Meningitis – Prophylaxis and Cure
Definition
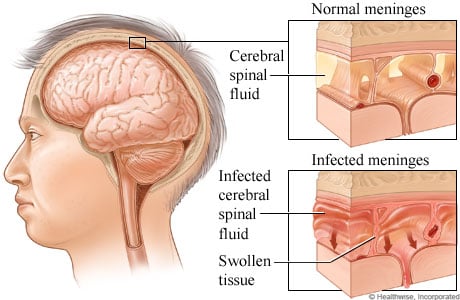
The World Health Organization (WHO) defines meningitis as an infection of the central nervous system affecting the meninges (i.e. thin protective membranes) of the brain and spinal cord. The meningeal infection results in the inflammation of cerebral and spinal meninges and is often caused by bacterial, viral, or fungal pathogens that may result in mild to severe complications resulting in variable morbidity and mortality in accordance with the virulence of the invading pathogen. Meningitis may also progress as a severe manifestation of subarachnoid hemorrhage, cancers, or chemical irritation.
Incidence
Five to ten cases of bacterial meningitis in 100,000 individuals are reported in the United States every year, with a death toll of more than 2000, majorly affecting children below five years of age. Bacterial meningitis in neonates is the result of Listeria monocytogenes, Escherichia coli, or Group B Streptococcus infestation. Haemophilus influenzae type b primarily causes meningitis in infants. However, the disease extends its roots in adolescents and adults through the pathogens like Neisseria meningitidis, Streptococcus pneumonia, and Listeria monocytogenes.
Classification
Types of Meningitis
| Causative Organism(s)/Etiology
| Expected Outcome
|
|---|---|---|
Viral (Aseptic) Meningitis
| Enteroviruses, mumps virus, lymphocytic choriomeningitis (LCM) virus
| Mild and benign illness develops in 0.1% of the infected individuals
|
Bacterial Meningitis
| Streptococcus pneumonia, Neisseria meningitides, Hemophilus influenza, Listeria monocytogenes, Streptococcus agalactiae (group B), Escherichia coli, Gram–negative bacilli (other than E coli), Staphylococcus aureus and Staphylococcus epidermidis
| Communicable and contagious illness transmitted through coughing and sneezing of the infected individuals. The disease progresses rapidly leading to serious medical emergencies and high fatality rates
|
Fungal Meningitis
| Cryptococcus neoformans and Candida albicans
| This type of meningitis develops in 10% of immunocompromised patients affected with AIDS, lupus and diabetes
|
Parasitic Meningitis (Primary amoebic meningoencephalitis)
| Microscopic amoeba (Naegleria fowleri)
| The progression of the disease results in the destruction of brain tissue leading to ataxia and hallucinations. Mortality results within 1 to 12 days from the onset of disease
|
Non-infectious meningitis
| The disease emanates as a manifestation of severe illnesses like cancers, lupus, head injury, mumps, tuberculosis, syphilis, birth defect, brain surgery and drugs (including Ergamisole and rubella vaccines)
| Photophobia (i.e. sensitivity to light) and Altered Mental Status
|
Signs and Symptoms
The most common symptoms of acute meningitis are sudden onset of high-grade fever, headache, neck pain, and vomiting. The clinical features of this dread disease include reflex spasm of the spinal nerves resulting in a positive Kernig sign (i.e. difficulty to straighten the raised leg due to pain) and neck stiffness on the patient’s physical examination. The neck stiffness further results in Brudzinski's sign, which causes the flexion of the patient's hips and knees with the proportionate induced flexion of the neck. Other symptoms include intolerance towards loud sounds (phonophobia) and difficulty in coordination. Bacterial meningitis is a life-threatening condition with more than 80% fatality rate of the infected untreated individuals. The condition results in a characteristic rash that is not apparent in the patients with viral meningitis. However, the surviving patients may experience learning disabilities and hearing loss due to brain damage by the bacterial species.
Transmission and Routes of Infection
The pathogen primarily infects a patient’s respiratory tract, intestine, or skin and its appendages. The complicated middle ear and paranasal sinuses infections of childhood have the scope of transmission to cerebral meninges, thereby resulting in dread meningeal complications. The invading bacterial pathogens of meningitis are transmitted through the exchange of respiratory (oral) secretions by direct close contact with the diseased patient.
