How HIV Attacks the Immune System

The fear of HIV infection develops into AIDS is one of the most alarming thoughts HIV-infected person could ever imagine. From the knowledge of the consequences of debilitating action of HIV to immune system, the presence of opportunistic infections proves to be more devastating.
With the diminished strength of body to fight the infections, HIV-infected person can acquire different infections at the same time. It could be brain diseases (meningitis), lung diseases (tuberculosis), skin diseases (Herpes), or even a rare type of cancer like Kaposi’s sarcoma at the same time. These pathogens can ravage the body without mercy.
In able to understand more how HIV attacks and destroys the immune system, substantial knowledge on how immune system responds to destroy pathogens (except HIV) is necessary. Numerous researches and strategies to eradicate HIV are very promising and opt to look forward.
What to know...
How to know how HIV can destruct immune system?
The Body's Immune Response against Microorganisms
The body’s immune system has the ability to protect from invaders like bacteria, viruses, parasites, or other foreign body tissues. These microorganisms consist of antigens (proteins) located on their cell surface. The body cells have also antigens called human leukocyte antigens (HLA), which are also found on cell surface, but the immune system recognizes HLA as self and does not react towards it. The body's capability to recognize antigen as foreign and harmful elicits immune response and destroys substances that contain antigen or antigen fragments.
There are two types of immunity provided by the immune system to fight against diseases: the innate (nonspecific) immunity and adaptive (specific) immunity.
Innate immunity is the first line of defense against all invaders; all normal persons possess this kind of immunity. Examples of these barriers against pathogens are: impenetrable skin unless it has membrane breakage; hydrochloric acid and enzymes secretion of stomach; flushing action and enzymes content of tears and saliva; sticky mucus which traps microorganisms; sneeze and cough reflex which eject pathogens and non-living things from respiratory system.
If an invader gets cross through these barriers, other cells of immune system develop adaptive immune defense to destroy the invader.
Body's Immune Response
Antigen Presenting Cells
Immune cells like macrophages and dendritic cells engulf and ingest the pathogens, and then place some of its antigen fragment or antigen protein on cell surface. These cells are called antigen presenting cells (APCs) since they present the antigen fragment as an alarm or marker for other immune cells to attack and take its action.
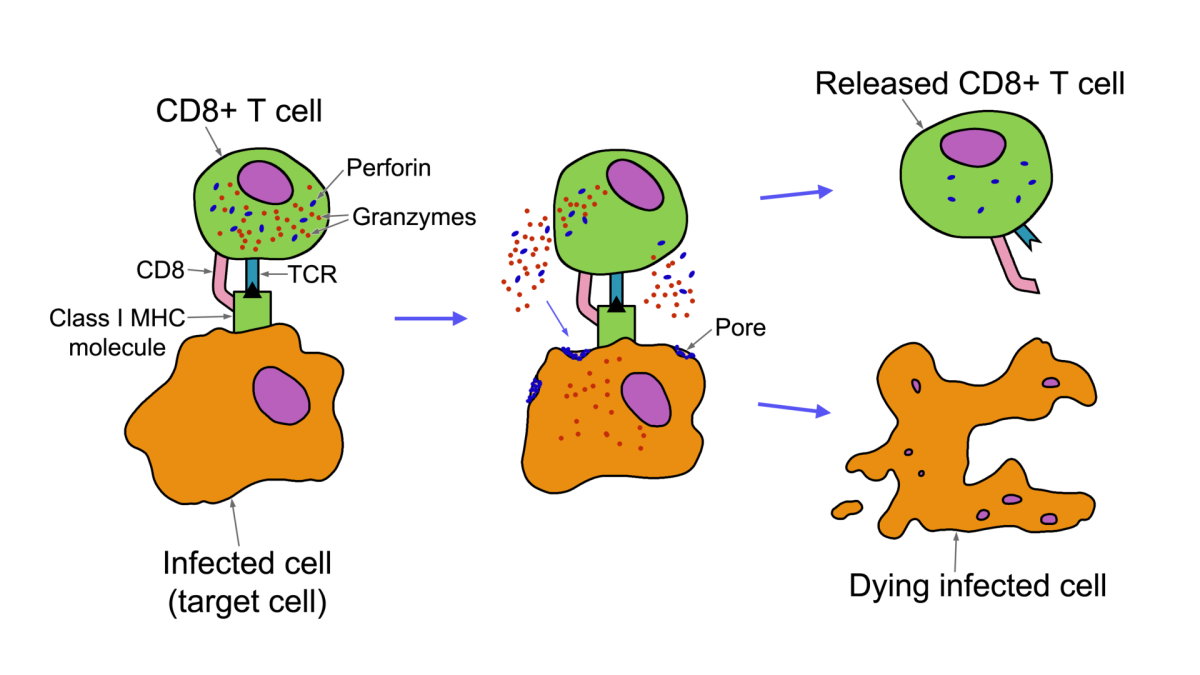
APC also has also the capability to send signals by releasing a group of cytokines (chemicals) called interleukin that can activate the natural killer cells. Natural killer cells are important in the recognition and destruction of virus-infected cells and malignant cells. They contain intracellular granules (filled with protein) that cause pores in the cell membrane of target cell, which lead to apoptosis or cell suicide.
