Histoplasmosis And Cryptococcosis: Etiology, Pathology, Clinical Manifestations, Diagnosis, Prognosis And Treatment
Disseminated Lesions Of Skin Manifested In Histoplasmosishttp

Etiology Of Darling’s Disease Or Cave Disease
This is caused by inhalation of Histoplasma capsulatum. This infection is worldwide in distribution but maximum number of cases have been reported from the west, especially the USA. Limited studies show that the infection is present in India. Histoplasma capsulatum is seen in soil enriched by the droppings of birds, especially fowls. When the spores are inhaled, yeast-like forms develop in tissues. It grows as a mould in its natural habitat and in vitro.
Pathology: The lesions are granulomata produced in several organs. Reticuloendothelial organs, lungs, adrenals, brain and other tissues may be affected. Lesions may resemble tuberculosis. Healing occurs with calcification. Cerebral lesions can be mistaken for those of cerebral thrombosis or hemorrhage.
Clinical Presentations
The majority of cases are asymptomatic. Pulmonary lesions may resemble different types of tuberculosis. Common manifestations include fever, cough, hilar adenopathy, penumonitis, apical infiltrates, fibrocavitary lesions and the subpleural solitary pulmonary nodules. Scattered military calcification may develop in disseminated histoplasmosis. Other manifestations include mediastinal syndrome, uveitis and adrenal insufficiency.
Disseminated histoplasmosis: Fatal disseminated histoplasmosis may develop in persons who harbour the infection and who receive corticosteroid therapy. Lesions occur in the liver, spleen, bone marrow, lymph nodes and adrenals. Clinical features include fever, hepatosplenomegaly, generalized lymphadenopathy and mucocutaneous ulceration.
Diagnosis
X-ray chest shows the pulmonary lesions. Delayed hypersensitivity test using histoplasmin is helpful in diagnosing past infection. The test shows cross-sensitivty with other fungi. It is more useful for epidemiological studies to determine the prevalence of histoplasmosis in the community. Its use in the diagnosis of individual cases is limited. Complement fixing antibodies are detectable in the serum and these, being more specific, are useful in diagnosis. Diagnosis can be confirmed by demonstrating the fungus in tissue biopsies or other suitable material.
Prognosis: Histoplasmosis is generally benign. In immunosuppressed individuals, complications are more.
Treatment: Specific treatment is not indicated in asymptomatic cases. In disseminated disease and in chronic pulmonary lesions, intravenous amphotericin B, given for 10 to 12 weeks is curative. Persistent cavities and mediastinal fibrosis may necessitate surgery.
Physical Presentations Of Blastomycosis

Infectious Diseases
Torulosis, European Blastomycosis, Busse-Bushke’s Disease
Infection by Cryptococcus neoformans leads to a clinical picture of subacute or chronic meningoencephalitis commonly. Sometimes, the infection becomes generalized and lungs, skin, bones and viscera may be involved. The fungus is present in nature especially in soil contaminated by the droppings of birds like fowls and pigeons.
Etiology: Cyptococcus neoformans is a yeast-like fungus, distributed all over the world. In tissues, it remains encapsulated in a polysaccharide capsule. Infection in majority of cases is subclinical, but generalized disease occurs, in immunologically deficient subjects.
Pathogenesis and pathology: It is probable that the fungus reaches the lungs by inhalation. The pulmonary lesions tend to heal spontaneously without becoming symptomatic. Histologically, the lesions range from mild inflammatory reaction to definite granulomas. Intracranial infection leads to basal meningitis. The organism reaches the meninges by the blood stream.
