- HubPages»
- Health»
- Women's Health»
- Pregnancy
Fetal Heart Monitor Types Used by Doctors: Contraction & Non-Stress Test, Fetal Scalp Monitor & Doppler

When I went in for my first non-stress test when I was pregnant, I found out that there was a problem with my baby's heartbeat. I never left the hospital that day...or for the next six weeks. Until my baby was born, in fact. For many days my baby, still a fetus in the uterus, was monitored continually for irregularities in the heartbeat. Though my doctor had used fetal doppler on me before, I never really thought of a fetal heart monitor as anything other than cause to "ooh" and "aah." But in the hospital, all that changed. The fetal monitor became my curse and my salvation. By the end of my pregnancy I became familiar with more types of fetal heart monitor than I'd ever hoped to know.
What Is Fetal Monitoring?
Fetal monitoring is used by doctors to monitor the heart rate of an unborn baby. At around 12 weeks gestation, your doctor may use a small ultrasound device called fetal doppler to pick up the heartbeat by placing it on your abdomen and listening through speakers. Doctors may also use a fetoscope after 18 weeks to listen to the baby's heartbeat. Neither of these types of fetal monitoring are sufficient for ongoing monitoring during high-risk pregnancy or labor. A bit more complicated are the electronic fetal monitoring or internal monitoring used for longer stretches of time or continuously during labor and during high-risk periods in pregnancy.
Two main types of monitoring are done clinically - electronic monitoring using ultrasound with an external fetal monitor or internal fetal monitoring. Types of external fetal monitoring include the non-stress test (NST) or contraction stress test (CST). Scalp monitoring is the common form of internal monitoring used.
My baby and I received many non-stress tests and contraction stress tests while in the hospital, and I'm very glad we did.
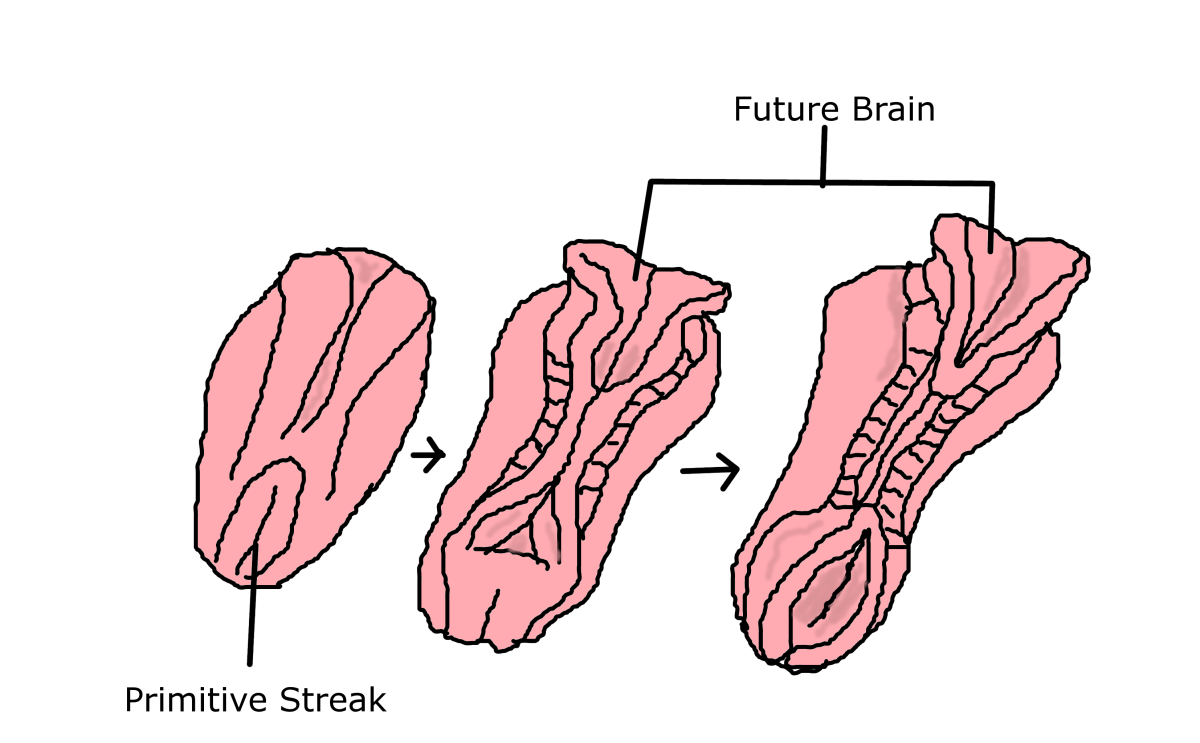
What is a Fetus?
