Israeli Breakthrough Offers Hope for Corneal Transplant Patients

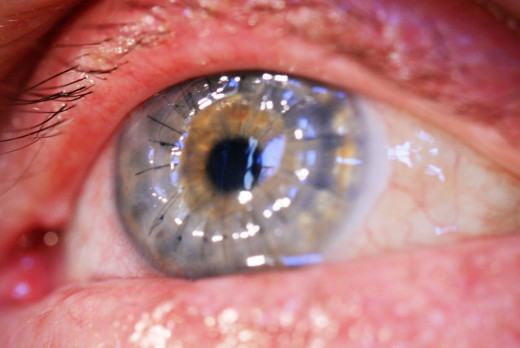
In a traditional full-thickness corneal transplant, a surgeon uses a surgical tool called a trephine. A trephine is something like a small cookie cutter. The diseased portion of the cornea is cut and replaced with a corresponding "replacement" piece from donated healthy cornea tissue. The incision is then sutured with a monofilament nylon which is one-third the thickness of a human hair. The entire procedure is done under a microscope. Different suturing techniques are used depending on the physician from a running stitch to 16 individual stitches all obtaining similar results.
The cornea has no blood supply and heals slowly so the stitches can be left in up to three years and in some cases permanently if the vision is good. Some people report feeling a scratching sensation when they blink. Other people find it somewhat painful particularly if one of the stitches breaks and pokes the eyelid when blinking. Great care must be taken to avoid rubbing the eye to keep from disturbing the stitches.
Internal suturing requires great skill and outcomes for patients can vary depending upon the performance of the surgeon. Now stitches may be a thing of the past. Israeli Professor Abraham Katzir of Tel Aviv's School of Physics and Astronomy has developed a way to seal incisions with temperature controlled laser bonding. Optical fibers made of silver halides deliver a laser beam that heats spots on the incision creating a strong bond without thermal damage. Wide testing was has been completed on deceased pigs and cows with no signs of leaks or overheating detected. Testing is now underway on live animals with the hope of clinical trials for humans sometime in the near future.
The applications of laser suturing are thought to be endless. Professor Katzir believes that this technique could have many applications. This technique has also been tried on skin wounds which healed well with virtually no scar. Naturally, plastic surgeons are watching with great interest. It is also hoped that this technique can be used in ear, nose and throat procedures, urology, other endoscopic and robotic procedures and possibly even on the brain.
Why Is This Important?
Loose stitches are the most common factor in developing a bacterial infection. As the graft wound heals, the stitches can become loose or break leading to erosion of the corneal epithelium. The corneal epithelium acts as a barrier which keeps out matter and destroying it allows bacteria into the cornea where it can cause infection. Loose stitches can also promote the growth of blood vessels which can promote graft rejection.
Infections in the cornea, while not life threatening, are a serious medical condition and will lead to the loss of the eye. If the donor cornea is rejected, another procedure can be performed but the chances of success decrease. So the development of a technique that can "instantaneously" create a strong bond without scarring will be life-changing for transplant patients.
Who Can This Help?
Cornea disease is the 4th most common cause of blindness with cataracts, glaucoma and age-related macular degeneration being the top three. Almost 10 million people suffer one of these condition across the world with 50,000 transplants being performed each year in the United States.
Conditions affecting the cornea which can lead to a transplant are:
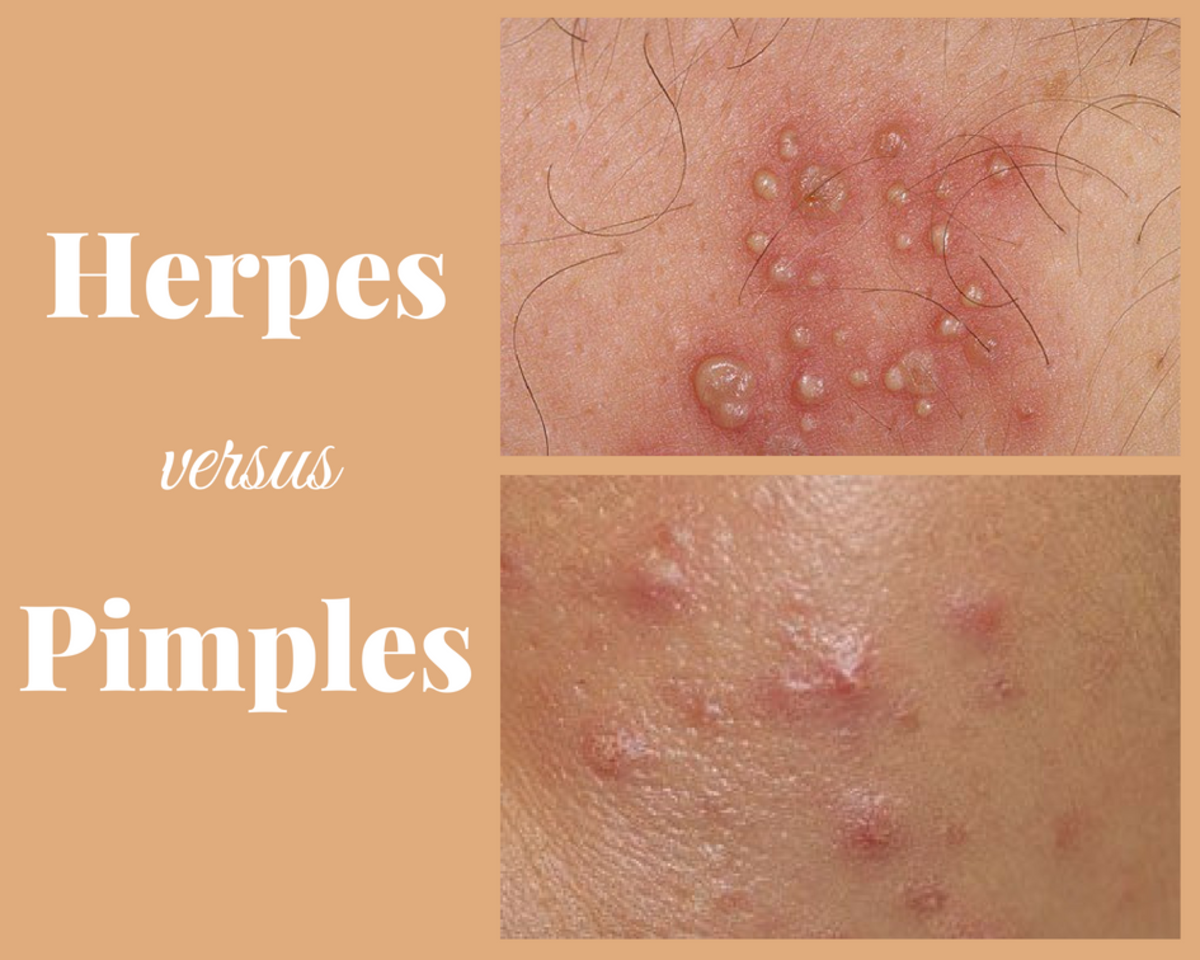
- Scarring from infections such as herpes in the eye or fungal keratitis.
- Scarring from trichiasis, a condition where the eyelashes grow inward toward the eye and rub against the cornea.
- Fuchs Dystrophy, where the innermost layer of the eye undergoes degenerative changes leading to vision loss.
- Kerataconus, a condition where the cornea weakens and bows into the shape of a volcano.
- Complications of LASIK.
