How to Tell if You Have Had An Eye Stroke
Anterior Ischemic Optic Neuropathy (AION) is a devastating disease that occurs in the middle aged and the elderly. It damages the optic nerve, and thus is called, 'a stroke of the optic nerve. Little warning is given as it strikes one eye, and can progress to the other eye later. A stroke of the optic nerve is not related to a stroke occurring in the brain so is not accompanied by any weakness or paralysis.
The Optic Nerve and its Role
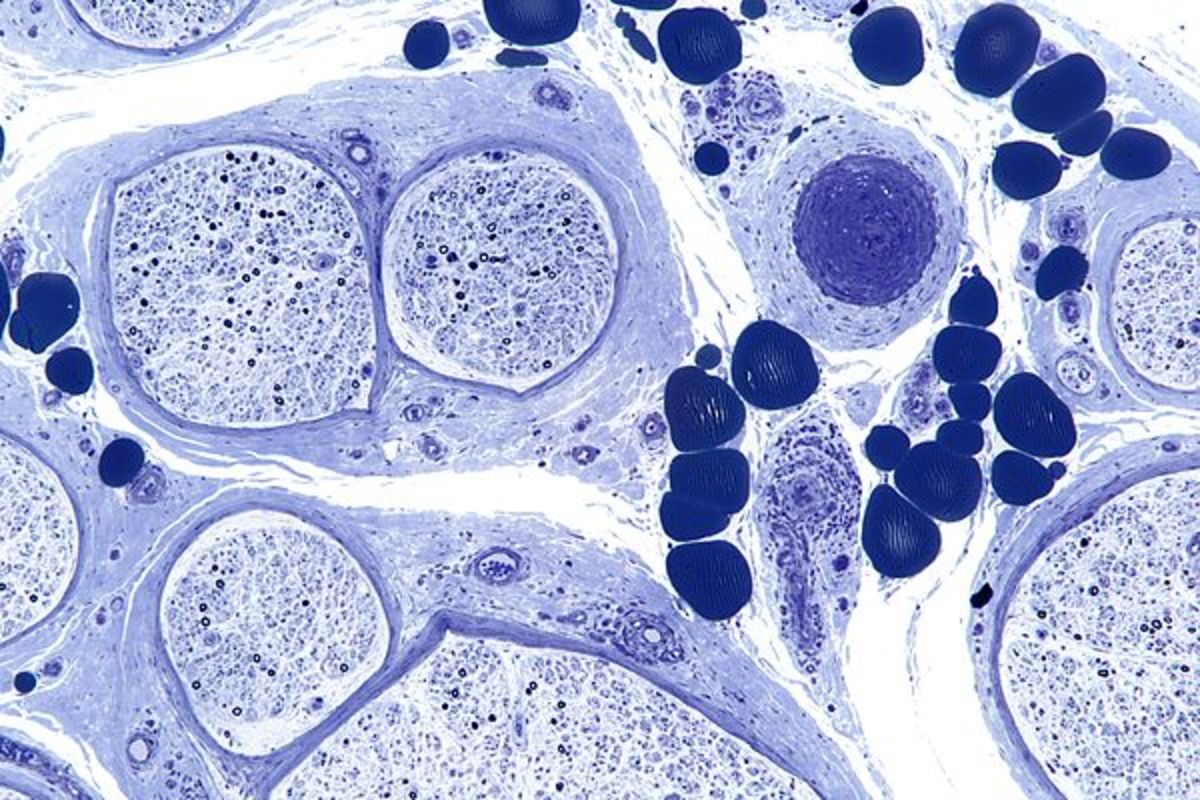
The optic nerve can be seen at the back of the eye in an examination by the Ophthalmologist. It is made up of millions of nerve fibers, and blood vessels which nourish the optic nerve with blood and nutrients. In a healthy optic nerve messages are sent to the brain resulting in vision. When the optic nerve is damaged, or its circulation is cut off, distortion or no vision is the result. How much vision is lost depends on how much damage to the optic nerve there is.
Ischemia's Two Types of Optic Neuropathy
ischemia, is a restriction in blood supply to tissues, causing a shortage of oxygen and glucose needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, resulting in damage to or dysfunction of tissue.
There are two types of Ischemic Optic Neuropathy depending upon which part of the optic nerve is affected.
Anterior Ischemic Optic Neuropathy (AION)
This is caused by acute ischemia of the front(anterior) part of the optic nerve which is supplied by the posterior ciliary arteries.
Posterior Ischemic Optic Neuropathy (PION)
This is a less common type, and is caused by acute ischemia of the back (posterior) part of the optic nerve located behind the eyeball and this part is not supplied by the posterior cilia arteries.
AION has two types depending on what causes it, Arteritic AION which is a serious type and is due to a disease called Giant Cell Arteritis or temporal arteritis. The second type is Non-arteritic AION a more common type with different causes but not associated with giant cell arteritis.
How AION is Diagnosed
The doctor will ask you some vital questions to determine which AION you have. In Non- Arteritic AION he may ask these questions to rule out non-arteritic AION. Painless, loss of vision due to AION may be the first symptom or complication of other diseases.
-
Was the vision loss sudden or gradual? If sudden what time of day was it discovered.
-
Any blurring or loss of vision before the actual vission loss, has it been stable since first discovering it, or improved or worsened.
-
Are you diabetic?
-
Any heart trouble, stroke, high or low blood pressure, or shock, recent heart surgery, cataract surgery, any excessive bleeding?
-
Any family history of glaucoma?
Do you smoke, are you on any high blood pressure medication, if yes, which drug, how often and what time of day do you take it?