Predisposing Factors
The risk factors of meningeal infections vary with age, community setting, travel, and exposure to the disease-causing organisms. Different types of meningeal pathogens become the cause of infection in various age groups. However, infants' risk for capturing bacterial meningitis is comparatively higher as compared to other age groups in the same geographical location. Similarly, people residing in larger groups have an increased risk of the occurrence of the disease. Traveling to regions of meningeal epidemics increases the risk of transmission of disease pathogen to the travelers. Scientists engaged in studying the meningeal pathogens get prone to become the victim of this communicable illness.
Prophylaxis
The people living in close contact with the infected individuals need to undergo antibiotic therapy to decrease the risk of the contagious infection. Vaccination is recommended for children against meningitis pathogens including, Neisseria meningitides (meningococcus), Streptococcus pneumoniae (pneumococcus), and Haemophilus influenzae type b (Hib). Persons with immunocompromised states are required to stringently follow hygiene and practice precautions like avoiding contact with the infected patients. Polysaccharide and meningococcal conjugate vaccines need the administration to control the infection in elderly people. Susceptible people with congenital or acquired absence of spleen need prophylactic treatment with antibiotics or administration of the pneumococcal vaccine to reduce the probability of pneumococcal infection.
Pathogenesis
The infection begins with the accumulation of live bacteria in the nasopharyngeal mucosa and extends further resulting in high-grade bacteremia. The invading pathogen acquires resistance by obstructing neutrophils phagocytosis and complement-mediated bactericidal activity. The bacteria then attack the central nervous system and induce inflammatory cytokines to make the blood-brain barrier more permeable and open the passage for the transfer of neutrophils and proteins to the subarachnoid space. With the movement of inflammatory mediators to the subarachnoid space, manifestations like cerebral edema and increased intracranial pressure further complicate the patients’ clinical condition.
Diagnosis
The clinical diagnosis follows the lab testing performed to confirm the suspected cause of meningeal infection. The following lab investigations help acquire a definitive diagnosis after clinical correlation with the test findings.
1. Cerebrospinal fluid (CSF) analysis (by lumbar puncture or spinal tap)
2. PCR (Polymerase Chain Reaction) Essays
3. Blood Cultures
4. Procalcitonin Analysis
5. CBC and Blood Glucose Tests
6. Comprehensive Metabolic Panel
7. CT (Computed Tomography)
8. Ultrasound
9. EEG (Electroencephalography)
10. MRI (Magnetic Resonance Imaging)
Treatment
The treatment of bacterial Meningitis requires hospital admission and controlled with the intravenous administration of antibiotics like ceftriaxone, ampicillin, vancomycin, and dexamethasone.
Apart from the antibiotic treatment regimen, oxygen therapy, administration of steroids and IV fluids, and antiviral drugs antagonize clinical manifestations of cerebral edema in meningitis.
Viral meningitis is comparatively a less severe condition and recovery is possible within a span of 10 to 14 days by the symptomatic treatment with painkillers and anti-emetics (to overcome the integral symptoms of headache and vomiting).
There is no direct herbal remedy to cure meningitis; however, the use of natural supplements with the prescribed medication helps the body to recover from this dread disease in a comparatively shorter time span. These natural supplements include Garlic, Olive leaf extracts, Zell oxygen plus (yeast preparation), Colloidal silver, American Ginseng, and Chlorella. The practitioners of integrative medicine recommend these natural herbs (along with the standard therapy) in alleviating the complications of meningitis due to their bactericidal, antiviral, disinfectant, anti-inflammatory, and antiseptic properties. Herbs like garlic, ginseng, and olive leaves contain trace elements, enzymes, essential nutrients, antioxidants, amino acids, and vitamins that enhance the immunity of the affected individuals against the invading pathogen.
The physicians at the University of Maryland Medical Center claim that species (Uncaria guianensis and Uncaria tomentosa) of the cat’s claw plant are effective in treating the clinical manifestations of meningitis, due to their anti-inflammatory properties. However, clinical trials are required to warrant the use of this American herb in medical prescriptions.