How to Help Avoid a Medical Misdiagnosis
Compromising Health With Misdiagnosis
A Case Study
When I presented with chronic bladder spasms, a doctor quickly categorized my symptoms as "overactive bladder." I was given drugs to halt my urine spasms which gave me dry mouth. I was advised that my back pain and heavy menstruation were unrelated. After a decade and thousands of dollars in visits to a urologist AND gynecologist, I finally received the correct diagnosis: the worst case of endometriosis my veteran gynecologist had ever seen.
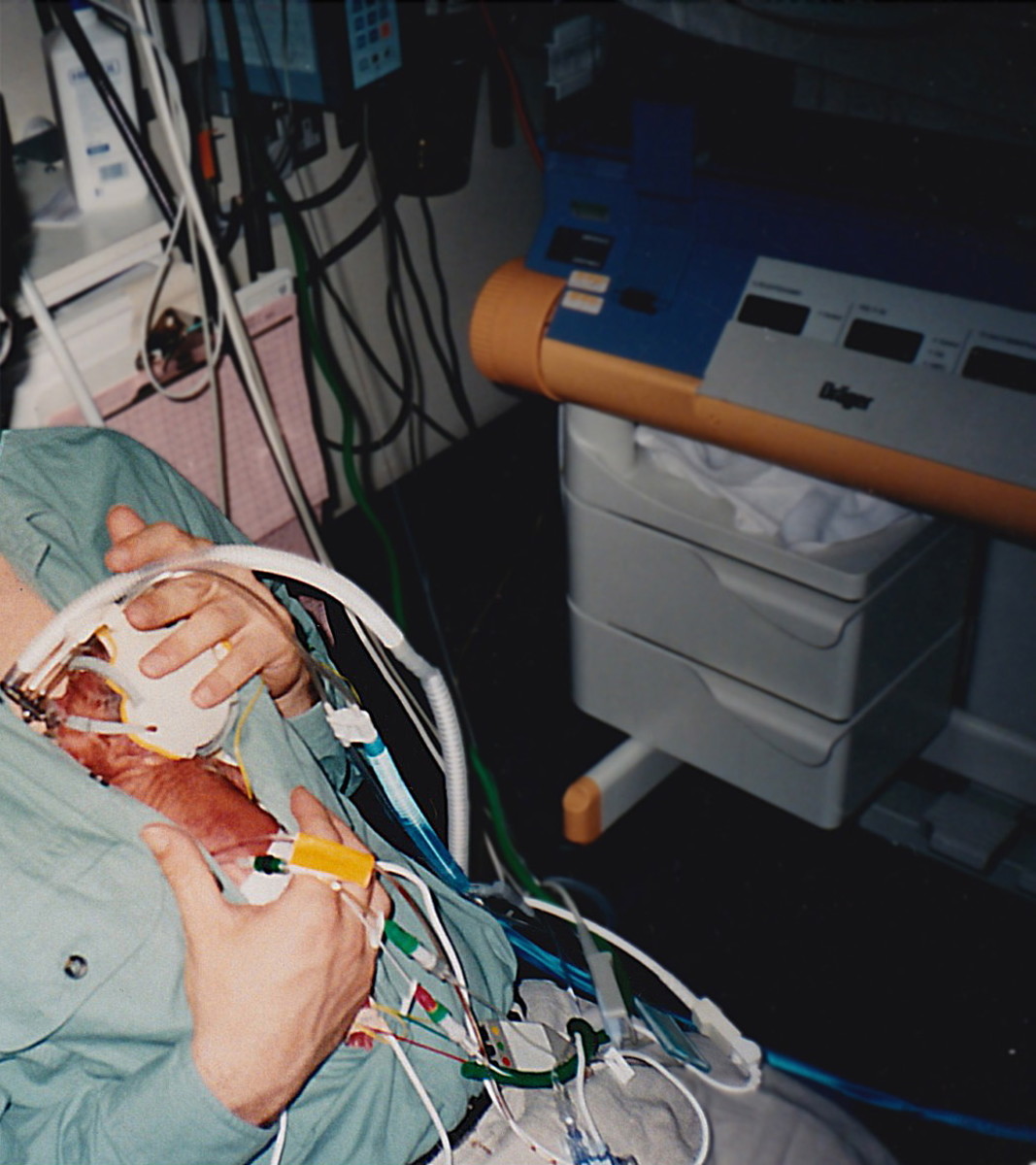
The treatment for my condition required the removal of both ovaries at age 32 and the loss of my ability to bear children. This in turn necessitated hormone replacement therapy (HRT) with an emphasis on progesterone therapy until I reached menopause age. Despite the removal of the majority of endometrial lesions, I continued to experience debilitating bladder spasms which required me to undergo numerous bladder distensions in order to reduce discomfort and pain. Each and every distension required general anesthesia costing me several more thousands of dollars in expenses and an incalculable effect on my general well-being and daily life.
