Klebsiella Pneumoniae Infections : Clinical And Health Relevance of Pseudomonas Infection Manifestations
Freidlander’s bacillus Infecting Pneumonia

Klebsiella Pneumoniae Infections
Species of Klebsiella are capsulated Gram negative bacilli found normally in the throat and intestinal flora. Klebsiella pneumonia (Freidlander’s bacillus) is a virulent organism which produces pneumonia in compromised hosts. There are different serotypes of Klebsiella and they are grouped according to the capsular antigens.
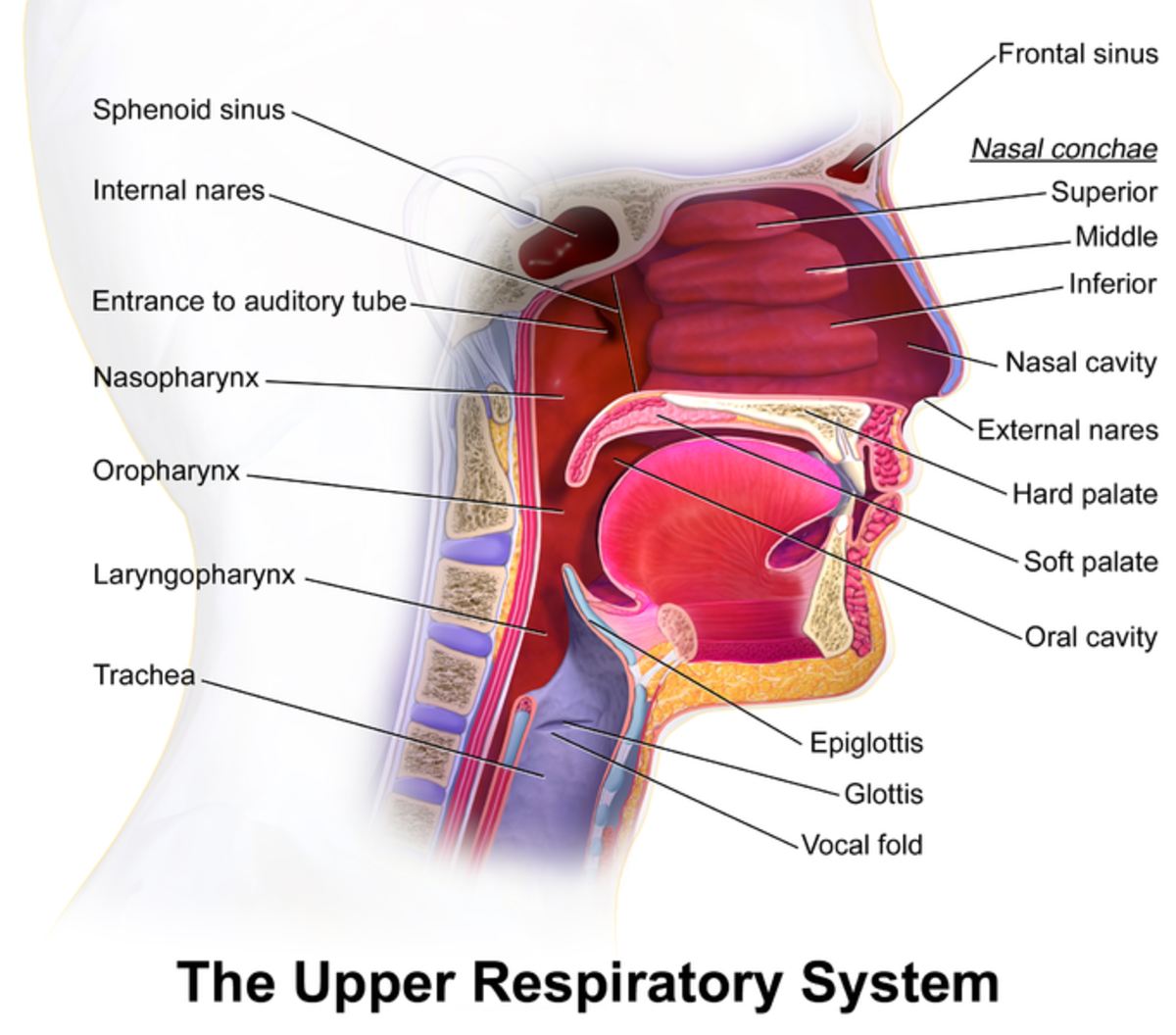
Pathogenesis: Klebsiella produces a wide variety of infections, the commonest being respiratory tract infections. Others are urinary tract infection, otitis media, mastoiditis, paranasal sinusitis and meningitis.
Pneumonia: Freidlander’s pneumonia usually occurs in diabetics and alcoholics. It could be acquired either from the hospital or from outside.
Treatment: In view of the severity of the infection, a combination of antibiotics is given. Gentamicin and cephalosporin or gentamicin and chloramphenicol are the preferable combinations. The treatment should be continued for 10 to 14 days or more.
Hospitalized Patient Of Pseudomonas Pneumonia

Infectious Diseases
Pseudomonas Infection
Pseudomonas aeruginosa is a Gram-negative bacillus which produces a characteristic greenish pigment called pyocyanin. The organism may be present in the skin surface of normal people. In subjects receiving antibiotic therapy in hospitals, this organism can be isolated from the sputum, superficial wounds, burns and many other sites. It is only rare to be the primary pathogen. Immunocompromised hosts are readily infected. The organism enters through abrasions in the skin or through the urinary, respiratory or gastrointestinal tract. In addition to local lesions in these sites, hematogenous spread may occur resulting in the development of hemorrhagic nodules and thrombosis of blood vessels.
