Hand And Arm Transplantation Restorative Surgery

Upper Extremity Transplants
Transplants have been around now for decades and few of us even blink when we hear about them. However, extremity transplantation is something quite different than the usual transplant. Organ transplants are performed because there is no alternative. Without a transplant, a patient will die.
Extremity transplants on the other hand are termed restorative procedures because the main goal of these transplants is not to save a patient's life necessarily but to save his or her function--or return the patient to normal function.
Also unlike organ transplants, which in some cases use cadaver organs, extremity transplants must obviously come from deceased donors--who will no longer be able to use his or her arms.
While this article deals with upper extremity transplantation, many of the techniques and especially the new protocol in place pertain to other vascularized composite allograft (VCA) transplants such as lower extremity transplants and face transplants.
How many upper extremity transplants have been performed to date? Approximately 85 to 90 of these very delicate, incredibly technical transplantations have been performed since the first one in 1998 in France. However, what's incredible to this author is that in this relative short span of time, there have been some amazing advances that could spell huge developments for this type of transplantation (but more importantly for other types) for decades to come.
We'll look at four inspiring individuals, their history and how they became involved with this pioneering new medical therapy.

Why Transplantation Instead of Prostheses?
While an arm or a hand prosthesis is a step above amputation for most patients who have suffered the loss of a limb, a prosthesis can never replace a human body part. Most prosthesis wearers will agree that a prosthesis is a step to returning to normal function but it lacks certain elements. Why?
- There is no sensation with a prosthesis - the wearer can never actually feel something hot or cold, soft or hard, wet or dry - like a tear.
- Most prosthesis wearers use the prosthesis as a stabilizer - meaning it is not an active arm or hand in that it cannot scoop up hair for a ponytail but instead can hold the hair in the prosthetic grasp while the other "real" hand feels and does the job. Imagine if you had no "real" hands or arms.
- No matter how sophisticated a prosthetic is, it can't replace the motor function of a natural limb.
- What if a person has lost both limbs? Double prostheses can help someone get from here to there and perform activities of daily living, which is an improvement - but it isn't restoring the person to their normal level of function.
- The psychological impact of losing a limb for any reason is daunting enough. Having to deal with prosthetic limbs can be overwhelming to people no matter how much they want to return to normal and how much "better" their functionality becomes or seems to others.

Who Qualifies for Extremity Transplantation?
- People with congenital absence or severe deformity of limbs
- Patients who have lost an extremity or extremities due to trauma
- Burn injuries can be a common cause for amputation and limb loss
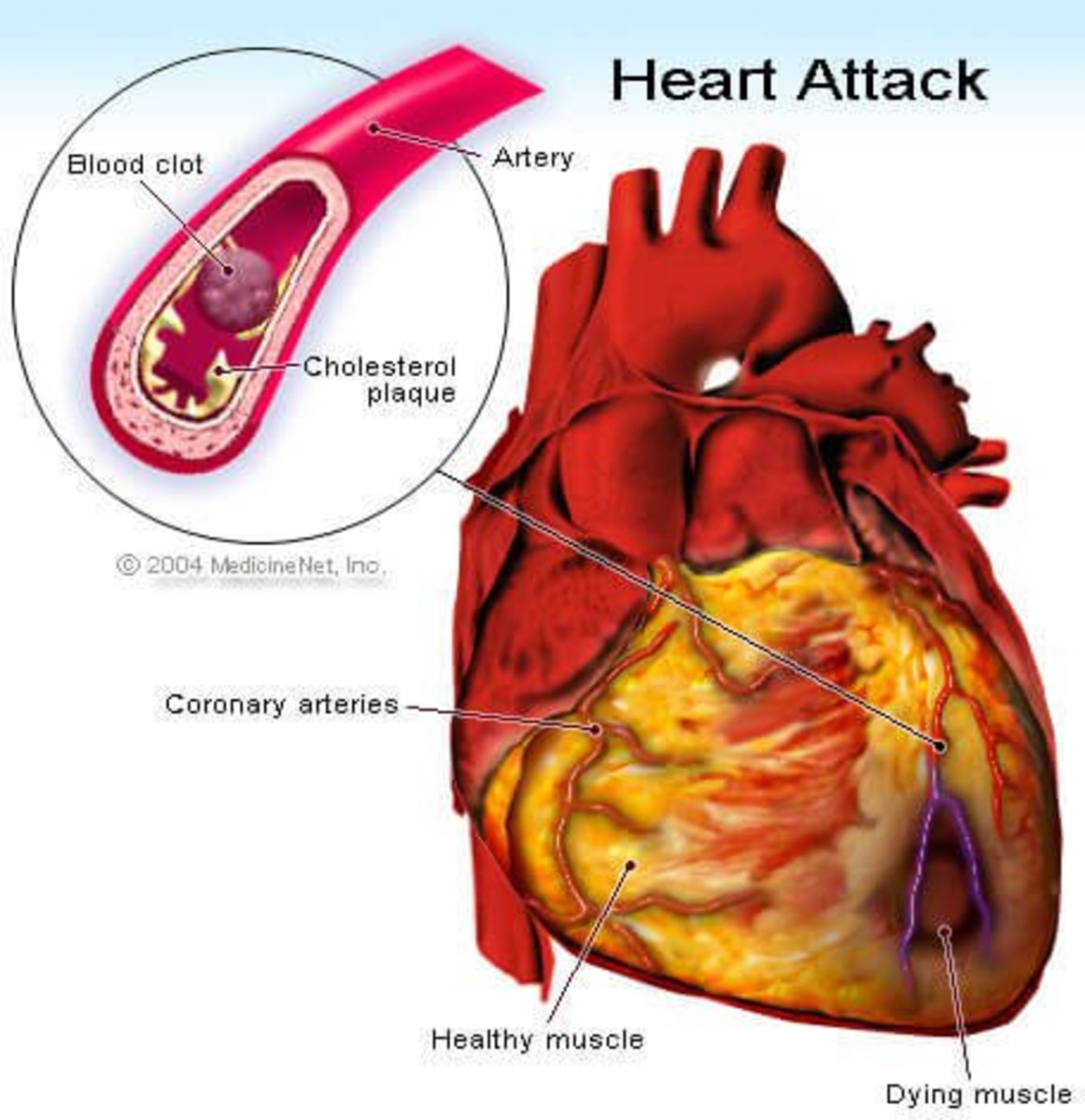
- Medical conditions such as sepsis, diabetes, Strep infections or other systemic illnesses that lead to amputation in otherwise healthy individuals
- People who have had little to no success with prosthetic limbs - surprisingly many are extremely painful to use and an estimate is that more than 50% of people with prosthetics do not use them for one reason or another
Who Does Not Qualify for Extremity Transplants?
- Someone who has lost their arm from the shoulder down - there needs to be part of the arm intact to receive a transplant of an arm or hand
- Someone who has lost fingers alone (not part of the arm itself) would not qualify for this kind of transplant
- Most experts agree there are some age limitations, however, in several cases, the age has been over the number quoted in most studies
- Life-threatening illnesses such as cancer, HIV, etc. would preclude anyone from receiving a transplant
- Even though extremity transplants are not life saving in nature, due to the number of people waiting for them, the hope is that the transplant will go to someone who will live many years and enjoy improved functionality as well