According to Endometriosis.org, endometriosis affects 1 in 10 women at some point during their reproductive ages. The World Health Organization suggests that this incurable disease affects 10% of females globally, or 190 million women. Why then was it so difficult for me to obtain an accurate and timely diagnosis?

Primary Care Passing the Diagnostic Buck
My entire ordeal could've been minimized. My gynecologist kept insisting my issues were urological as my urologist pointed the finger back at him. My primary care physician merely shrugged contending the crisis was outside his purview. In terms of specialists, it took a gynecologist, a urologist, a pathologist, and a general surgeon to diagnose my condition. Until I pleaded with my gynecologist and urologist to work together as co-diagnosticians, neither had picked up the phone to call the other.
Dr. Sandeep Jauhar wrote an article for Time in 2014 entitled Doctored: The Disallusionment of an American Physician. In the article, he noted,
"In 1940, three-quarters of America’s physicians were general practitioners. By 1960 specialists outnumbered generalists, and by 1970 only a quarter of doctors counted themselves general practitioners."
The Association of American Medical Colleges reported that, as of 2019, there were over 938,000 U.S. doctors of which 118,198 (12.59%) served family medicine or general practitioner roles. This means that between 2014 and 2019, the number of general practitioners dropped another 50%.
Whether there are too few general practitioners bears direct relevance to the role they play as diagnosticians. A decade earlier (in 1993), then President Bill Clinton was criticized for suggesting that the U.S. needed to ensure there were an adequate number of general practitioners, even if that meant government regulation. Mr. Clinton was advocating the active role general practitioners play in patient health, diagnosis and prognosis. Dr. Robert Summitt, former Dean of the University of Tennessee College of Medicine agreed. Though citing reluctance, Summit saw the need for regulation to control an outbreak of medical specializations that didn't serve U.S. patients well. Derek Thompson, writing for The Atlantic in 2022 noted,
"Overburdened with debt and eager to translate their long education [eight years] into a high salary, American medical students are more likely to become specialists, where they tend to earn some of the highest doctor salaries in the world, in part because the U.S. does such an efficient job at limiting the supply of their labor."
Too Many Specialists And Not Enough Diagnosticians
Specialists are GREAT — at their specialty. The inherent problem with too many specialists is that general practitioners who are increasingly scarce are depended upon to know what type of referral is needed. It is well known, for instance, that cancer is easier to cure when caught early. General practitioners are generally better equipped at steering patients toward the right path because it is their job to analyze a set of facts and symptoms that lead toward a diagnosis.