Pneumonia: Pseudomonas pneumonia seen in hospitalized persons, receiving antibiotic therapy. Colonisation of the throat by the organism and aspiration into the respiratory tract are responsible for the lesion. Both lungs show microabscesses.
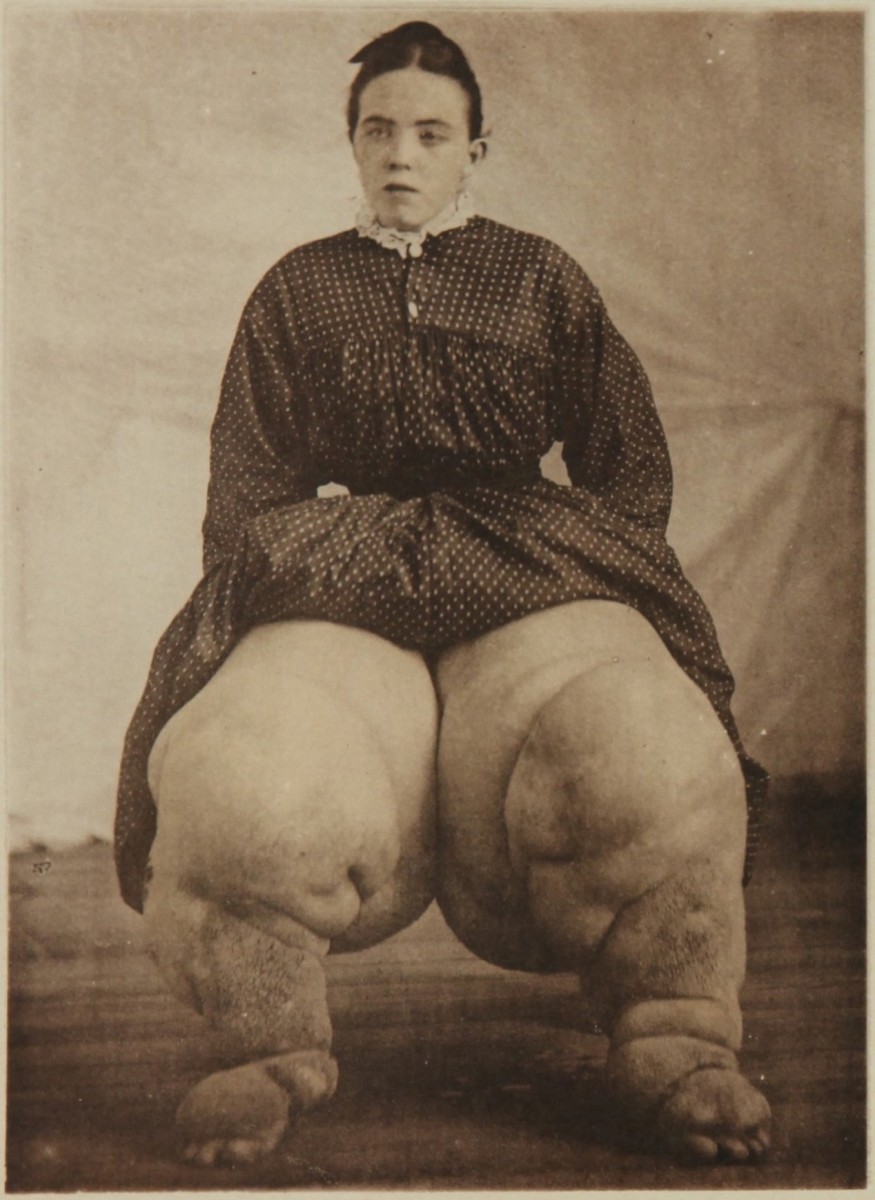
Skin lesions: Wounds, ulcers, burns and other superficial lesions are secondarily infected to produce mild lesions. Bacteremic spread leads to ecthyma gangrenosum which appears as indurated purple black areas about 1cm in diameter with ulcerated centers. Other manifestations include hemorrhagic cellulitis and macular lesions.
Other superficial infections: Pseudomonas is a common secondary invader in patients having indwelling catheters and obstructive uropathies. External otitis, mastoiditis, paranasal sinusitis, perirectal abscess and infantile diarrhea may develop in susceptible individuals.
Systemic infection: Primary bacteremia occurs in patients with burns and in leukemic subjects. Septicemia and endotoxic shock may develop in them. Pseudomonas aeruginosa causes bacterial endocarditis especially after cardiac surgery and burns and in drug addicts. Mortality in pseudomonas bacteremia ranges from 50 to 70%. Meningitis may result from bacteremia or it may follow lumbar puncture done in hospitals.
Treatment: Superficial infections respond to local cleaning and topical application of polymyxin B. Systemic infection is treated with a combination of gentamicin and carbenicillin which act synergistically against the organism. The dose of gentamicin is 3 to 5 mg/Kg/day in three divided doses and that of carbenicillin is 400 mg/Kg/day in four equal doses. Resistant strains can be treated with amikacin which is resistant to bacterial inactivation. It is given intravenously 6 to 10 mg/Kg/day in 2 divided doses. An alternative is systemic polymyxin in which has to be given in a dose of 500,000 units every 8 hours intramuscularly.
Prophylaxis: Since Pseudomonas is a common cause of nosocomial infections, utmost care should be taken to prevent cross infection by following good personal hygiene and strictly aseptic techniques. Prudent use of antibiotics helps to minimize colonization by Pseudomonas aeruginosa. Systemic antibiotic prophylaxis does not prevent pseudomonas infection. A vaccine has been used in a limited scale to prevent infection in high risk patients.
© 2014 Funom Theophilus Makama