Fecal Microbiota Transplantation For The Treatment Of Irritable Bowel Syndrome
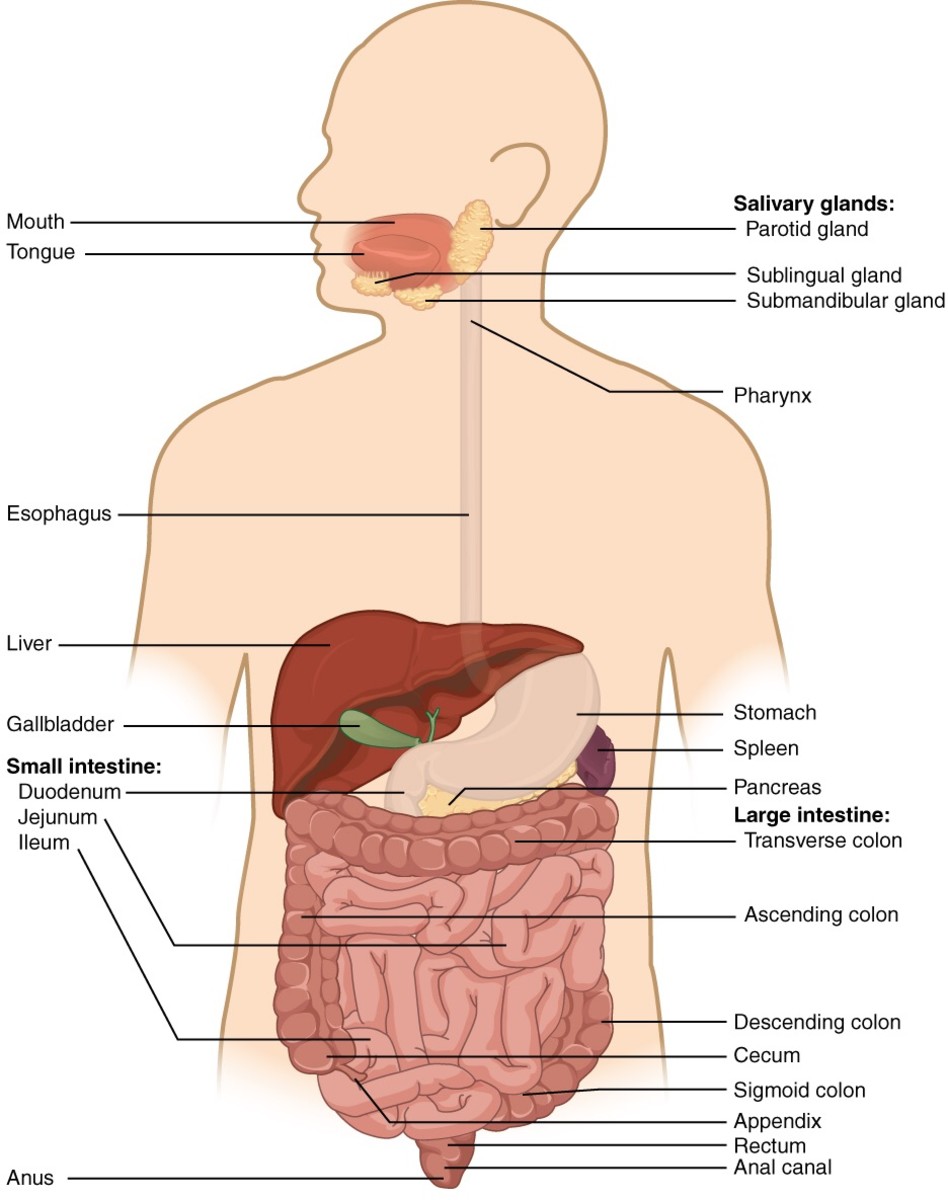
Irritable bowel syndrome (IBS) is the most common functional gastrointestinal disorder, (and one of the most common gastrointestinal diseases worldwide), with no clear underlying causative factor and no single effective and curing treatment known.