Furthermore, APC presents the antigen to T lymphocytes. There are specific T cells coated with different chemical molecules on their surfaces and their distinction are aided by the term called “cluster of differentiation” or CD.
The Helper T cells (CD4) are T cells containing CD4 molecular markers on their surface. Once triggered by the APC to differentiate and proliferate, helper T cells produce two functions:
(1) release cytokines that activate the macrophages and cytotoxic T cells to explicitly eliminate the pathogens.
(2) release another group of cytokines that send cues to B cells to release antibodies towards antigens.
Cytotoxic T cells (CD8) are T cells containing CD8 molecular markers on their surface and destroy the infected cell showing antigenic proteins on its surface. They release cytotoxin that lyses the cells;
B cells, when sensitized and primed, produce clones and secrete antibodies in response to the alarm received. These antibodies attach and bind to antigenic protein and mark the antigen for other cells like macrophages to promote phagocytosis. The activated macrophages capture, engulf and destroy the antigen together with the attached antibodies. In addition, the antibodies can also disrupt the antigen cellular membrane and lyse the cell.
When the infection subsides, Suppressor T cells (or regulatory T cells) down-regulate the function of immune system by signaling it to rest—since the continuous activation of immune response may harm body’s own healthy cells.
Once the same pathogen invades again, according to Medical Immunology book (sixth edition) by Gabriel Virella, two unique characteristics of immune response under adaptive immunity will be at work:
- Respond only to specific type of invader
- Remember the same antigen encountered. The capacity to destroy that pathogen is higher and swifter compared to the previous exposure.
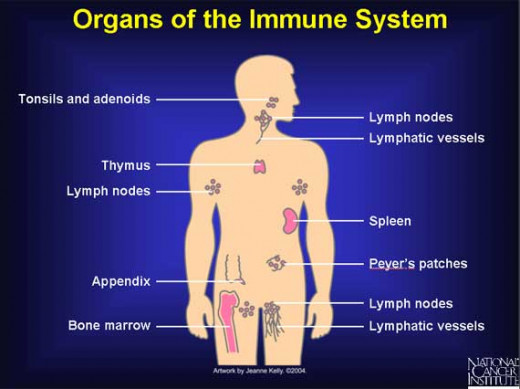
Mature lymphocytes travel through blood to lymphoid organs then circulate into blood again to assure the body is free from any invading substances. These are the amazing facts how body was intricately made and how efficient it is to protect against invading microorganisms. But then, these are also the same cells HIV attacks.
According to National Institute for Allergy and Infectious Diseases, there are different ways how HIV ravages the immune system :
- killing cells directly
- apoptosis (cell suicide)
- destroying innocent bystander cells
- destructing immune precursor cells or young cells that will develop into mature cells which are adept to perform immune function.
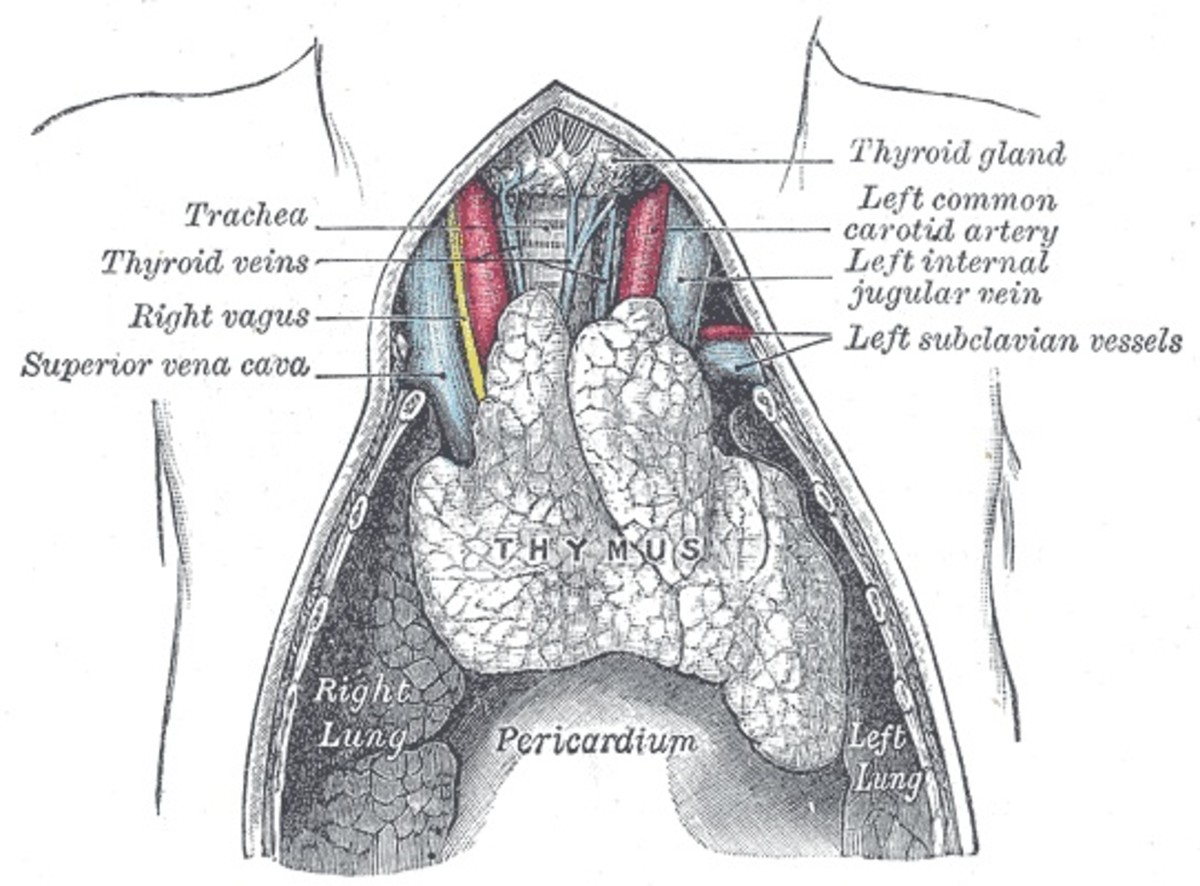
- damaging the bone marrow and thymus where B and T lymphocytes mature.
Have you imagined a defense system without each member's function?
How HIV attacks the immune system
HIV is made up generally of viral envelop, which composed of glycoproteins (gp120 and gp41) used for attachment and fusion to the receptors found on the surface of the host cell; two single-stranded viral RNA which contain viral genetic code and instruction for viral replication; enzymes and other viral proteins which are necessary for efficient generation of new HIV cells.
HIV doesn't attach to any type of body cell. It requires a receptor to be able to bind to host cell—the CD4. CD4 is one type of glycoprotein found on the surface of helper T cell, regulatory T cell, monocyte, and dendritic cell.
