Leptospirosis: Epidemiology, Pathology, Clinical Manifestations, Diagnosis, Treatment And Prevention
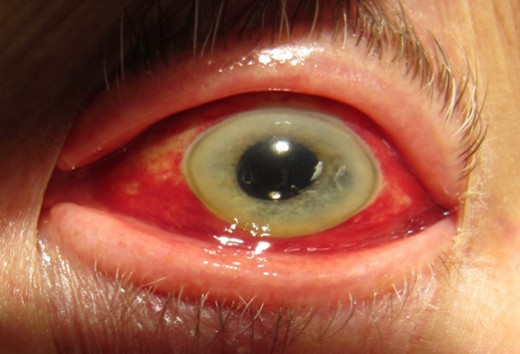
The Eye presentation In leptospirosis
Epidemiology And Pathology Of Leptospirosis
Leptospirae cause serious disease in man in different regions. Among the several serotypes, only Leptospirae icterohaemorrhagiae, L. canicola, L. Pomona, L. hebdomadis and L. autumnalis are harmful to man. Most of the leptospirae are primary parasites of domestic and wild animals by occupational exposure. Though leptospiosis used to be described under different synonyms depending on the organism and the clinical manifestation, it is now clear that considerable overlap occurs among them and therefore they are all described together.
Epidemiology: Leptospirae are eliminated in the urine of their animal hosts, which harbor the organisms in the renal tubules. Man gets infected by coming into contact with the infected urine during occupational or recreational activities. Rats, several varieties of other rodents, dogs, pigs and other animals harbor the organisms. Miners, sewer workers, butchers and veterinary surgeons are exposed to the risk occupationally. Other sources of infection are swimming pools and tanks.
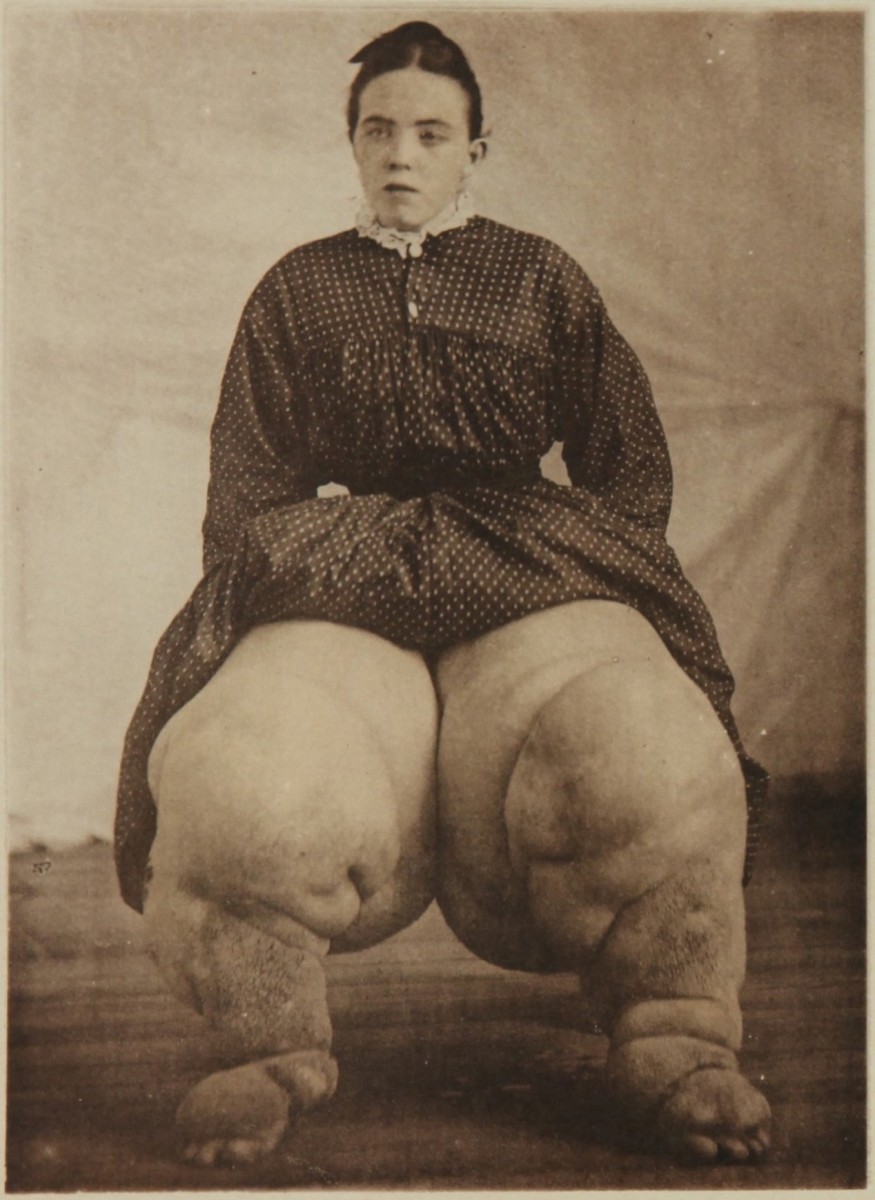
Pathology and pathogenesis: The organisms enter by penetrating the skin and mucous membranes. The disease is characterized by generalized endothelial damage. Major lesions are seen in the liver, Kidneys, brain, meninges, muscles and skin. In the early stages, the direct invasion by the parasites causes the damage, but in the later stages, immunological processes also play a part. In the early phase parasites are seen in tissue and secretions. They disappear in the later phases. At autopsy, the demonstrable lesions include renal tubular necrosis, presence of granular and myoglobin casts in the renal tubules, centriolobular of massive necrosis of liver cells with biliary stasis, and petechial hemorrhages in cardiac and skeletal muscles.
Vasculitis In leptospirosis

Infectious Diseases
Clinical Manafestations And Treatment Of leptospirosis
