Herpes Zoster (Shingles): Clinical Presentations, Complications, Diagnosis And Treatment
Shingles Presenting In Herpes Infection

Infectious Diseases
Clinical Manifestations And Complications Of Herpes Zoster
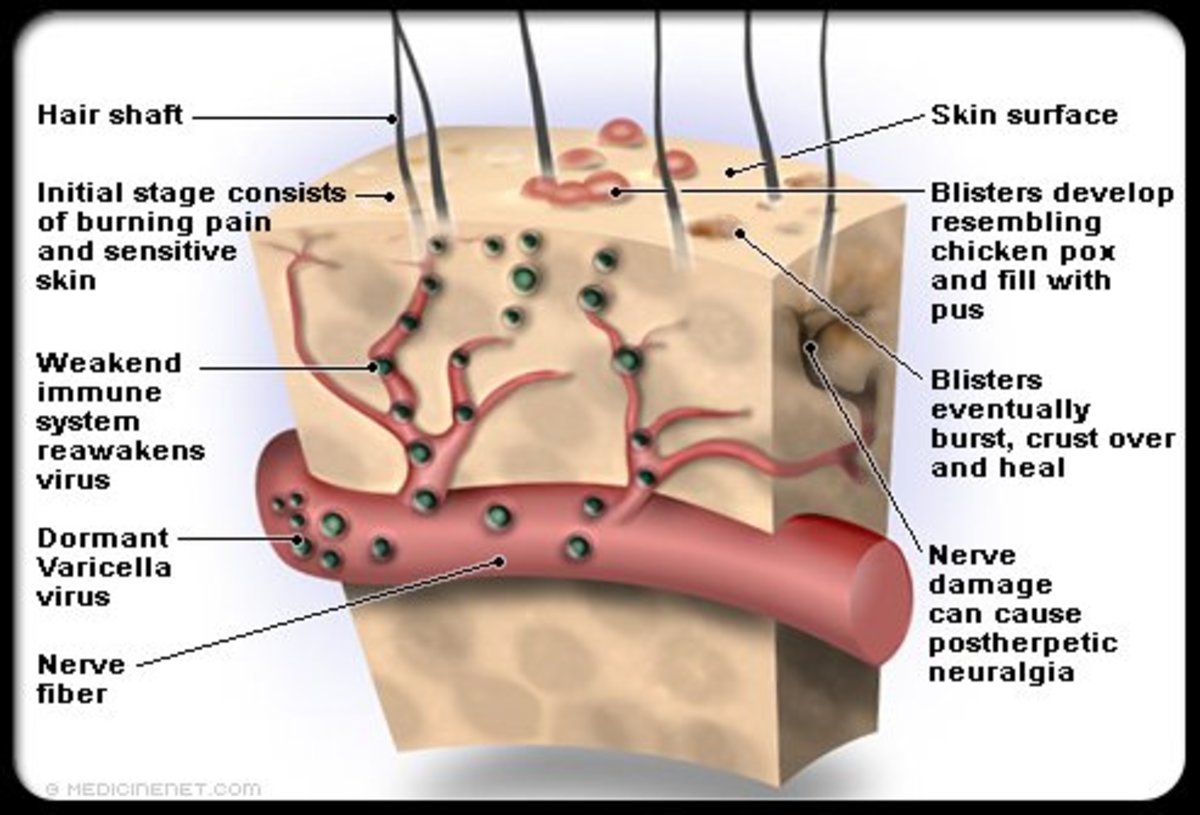
Herpes zoster is an acute eruptive disorder characterized by painful radiculitis and vesicular eruptions in the corresponding dermatomes. It is seen more commonly in subjects above the age of forty years. Chickenpox and herpes zoster are caused by the same virus, the later occurs in persons who have acquired partial immunity. The virus remains dormant in the posterior root ganglion and activation occurs due to factors which are not clearly known. Attacks of herpes zoster are often precipitated by immunodeficiency states, hematological or neurological malignancies or trauma.
Clinical Manifestations
The eruption has an abrupt onset after a prodromal illness characterized by malaise, fever and severe pain in the corresponding dermatomes lasting for 3 to 4 days. The pain may be lancinating, deep-boring, burning or vague and in many cases it is unbearable. The common sites for the eruptions are the ophthalmic and maxillary divisions of the trigeminal nerve, geniculate ganglion of the facial nerve and thoracic and abdominal nerve roots. After a variable period of pre-eruptive neuralgia, the rash begins as reddish papules which soon develop central vesiculation. The vesicular fluid becomes turbid in three days and crust formation occurs after a week. The rash may involve a whole dermatome or only parts of it. The eruptions seldom cross the midline. With the formation of pustules the initial pain may subside, but in many elderly patients it may persist in the same form or in an altred form for months or even years. This is referred to as post herpetic neuralgia. Vague paraesthesiae, varying degrees of sensory loss and even lesser degree of motor loss may persist over the affected segments for considerable periods. In general the condition is benign, but the development of neuralgia may lead to severe distress and even suicidal tendencies in susceptible subjects. Incidence of post- herpetic neuralgia is more in elderly subjects with severe prodromal symptoms and painful confluent lesions.
Complications:
- Secondary infection: The vesicles may be infected by bacteria, giving rise to fever. Deep scarring may occur.
- Ophthalmic herpes: Corneal scarring may develop in herpes involving ophthalmic division of the trigeminal nerve. Optic neuritis and oculomotor palsy may occur less commonly.
- Herpes of the geniculate ganglion presents as facial nerve palsy and vesicles over the ipsilateral external auditory meatus (Ramsay-Hunt syndrome). Genrally the facial nerve palsy tends to persist.
- Paralysis of muscles corresponding to the involved spinal segment is a rare sequel. Encephalitis and myelitis have been reported rarely.
- In leukemic subjects and those on immunosuppressant therapy extensive vasiculation may develop (generalized herpes).
Diagnosis and differential diagnosis: Once the eruption has occurred over the sensory root distribution, diagnosis becomes easy. Before the onset of the eruption, the pre-herpetic neuralgia may be mistaken for other serious conditions depending on its location. These include trigeminal neuralgia, vascular headache, painful ophthalmic problems, myocardial infarction, pleurisy, cholecystitis, appendicitis or any surgical abdominal emergency. Careful examination of the part in bright light may show at least erythematous rashes in many cases and this should suggest the diagnosis.
Even in cases with clearcut diagnosis, an attempt should be made to bring out an underlying malignancy like lymphoma or carcinoma, especially in the elderly subjects.
Local Treatment Is Sufficient In Treating Herpes Zoster

Treatment Of Herpes Zoster
Local treatment consist of keeping the area dry and clean. Analgesics like aspirin and dextropropoxyphene are required in the eruptive stage. A short course of ACTH or prednisolone has been recommended in the elderly patients with a view to prevent post herpetic neuralgia. Opinions are divided on this issue. The risk of dissemination of infection is a real danger. Antiviral drugs like vidarabin or acyclovir have been employed. These drugs are given in a dose of 5 mg/Kg body weight/day parenterally for two days. This has to be considered in those with poor general condition or those on immunosuppressant therapy. The most troublesome complication of herpes zoster is post-herpetic neuralgia. The pain is often refractory to analgesics. Diphenylhydantoin (300 to 400 mg/day), carbamazepine (200 to 1000 mg/day) and tricyclic compounds (amytryptaline, imipramine, doxepine) have been used with some benefit. Other therapeutic modalities like transcutanoeus nerve stimulation (TNS) have benefited some patients.
© 2014 Funom Theophilus Makama