- Chemical burns or damage from an eye injury.
- Complications of cataract surgery.




One Patient's Journey
On February 6, 2015, my son was diagnosed with kerataconus, a weakening and bowing of the cornea. In his case, he had become blind in his left eye and the only available treatment was a corneal transplant. Complicating his situation was the fact that he also has autism. .
We knew from our research that once the transplant is completed the eye is a very delicate position. One hard bump to the eye due to an accidental fall or a hit in the head during contact sports can result in the eye rupturing and loss of the eye. Even something as simple as rubbing the eye vigorously can rupture it. So when he was turned down for a transplant at both Northwestern Memorial Hospital and Rush in Chicago, who felt he may rub his eye and effectively lose it to trauma or infection, we were devastated. Our primary physician encouraged us to get a second opinion and we left for Mayo Clinic hoping for the best.
Our first appointment at Mayo lasted 5 and a half hours. He was tested extensively and we were exhausted. They were very kind and very thorough and we felt confident he was in good hands. Not only did they feel he could handle the transplant procedure but they also fitted him for a contact lens in the right eye which neither Northwestern nor Rush would do. Due to the severity of the condition of his left eye, we scheduled his surgery for September, 2015.
While the stress and worry was intense, the procedure and post operative care turned out to be relatively easy. The night before your procedure you wash your face and put an antibiotic eye drop in the affected eye. You repeat this procedure in the morning before your surgery. Because he has autism they were concerned he wouldn't be able to sit still for the procedure so he was given a general anesthetic. The procedure took about 2 hours and the pain following it was minimal. Antibiotic eye drops and steroid drops are given four times per day which he had no problem with.
I am not a medical professional and would not profess to give medical advice. However, if you do know someone with a handicapping condition who is facing the decision we were, I would highly recommend you seek a second opinion if you are turned down for the procedure. Our fears of what could happen were not even close to reality and he has done very well. There will be about 8 office more office visits during the course of the year and it can take up to one year for the blurriness in the eye to clear.
If you find yourself in a similar situation, where your loved one desperately needs a procedure which he or she has been turned down for due to a disabling condition, get a second opinion. We are so glad we did and would encourage anyone to go to Mayo Clinic if you can. Their reputation is well deserved.
Are you willing to be an organ donor after your death?
Are You Signed Up To Be A Donor?
No article involving transplants can end without a word of thanks to the donor whose parting gift restored my son's sight. Another family's tragedy saved my son's vision and while we rejoice in restored sight we grieve for someone we don't even know. So whoever you are, thank you. We intend to pay it forward.
Not only are we all signed up to be organ donors, we hope you will too. So here are a few things to think about to help you decide to give the gift of sight.
- Donors can be any age. Most are between the age of 2 and 70 and if a recipient cannot be found, the corneas will be used for education or research.
- Donation does not affect the medical treatment you receive at the end of your life.
- Donation doesn't affect your appearance if you wish to have an open casket at your funeral.
- There is no cost to you.
- People with cataracts or poor sight can still donate their corneas.
If you're still unsure watch Cassandra's story. And thank you.
© 2015 Chantelle Porter