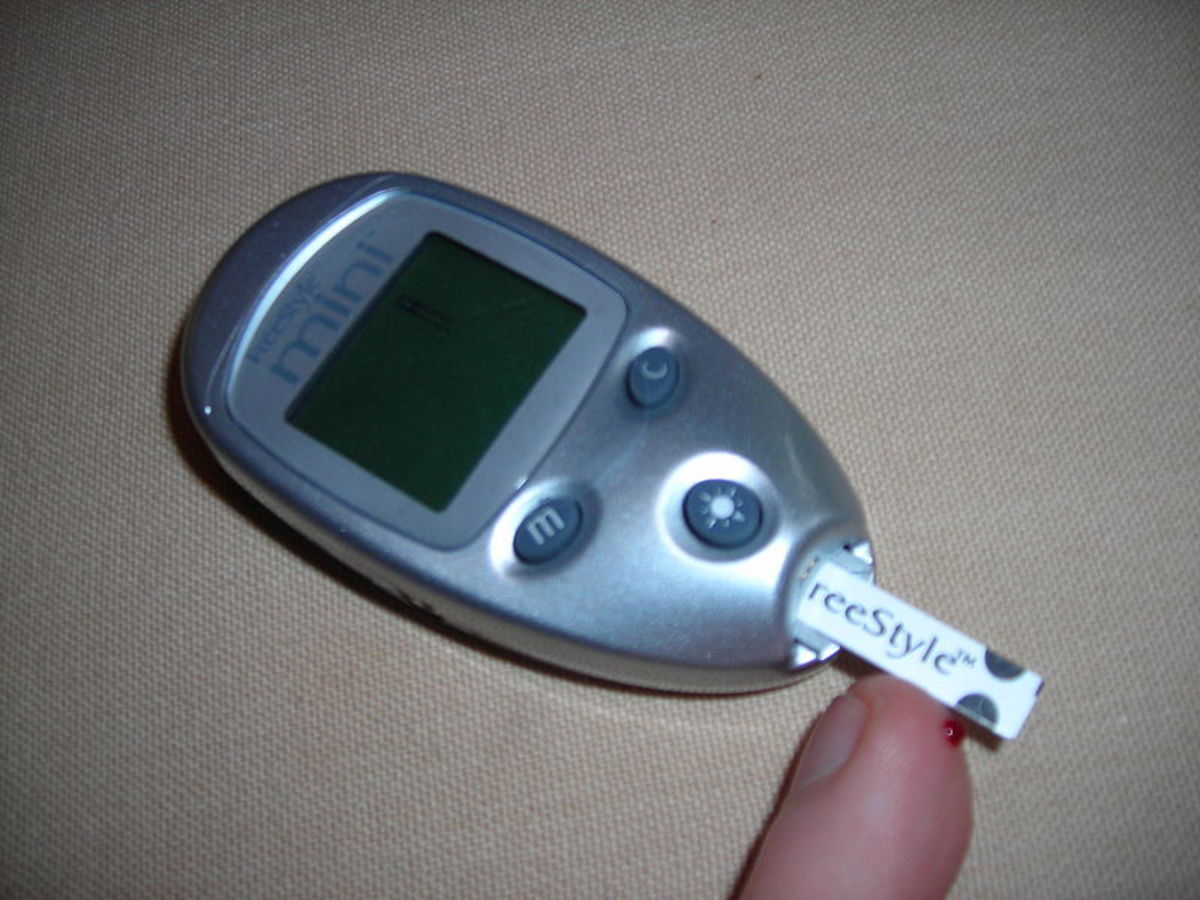
1. Check your blood glucose level before doing the exercise. This helps you plan the intensity of activity that is appropriate for your case. The lower the blood glucose level, the lesser activity is advised. The most important aspect of knowing your blood glucose level before execution of any exercise is the prevention of sudden onset of hypoglycemia or low blood glucose level, especially if you just took an insulin medication. If blood glucose level is low or near the normal range for diabetics, exercise is discouraged for safety reasons.
2. Bring good sources of glucose. This is to make sure that you have good sources of glucose reserves on your pocket while you are on activity. There are a lot of diabetics who suddenly developed hypoglycemia while on exercise and suffered injuries from fall and accidents. In cases of hypoglycemia, the best sources of glucose that may be administered to the person are fruit juices and candies.
3. Wear a wrist tag or any identification that would identify you as a diabetic. This helps rescuers identify your health condition in cases of fainting and unconsciousness brought by hypoglycemia. Providing health informations even in semi-conscious or unconscious state would help the rescuer speed up the treatment process and prevents further diagnostic examinations that could delay treatment.
4. Never start an exercise with an empty stomach. Having exercise with an empty stomach would double the chances of having hypoglycemia, especially, after taking any dose of insulin or any hypoglycemic agents. Eat meals with good proportion of carbohydrates is advised.
5. Never exercise without any companion. Bringing companion during exercise would lessen the chances of injuries and delayed emergency response during hypoglycemic attacks. Make sure your companion knows your health condition, for him/her to have anything to report once health problems arise during exercise.

6. Wear proper protective apparel. This may include jogging pants and long-sleeved shirts even with exercise of minimal effort. Even with walking, these are advised to prevent scratches and light skin wounds that may occur during exercise, especially, during emergency situations. Take note, with the case of diabetes mellitus, there is a high tendency of infection development and poor wound healing.
7. Always start light. This can be done by starting from stretching and walking. This is for the toning of muscles and heart conditioning to avoid sudden change of their workload that causes circulatory problems and sudden lowering of the blood glucose level.
8. Know the weather condition. Extreme weather, either hot or cold, has negative effects on the blood glucose level. Most of the diabetics who continue exercising under extreme temperature suffer from hypoglycemic attacks. Check first for local weather reports before proceeding.
9. Take the blood glucose level after each exercise. This is to evaluate the response of the blood glucose level to the exercise. This must be compared to the blood glucose level before the exercise, recall the type of activity done, and its duration for you to have basis for the next plan of activity. This will also serve as the basis of the day’s diet and insulin dosage.
10. Document the result. The person should have a hard copy of his/her blood sugar monitoring before and after each exercise. This is to have something to present to the physician, this is for evaluation and possible modification of the treatment regimen during the next check-up.