The Society to Improve Diagnostic Error in Medicine states that diagnostic error accounts for up to 80,000 deaths per year in the U.S. The Society adds that patient surveys further reveal that 1 in 3 persons will experience diagnostic error. In fact, research indicates that diagnostic error accounts for more malpractice claims than either surgical mistakes or overdose. The Society cites the National Academies of Sciences, Engineering, and Medicine's 2015 landmark report, Improving Diagnosis in Health Care, noting eight main goals to improve diagnosis and diagnostic outcomes in the field of healthcare. These goals may seem like a no-brainer to a patient seeking diagnosis, but they are less obvious to doctors who may have a limited understanding for what the field of medicine needs from them diagnostically. In summary, the goals for improvement are:
- Better professional and patient teamwork in the diagnostic process
- Better education and training in the diagnostic process
- Health information technology that supports the diagnostic process including payment and healthcare delivery systems
- The development of approaches to learn from diagnostic errors
- The establishment of a medical culture that supports the diagnostic process which includes reporting liability and improving diagnosis
- Dedicated funding for research on the diagnostic process and related errors
What You Can Do To Prevent A Misdiagnosis
Hire A Diagnostician
There has been a slow emergence of a new field of specialization called "Diagnostician." One might expect this to look something like Dr. Gregory House on the FOX network series without the theatrical flare. The Southern Medical Association reports that the use of artificial intelligence will play a role in future diagnostics, particularly in enhancing a physician's judgment. There is also a new test for a myriad of cancers. Insurance currently allows screening for only five cancers: lung, colon, breast, prostrate, and ovarian cancers. However, a new test developed by GRAIL called the Galleri hopes to broaden early cancer diagnoses with the ease of a single blood test. The new test is not FDA approved yet, but according to the Cleveland Clinic, high risk or immunocompromised patients can talk with their healthcare provider about ordering the test.
Unfortunately, the American healthcare system cannot boast itself as the best in the world despite the advantages of a democratic and capitalistic society. Until improvements are made in diagnosing conditions early, particularly terminal ones, it behooves a patient to take their own health into their own hands.
Learn How to Use The Information Highway
As my case study revealed, the battle between specialties only resulted in a diagnosis because of my insistence that something more was wrong. I used the Internet to learn that my symptoms had a good chance of being endometriosis and that the ONLY way to diagnose the condition was laparoscopy. I downloaded my research in order to convince my gynecologist that I needed this procedure while demanding that my urologist be simultaneously present during the procedure. Had the laparoscopy been negative, a bladder biopsy via cystoscopy would have then become necessary to rule out a bladder condition. This made sense in order to avoid a second round of general anesthesia and a further delay in diagnosis.
Since this ordeal, I learned that endometriosis and interstitial cystitis OFTEN accompany one another. One would think that both of my doctors would have known this, but neither of them did. There is tremendous truth to the adage that "the best patient is an informed patient."
Trust Yourself Over Conventional Wisdom
Many physician's subscribe to Ocam's Razor, a term that reflects the most logical answer is the correct one. However, a skilled physician in any field is not necessarily a good diagnostician and may therefore, subscribe to Ocam's theory. My own common sense and the Internet enabled me to steer professionals in the right direction, but what does it say about our medical profession that a patient has to steer the doctor in the right direction?
A system replete with specialists does not help render a correct diagnosis when an illness falls outside the realm of any particular specialty. There is insufficient cross-training among practitioners to recognize when additional referrals are warranted. A wholistic approach to healthcare is necessary to understand how all twelve body systems work synergistically together for optimal health. The pressure to keep physician salaries high and medical costs down serves to prolong symptoms for countless patients. Moreover, physicians may unwittingly cause intragenic disease or side effects with the use of contraindicated pharmaceuticals. I am reminded of a friend who suffered from severe neurological symptoms only to learn that several of his prescribed drugs had severe contraindications.
Prevention is definitely the best medicine and far cheaper than chronic diseases like cancer. If you have a gut feeling that something is wrong when your doctor believes otherwise, press the issue. Blood work is sometimes the general practitioner's Bible for diagnosis, but there are countless ailments that do not show up in regular blood work.
Symptoms are the body's way of saying something is wrong, so learn to listen to your body.
Examples of complementary medicine include but are not limited to massage, meditation, biofeedback, reiki, frequency or music therapy, and the most common, use of dietary supplements.