Your baby starts being called a fetus at about 10 weeks into pregnancy. Before then, your baby is a zygote or an embryo, and after she's born, she's a baby! Read more about the fetal development timeline in the first trimester of pregnancy.
Non-Stress Test and Contraction Stress Test
A routine non-stress test takes under an hour and is quite tolerable. It is given anywhere from 27 weeks of pregnancy on in order to detect signs of fetal distress.
You can assume one of several reclining or even side-lying positions. If you have breathing problems lying on your back because of pregnancy, tell the nurse or technician, as I did - you can be elevated comfortably or moved at an angle.
The health care provider rubs conducting jelly over your abdomen and then attaches electrodes to the spot above the baby. Your baby's heartbeat will be detected through your abdomen with perhaps a little bit of maneuvering of the electrodes. Sometimes the baby moves and sometimes finding the heartbeat can be challenging.
If after about half an hour the heartbeat hasn't been detected, this is not necessarily an alarming thing. Your baby might simply be asleep, or in a difficult position. The doctor may give you some food to eat - which is almost guaranteed to wake the baby up and get that fetus moving enough to find the heartbeat.
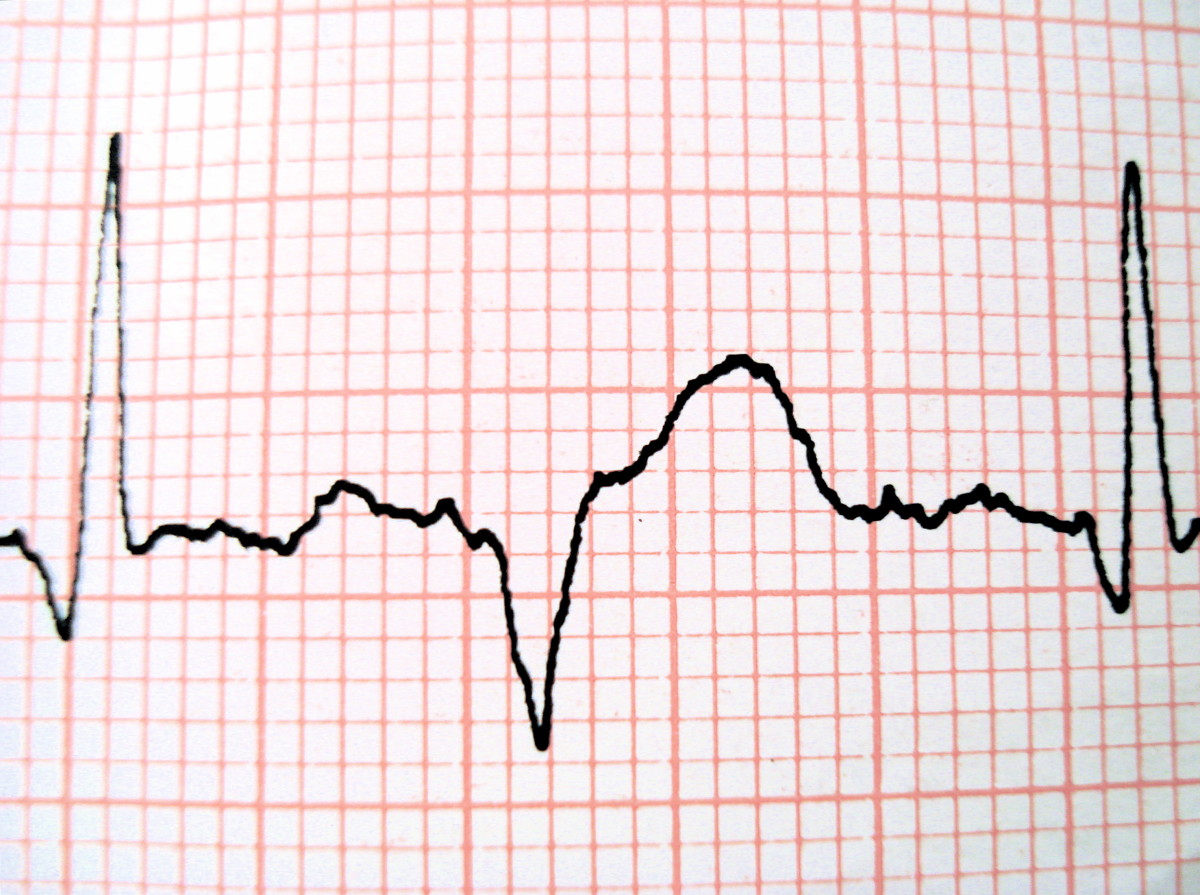
You can ask to see the graph of the heartbeat and hear the heartbeat yourself during or after the non-stress test.