The diagnosis is based on exclusion of other diseases of the gut, by appropriate tests, imaging, and possible colonoscopy, and the presence of the characteristic symptoms of IBS.
The occurrence of IBS in the general population is estimated to be around 15% or more, as many people don't seek medical help when the symptoms are mild.

What's the role of colonic bacteria in health and disease?
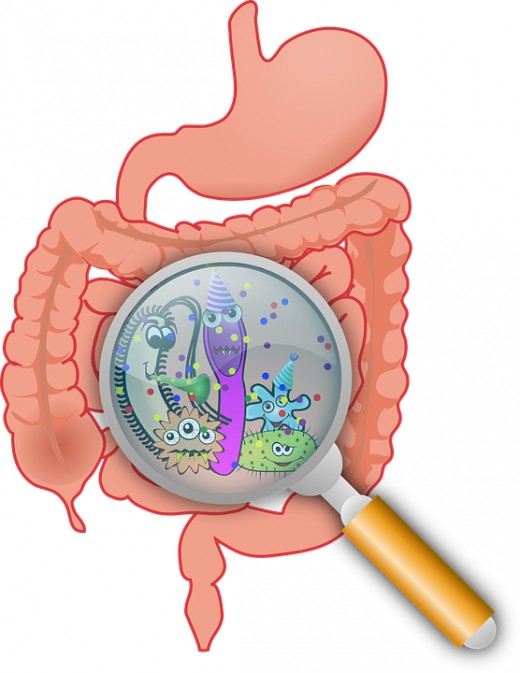
During the last few years, more attention was paid to bacteria in the colon (large bowel) as a significant determinant for the development of IBS.
Bacteria are normally present in the colon, and is called “normal flora”, which doesn't cause disease, rather it helps in digestion, and even provide us with vitamins, B and K, they synthesizes.
Colonic bacteria is also called “microbiota”, a word that means : microscopic living organisms
In subjects with IBS this bacterial flora demonstrates differences from that of unaffected subjects, which is essentially a different bacterial flora (or microbiota) population.
In other words, the species of bacteria and their numbers differ from that of normal, creating a colonic medium that favours and triggers the development of IBS symptoms.

Colonic bacterial infections , is a well known strong trigger of IBS. Bacterial infections commonly cause diarrhea, and increased “washing out” of healthy microbiota, another factor which adds to the process of microbiota population change.
Symptoms of IBS persist even after an infection subsides, a fact that supports the role of unhealthy microbiota in the causation of IBS.
Based on these facts, it was suggested that if this “unhealthy” medium in the colon, is restored back to normal, it would theoretically help curing IBS.
Of course, genetic and environmental factors may also play a role in IBS, along with the presence of abnormal colon motility, increased sensitivity to pain when the colon distends with gas, and the influence of signals coming from the brain.
Why Fecal Microbiota Transplantation?
The idea of restoring colonic microbiota to normal, was further polished, and the way how to change the colonic bacterial flora was already there and was used to successfully cure other colonic diseases. It's fecal microbiota transplantation (FMT).
FMT denotes the process of transferring the normal “microbiota” from a normal person to the patient's colon in order to replace his/her “unhealthy microbiota”, with the healthy “donated” substitute.
FMT is considered as a curative therapy for “Clostridium difficile” infection (a bacterial infection that causes diarrhea and can resist antibiotics), with restoration of normal microbiota and complete recovery.
The other disease that responded to FMT is inflammatory bowel disease.
Since the principle is the same, FMT has been tried for treating IBS symptoms, with obvious success.
How altering the colonic microbiota can cure gut disorders, including IBS?
Microbiota and immunity
The presence of normal microbiota is essential for the immunity of the gut. It has been linked to the normal development of the lymphoid cells in the gut ,an important first-line defence system.
When the microbiota is altered (as in persons suffering from IBS),this system becomes abnormally and inappropriately activated , producing a mild and ongoing inflammatory process, which is thought to be responsible, in part, for pain.
In addition, the colonic lining becomes permeable, so that it no longer acts as a defence barrier against threats from the gut lumen.