Recognize Alternative Healthcare Methods
My father used to say doctors are called "practicing physicians" because they are practicing on us. In all fairness, I am not discrediting the thousands of dedicated physicians who have saved millions of lives and/or made their patients better. They deserve every accolade for their dedication and expertise. But a medical degree doesn't automatically place one in a heroic category. Misdiagnoses still occur and for the patient, this means being aware of the entirety of their body's signals, symptoms and energy. A basic understanding of anatomy and physiology is better than ambiguity when communicating with your doctor. An understanding of the different types of healthcare and what healthcare insurance will cover is pertinent to making sound decisions in personal healthcare.
Functional Medicine
Functional medicine is a form of alternative care that encompasses unproven methods and treatments. Functional medicine is considered ineligible for course credits in the U.S. since the American Academy of Family Physicians considers some treatment protocols potentially harmful to patients. In my case study, this would include Hormone Replacement Therapy. Conventional medicine would have me take a synthetic hormone like Premarin which at the time was horse urine (today they use yams). Since HRT drugs had serious side effects with long term use, I opted for a bio-identical form of HRT specially formulated by Women's International Pharmacy. I viewed this as safer given the fact I had to take it for 25 years but like all forms of functional medicine, this method of HRT was NOT covered by insurance.
Complimentary And Alternative Medicine (CAM)
Alternative, complementary, integrative, holistic, natural, or new age medicine are terms that are often used interchangeably today. According to Cleveland Clinic, the real difference is how each approach is used. For instance, alternative medicine is used in place of traditional or conventional medicine while complementary medicine is used alongside conventional medicine. Integrative medicine is a holistic approach which also focuses on emotions and mental health. At one point in American history, the lobby for conventional medicine fought hard AGAINST any form of medicine other than its own. However, other approaches to healing developed a powerful lobby of their own and there is now a more favorable attitude toward allowing a patient the freedom to choose the method of care that works best for them. Some conventional facilities are even incorporating complementary methods into their programs and protocols while the issue of insurance coverage may remain a coin toss.
Examples of complementary medicine include but are not limited to massage, meditation, biofeedback, reiki, frequency or music therapy, and the most common, use of dietary supplements. Aromatherapists may utilize reflexology which involves manual pressure to specific areas of the foot, hand or ear which are believed by ancient forms of medicine to correspond to affected organs or body systems. Aromatherapists will recommend essential oils for reflexology and in other energy techniques as well. Cleveland Clinic does an excellent job of giving the patient a preview of his/her options.
Diet And Exercise Really Matter
Another adage worth its weight in gold is "you are what you eat." Indeed, we are! Understanding the benefit of a balanced and nutritional diet is imperative to good health. In a world laced with chemical exposure, it is also imperative to grasp the impact those toxins have and how to cleanse those toxins. Eating a plant-based rainbow-colored diet, adhering to a fast-mimicking diet, and participating in regular detoxes or cleanses is the best thing a patient can do for optimal health.
Sources
https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-us-doctor-medicine-us-md-degree-specialty-2019
https://www.nytimes.com/1993/09/15/us/clinton-seeks-to-regulate-medical-specialties.html
https://www.theatlantic.com/ideas/archive/2022/02/why-does-the-us-make-it-so-hard-to-be-a-doctor/622065/
https://www.improvediagnosis.org/what-is-diagnostic-error/
https://sma.org/ai-in-medical-diagnosis/
https://health.clevelandclinic.org/the-galleri-test/
https://nap.nationalacademies.org/catalog/21794/improving-diagnosis-in-health-care
https://www.independent.ie/life/health-wellbeing/functional-medicine-is-it-the-future-of-healthcare-or-just-another-wellness-trend-37437566.html
https://en.wikipedia.org/wiki/Hormone_replacement_therapy
https://my.clevelandclinic.org/health/treatments/16883-complementary-therapy
This content is accurate and true to the best of the author’s knowledge and is not meant to substitute for formal and individualized advice from a qualified professional.
© 2009 Vicki Carroll