Retired Master Sgt. Janet McWilliams lost her hand in combat when a package bomb exploded in her office. In 2010, she was the tenth person and the first woman to receive a hand transplant.
The surgery was performed in March 2010 and was the first performed in a Defense Department facility by a team of civilian and Defense Department physicians.
Within two weeks after the surgery, McWilliams was able to move her thumb and fingers.
Perhaps the most remarkable take-away from this story in particular was her wish that this would be a breakthrough for other combat victims.
Double Hand and Arm Transplantations
In October, 2011, a combined team of more than 40 surgeons and other healthcare professionals performed surgery on Richard Mangino. He was a 65-year-old male who had lost both arms below the elbow and also both legs below the knee following systemic sepsis and its complications in 2002. This surgery was done at Brigham and Women's Hospital and the procedure lasted more than 12 hours.
Later in 2012, this remarkable story followed Mr. Mangino who was now able to play tunes on his guitar, mow the lawn, drive and throw a football on the beach with his grandchildren.
The transplant teams at BWH are planning surgery later this summer on another quadruple amputee who lost all four limbs due to a Strep A infection after giving birth. Katie Hayes, whose daughter is now 2 years old, stated the price of these surgeries to the CNN interviewer as between $60,000 and $200,000.
In the interview, Katie speaks ardently about her desire to just return to doing the normal things with her hands and arms that we all take for granted. This illustrates quite poignantly how these types of transplantations differ from other transplants and how they are all about functionality and returning someone to a normal way of life.
First Solder to Receive a Double-Arm Transplant
Last but perhaps most remarkable of all, Brendan Marrocco is the first soldier to survive a double-arm transplant. Brendan was the victim of a roadside bombing in Iraq in 2009, a scenario in which he lost both arms and both legs. He received a double-arm transplant in late 2012. However, most notably, he also received a bone marrow transplant later from the same deceased donor. This is groundbreaking therapy in terms of survival for transplant recipients and a treatment which could lead to incredible breakthroughs in terms of other transplanted organs and composite grafts.
Brendan's operation was performed at Johns Hopkins. His was only the seventh double-arm transplantation to be performed in the US. There have been four additional patients who underwent the same type of transplant and all are doing well. All five of these patients received bone marrow transplants along with the extremity VCA transplants.
All recipients are doing extremely well and all are on the same less toxic single-drug anti-rejection medication protocol called Immunomodulatory Minimization Protocol or IMP. This therapy protocol for transplant recipients means that patients will undergo a bone marrow transplant after their transplantation surgery - the bone marrow taken from the same recipient as their limbs. This equates out to less graft rejection and less need for aggressive immunosuppression, which in many cases has led to premature death due to side effects like cancer or organ failure. These side effects have been known to be due to the toxicity of anti-rejection medications. To many, the single-drug therapy could mean not only return to a normal functional state but also long-term survival since most transplants are considered a means to extend someone's life in the short term.
Future of Upper Extremity Transplantations
With an estimated 300 soldiers alone having lost a hand or an arm in worldwide conflicts, there is a tremendous need for upper extremity donors. Many people think that simply checking the organ donor box on your driver's license means that your body would also be a donor for other tissues such as extremities or facial transplants. In fact, this is not the case.
Extremity and other VCA graft transplants must be procured in a time-sensitive fashion (usually within 4-12 hours of death) and their donation must come from family members. It can be a very sensitive issue for some families to consent to having their loved one's visible body parts removed, however, the gift of these transplants is obviously priceless.
The surgeries themselves are mind boggling in their expertise - attaching blood vessels, nerves, bones, tissues and tendons. The talented medical staff who perform them are technical wizards.
After surgery, the patient's work has just begun as it becomes the rehab team's job to get the patient's new limb or limbs moving, usually within 24-48 hours. Therapy for a transplanted hand or upper extremity is roughly 6 hours per day 5 days per week for at least 1-2 years. It's a full time job. It is said that nerves regenerate at 1 inch per month in the VCA patient's transplanted limb but most begin to feel and have movement soon after surgery.
These are just a few of the incredible stories about transplantation. Look to the future to see further advances and more medical miracles for those needing transplants to not only save their life but return them to a functional way of life.