Microbiota and the brain:
A second role of microbiota is to connect between the brain and the gut, in a way that any stress, either psychological or physical, will affect the biological properties of colonic microbiota. The latter, then enhances the colonic wall sensitivity to pain.
Bacterial infections of the colon can significantly change the composition of the colonic microbiota, an effect that may trigger the development of IBS.
The same can happen with the use of antibiotics, since antibiotics kill certain types of microbes, allowing other types to grow, and the final outcome would be a change in microbiota composition.
In contrary, treatment with probiotics (microorganisms that have beneficial health effects when consumed), normalizes the microbiota population, and the sensitivity of the colon to pain diminishes, hence, symptoms of IBS get relieved.
What' are the characteristic properties of microbiota in IBS?
Patients with IBS have the following important microbiota features:
- Less numbers of the bacteria known as “Lactobacillus” , “Bifidobacterium” , “Bacteroidetes”, and “Actinobacteria”
- Increased numbers of the bacteria “Enterobacteraceae” and “Firmicutes”
These differences in the composition of microbiota in IBS patients from the normal, suggested that restoration of the normal microbiota may help curing the disorder, a process that can be achieved by FMT.
Furthermore, differences in the microbiota have been recognized between the different subtypes of IBS : diarrhea-predominant, constipation-predominant, and mixed subtypes.
How effective is Fecal Microbiota Transplantation in treating IBS?
FMT has been already shown to be effective in the treatment of Clostridium difficile infection.
But recently, the fact that FMT is likely to be effective in other diseases, including IBS, has been studied, with very promising results.
The success rate of treating IBS with FMT, reaches 70-90% as studies showed.
How is the “donor” of the fecal material selected?
A donor is the subject who donates his/her feces to be “transplanted” in the patient's gut.
Before transplantation, a donor should be screened for infectious diseases, to ensure safety of the procedure.
A donor shouldn't have practised high risk behaviours, like illicit intravenous drug abuse, which expose to the risk of acquiring infections.
Additionally, a donor shouldn't have used antibiotics or medications that suppress immunity, within the preceding 3 months, because these can change the composition of the normal donor's microbiota.
How Fecal Microbiota Transplantation is done?
The fecal material of the donor, when processed is infused into the gut by any of these methods:
-A nasogastric tube: a slim flexible tube that's passed through the nostril and advanced down to the stomach.
-A nasoenteric tube: similar to the nasogastric tube, but is further pushed into the small bowel.
-Endoscopy : either upper endoscopy, or lower endoscopy (colonoscopy).
-Enema.
Among the above mentioned routes, colonoscopy is associated with better results in patients treated for Clostridium difficile infection, though it's still not clear which of them is most appropriate for treating IBS.
Further research is required to determine the optimal route of FMT administration for patients with IBS.
Is FMT acceptable by people?
Studies showed that FMT acceptance is very high (more than 95%), although some routes through which the material is infused are less acceptable, as in the case of upper endoscopy or nasogastric tube, in comparison with colonoscopy or enema, which are best preferred.
Recently, a manufactured capsule containing the microorganisms thought to be responsible for the healing effect of FMT, is available and may revolutionize this kind of treatment when its efficacy is proven.
Safety of FMT:
Since FMT requires the inoculation of a very dirty and highly contaminated material from one person to another, a theoretical risk of transmitting infectious diseases is always there.
Human feces contains thousands of strains of bacteria, some are beneficial, and some are harmful.
The results of the available studies on FMT, proved that when the donor is properly selected and thoroughly screened for contagious diseases, the risk of complications is extremely negligible.
Is FMT currently used for treating IBS?
While FMT is becoming increasingly available and permitted by regulations for use as a treatment option for patients with Clostridium difficile infection, it's use for IBS is still under strict control.
Further studies are needed to strengthen the evidence of FMT efficacy for curing IBS symptoms, in order to be recommended as a standard therapy.
So how will be the future of FMT?
Based on the available data, FMT is going to be an effective, and curing treatment for IBS sufferers.
The evidence is growing day-by-day, to support this relatively newly applied method of managing some gut disorders, to include also other functional gut disorders, and not just IBS.