Clinical Features
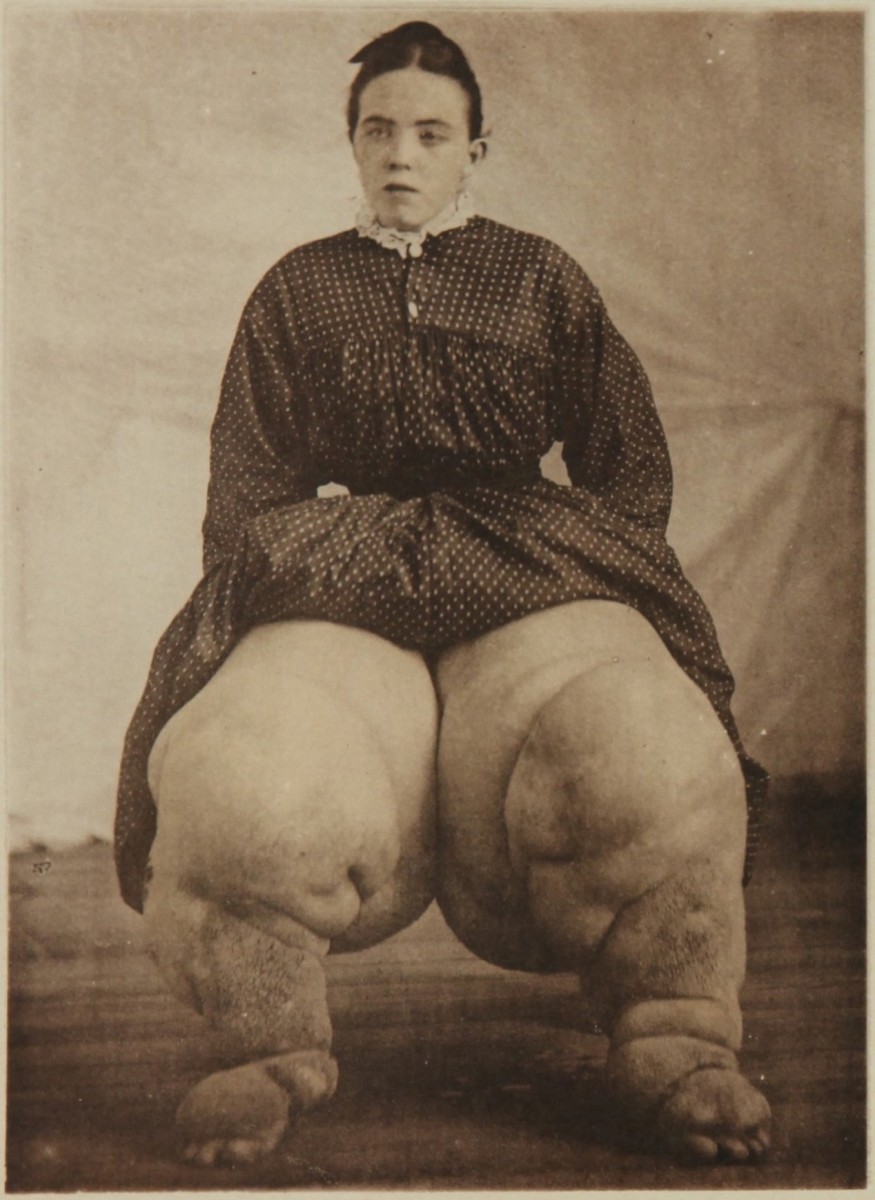
The pulmonary involvement may be subclinical. It may be detected during routine investigation or accidentally, as inflammatory or tumour like lesions. Often these lesions are mistaken for tuberculosis. Meningoencephalitis closely resembles tuberculous meningities. Papilledema and cranial nerve palsies occur in some cases. The course is prolonged with remissions and exacerbations. Papular or suppurative lesions occur in the skin in 10% of cases. These ulcerate and discharge hairy material containing the fungus. Other viscera such as liver, pericardium and endocardium may be affected.
Diagnosis: Diagnosis is confirmed by finding the encapsulated fungus in the sputum, urine, tissues and cerebrospinal fluid. The fungus can be cultured and identified. The encapsulated organism can be demonstrated in the CSF by microscopic examination after mixing with a drop of India ink. Serological tests like complement fixation and latex agglutination are available, but being nonspecific, they are not of great help.
Treatment: Cryptococcosis of the CNS is treated with fluocytosine, given 150 mg daily orally in four divided doses or intravenous amphotericin B. Amphotericin B is started in a daily intravenous dose of 10 mg in a drip as the initia dose and it is increased to 50 mg/day to reach a total dose of 2g. Mild toxic effects include nausea, vomiting, chills, fever, headache and malaise. The drug is nephrotoxic and increase in blood urea is a contraindication for further therapy.
© 2014 Funom Theophilus Makama