-
Are you on any birth control pills, or estrogen pills?
Giant Cell Arteritis AION is a medical emergency because of the complication of visual loss in one or both eyes, which is preventable if diagnosis is early and treated immediately and aggressively with corticosteroids. This disease strikes those over 50 years or older, and is more common in women than men.
Eighty percent of persons with Giant Cell Arteritis will have felt unwell for some time. Twenty percent have no general symptoms and are healthy. Some patients experience, 'euphoria or well-being,' while they are unconcerned about their vision loss and may insist they see well when it is clear they can't. They may even refuse treatment so it is important for family support to convince them they need help.
Signs to Look For
If Giant Cell Arteritis is present the physician will want to know about these problems.
- Pain while chewing food, loss of appetite, weight loss, pain in the temples and neck
-
Scalp tenderness, headaches, fatigue, sleepiness, muscular aches and pains
The ophthalmologist needs to know how much the patient can see at every visit, to see if any changes have occurred. Plus reading the eye charts for distance and near visual acuity, the patient will often have visual field testing.
Visual field testing:
This test measures both straight ahead and side vision. A defect in the visual field test shows which optic nerve fibers are affected by the disease. A normal eye (20/20) visual acuity can have visual field loss in the periphery, so a normal visual acuity does not determine no visual loss.
Relative Afferent Pupillary Defect
The pupil of the eye gets larger and smaller according to the amount of light, the optic nerve reacts to light. If the pupil is constricting to light less than normal it shows there is damage to the optic nerve. Pupils are tested by shining a light into each eye causing them to constrict, as the light is moved between the eyes the pupil should constrict to the same size. If this doesn't happen then a relative afferent pupillary defect is present in the affected eye.
Glaucoma Testing
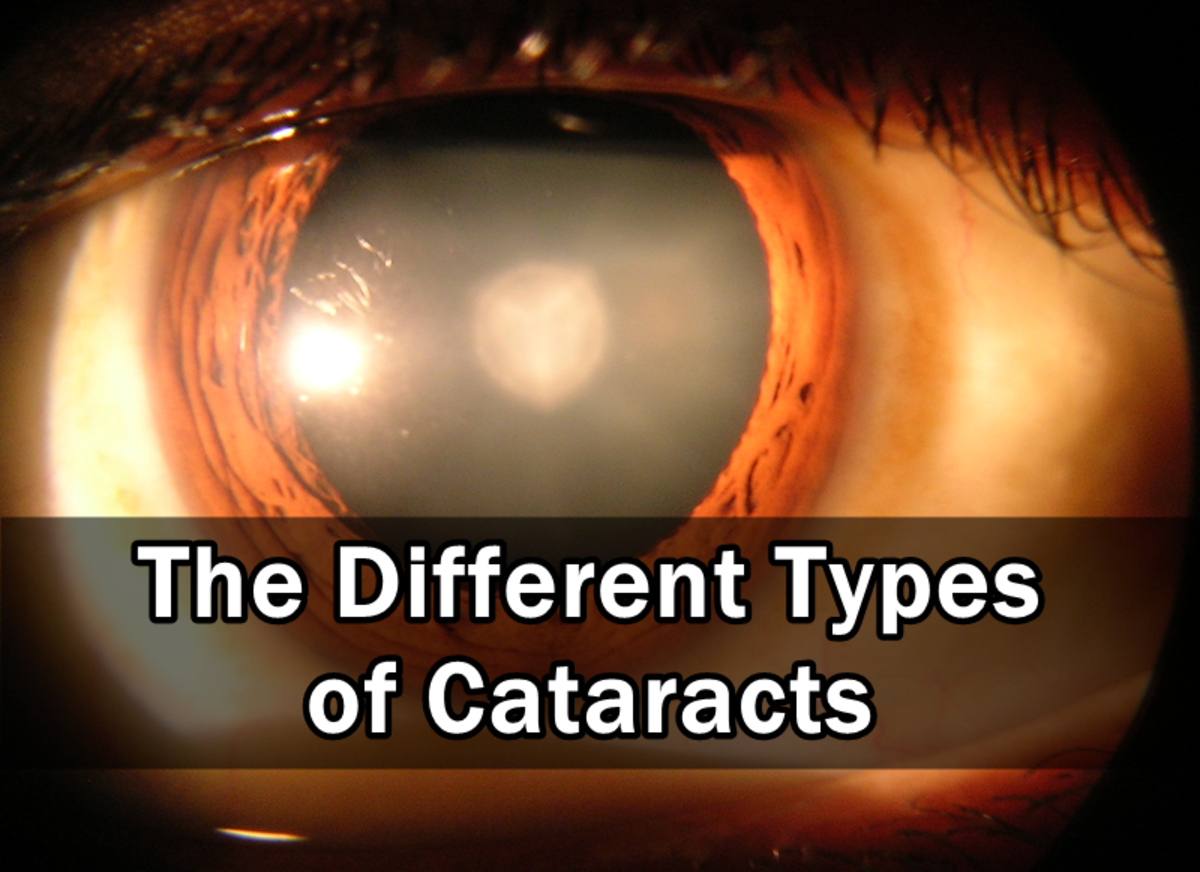
Pressure in the eye is measured with a tonometer, it is a painless procedure that is essential to obtain information about the circulation in the eye. A person may not know they have high pressure in the eye until they have experienced visual loss.
Fundus Photograph and Fluorescein Fundus Angiography
This is a routine dye test to determine the state of circulation, or the amount of swelling in of the optic disc and its resolution.