The contraction stress test is similar. With extra electrodes, it detects when your uterus contracts (though not how strong the contractions are). When it is performed, it is done simultaneously with the non-stress test so your doctor can see if the contractions are affecting the baby's heartbeat (as mine were).
The contraction stress test is specifically designed to test more than the fetal heartbeat. It detects how well or how poorly your placenta is providing oxygen to the fetus during a contraction. This will give a measure of the risk of traditional labor and indicate whether a cesarean section may be indicated. To stimulate contractions, you may be given oxytocin as part of the oxytocin challenge test. Another type of test that serves a similar function is one that uses friction on the nipple to stimulate contractions.
Are non-stress tests or contraction stress tests dangerous? According to MedLine Plus, no known risks exist, though some individuals suspect there could be an association with early delivery or cesarean section that's not medically called for. That has not been established one way or another with medical evidence.
Fetal Scalp Test
If there's a problem or question with external fetal monitoring, you may get fetal scalp monitoring. Unlike the non-stress test and contraction-stress test, there's no use of ultrasound, and this test is more accurate.
This test is only used when your water is broken. If the test is indicated, an amniotomy may be performed to break your water. An electrode is inserted through the vagina and cervix and attached to the fetus's scalp. The electrode is connected to a wire that's connected to a monitor.
I didn't get administered this test - though I swear it feels like that's the only test I didn't get during my pregnancy! Is it comfortable? According to MedLinePlus, "Some patients report feeling mild discomfort while the electrode is inserted through the cervix." So I wouldn't expect lots of fun. But your odds of getting the test are slim.
Is a fetal scalp test dangerous? I don't know if it's any less or more dangerous than amniocentesis. The risks of the test include possible infection or the bruising of your baby's scalp.
Fetal Monitoring During Labor and Birth
Pregnant women who are in one of the following categories may receive continual monitoring during the birthing process:
- high-risk pregnancy
- induced labor
- getting an epidural
The non-stress test and contraction-stress test may be used either continually during the entire birthing process or intermittently. The scalp test is used continually only during labor and birth.
Results of the Fetal Non-Stress Test, Contraction Stress Test and Scalp Test
The tests are designed, ultimately, to find out how well your baby is likely to handle the birthing process - essentially, whether the fetus is in "fetal distress."
When the uterus contracts during labor, your baby's heartrate will drop a bit with the constriction of blood flow - but you don't want it to drop too much, nor do you want the baby to have trouble recovering from the drop. That's called fetal distress.
If the fetal heart rate measured on the non-stress test ranges from 120 to 160 beats per minute, with about a 5 to 25 beat-per-minute fluctuation from the normal baseline, this is generally considered normal.
When the fetal heartbeat results do not fall into the normal range - as they didn't with my baby - it could mean one of several things. Some possibilities are:
- The umbilical cord might be twisted or blocked temporarily with the baby's movements.
- Fetal heart block could be occurring. This is when an irregular heartbeat rhythm is caused by a blockage in the heart.
- The fetus is in a breech position, (fetal malposition or malpresentation) with the head up and the feet down.
- There's not enough oxygen reaching the fetus (fetal hypoxia).
- There's an infection somewhere.
- There's a problem with the supply of oxygen to the placenta, and therefore the baby.
- Fetal distress is occurring.
- The placental lining has been damaged - this is called abruptio placenta.
When you're pregnant and your doctor uses some type of fetal monitor to check out your baby's heartbeat, it's almost impossible not to fear the worst. But the odds of there being a problem are statistically slim. My advice, based on my own experiences as an older pregnant woman? Your best approach is to stay informed, talk to your health care provider if you have any concerns, and be prepared for anything.
How Stressed Were You By the Non-Stress Test?
Do you think "non-stress test" is a HUGE misnomer?
Disclaimer
This isn't medical advice. Please don't take it as such. This is information I learned when I was in the hospital and based on my research on fetal monitoring since. Ask your doctor any questions you have about the different types of fetal monitoring.

![The Fallout From the Conservative Assault on the Right to Privacy and the Supreme Court's Lurch back to 1820 [Updated] The Fallout From the Conservative Assault on the Right to Privacy and the Supreme Court's Lurch back to 1820 [Updated]](https://images.saymedia-content.com/.image/t_share/MTkxMTU1MjUyMDYwMjM1NTM5/the-fallout-from-the-conservative-assault-on-the-right-to-privacy-and-the-supreme-courts-lurch-back-to-1820.jpg)