Average incubation period is 10 days, but this may range from 4 to 21 days. The vast majority of infected persons do not develop the clinical disease, which occurs only in 5 to 10%. Onset is that of a flu-like illness with fever, headache, malaise, prostration and muscle pains, In anicteric cases, these may be the only manifestations.
In those cases that develop the classical diseases, after 4 to 7 days of nonspecific illness, the fever subsides temporarily to recur later. During this second phase, immunologic disturbances predominate. Clinical features include jaundice, renal failure, menigeal irritation, petechail hemorrhages from skin and mucosa and myocarditis in some cases. The deep jaundice is out of proportion to the degree of parenchymal liver cell damage, as assessed by liver enzymes. Liver is enlarged in 25% of cases. Most of the cases show severe and characteristic myalgia, especially of neck and back muscles. Myocarditis may give rise to arrhythmias, cardiomegaly or cardiac failure. Hepatorenal lesions predominate in L. icterohemorragiae infections (Weil’s disease). Pretibila skin lesions are often seen in infection with L. autumnalis (Fort-Bragg fever). Leptospira canicola is noted for production of meningeal irritation and conjunctival congestion (Canicola fever). Prlonged uveitis is seen in some cases. Mortality in leptospirosis ranges from 10 to 15%.
Diagnosis: Clinically, the diagnosis should be suspected when sporadic or small outbreaks of jaundice occur, associated with severe myalgia, hemorrhagic manifestations and neutrophil leucocytosis.
Treatment: Leptospirae are sensitive to penicillin and tetracycline. Benzyl penicillin 2.4 or tetracycline eliminates the organisms from the renal tubules, it is preferred by many. Administration of antibiotics late in the disease is not of much benefit. When hepatic, renal, cardiac or hemorrhagic manifestations predominate, therapy is directed towards them.
Prevention: Leptospirosis can be prevented by avoidance of infection from animal sources, personal hygiene and disinfection of infected water sources.
© 2014 Funom Theophilus Makama