HIV Attack Mechanism:
- Through glycoproteins from viral envelop, HIV merges to the receptor or co-receptors on the surface of the host cell (mainly on the helper T cells).
- HIV releases its contents in the host cell like HIV RNA, enzymes (reverse transcriptase, integrase, protease), and other viral protein.
- Viral RNA converts into viral DNA through enzyme reverse transcriptase
- Viral DNA integrates into host DNA through enzyme integrase.
- Integrated viral DNA produces new viral RNA and proteins.
- New viral RNA and viral proteins assemble into an immature HIV cell through enzyme protease until it matures making the new HIV ready and competent to infect another host cell.
Long-live HIV!
HIV can establish a latency period in an individual T cell. What does it imply? When CD4 T cell becomes infected with HIV but manages to survive, the cell goes back to resting memory state and becomes the resting reservoir for HIV. Even though HIV is unproductive and nonfunctional in the resting state, neither it is killed nor destroyed, the HIV competent-genetic code for replication remains unharmed (though contained).
What’s even more distressing is that HIV reservoir is considered to be the major hindrance in curing HIV disease—because the latent virus residing in resting cell is inaccessible by Highly Active Antiretroviral Therapy (HAART), the standard treatment for HIV infection used today; and maintains state of invisibility to immune defense. These two factors significantly take account why HIV is considered a life-long disease.
Furthermore, the latent viruses can reactivate, and thus, re-perform the massive destruction of immune system.

A Study to Eradicate Long-lived HIV
On-going research, conducted by AIDS Research Alliance, proposed eradication strategy to eliminate the HIV reservoir for those infected persons under antiretroviral therapy (ART)—destroying HIV reservoir can possibly make way to total elimination of HIV in the body.
Reactivation will result in expressing the virus through the use of activating agent called prostratin. Prostratin is a non-tumor-promoting phorbol ester found on Mamala tree. A similar study posted on Journal of Virology has strengthened the confirmation made by the AIDS Research Alliance regarding the dual role of prostratin: (1) inhibits infection of CD4 lymphocytes; (2) reactivates latently CD4 infected cells.
If CD4 cells infection will be inhibited and if all latent CD4 infected cells will be activated and be productive again (by the combining efforts and functions of immune system and HAART), this proposed strategy can, perhaps, lead to all HIV controlled and sooner destructed. Looking forward for the progress of this research is a must.

A time will come
Understanding how the body is beautifully made and how this body can be destroyed by a microscopic virus in such a very short time is not hidden anymore. Acceptance of this fact can lead to a more strengthened and will-powered person capable to live happily.
Profound studies commence from the knowledge how immune system works and how HIV attacks the immune system. From then on, there are many promising in-progress researches develop throughout the years. Time will come when HIV infection will not be considered a life-time disease anymore and the crusade for an AIDS free generation will be at hand.